Intolerance of Uncertainty Mediates the Influence of Viral Anxiety on Social Distancing Phobia Among the General Korean Population During the Coronavirus Disease 2019 Pandemic
Article information
Abstract
Objective
We aimed to examined the reliability and validity of Korean version of Social Distancing Phobia scale, and whether intolerance of uncertainty mediates the association of the general population’s social distancing phobia with viral anxiety and depression.
Methods
Through this anonymous online survey, we collected responses from 400 individuals in the general Korean population. Participants’ demographic information and rating scales scores, including the Social Distancing Phobia scale, Stress and Anxiety to Viral Epidemics-6 items, Patient Health Questionnaire-9, and Intolerance of Uncertainty-12 items.
Results
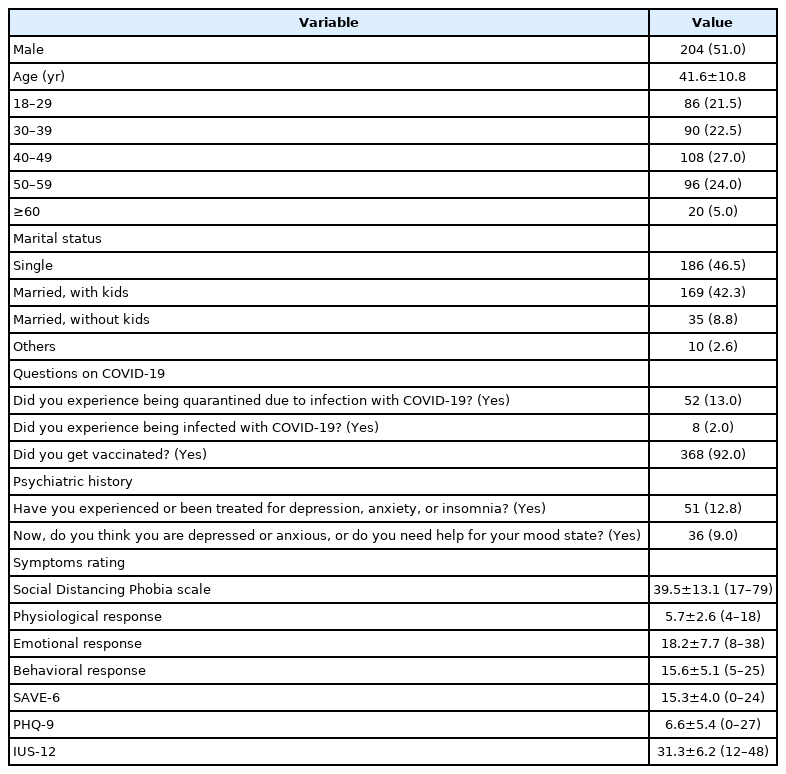
Confirmatory factor analysis showed a good model fit, and the Korean version of Social Distancing Phobia scale showed good internal consistency. Social distancing phobia was significantly correlated with age (r=0.213, p<0.001), viral anxiety (r=0.390, p<0.001), depression (r=0.244, p<0.001), and intolerance of uncertainty (r=0.323, p<0.001). A linear regression analysis showed that age (β=0.235, p<0.001), viral anxiety (β=0.281, p<0.001), depression (β=0.121, p=0.009), and intolerance of uncertainty (β=0.200, p<0.001; adjusted R2=0.246, F=33.6, p<0.001) predicted social distancing phobia. Mediation analysis revealed that viral anxiety directly influenced social distancing phobia (z=6.48, p<0.001), and intolerance of uncertainty partially mediated this association (z=2.92, p=0.003).
Conclusion
Social distancing phobia may cause psychological stress but may also increase adherence to physical distancing measures and prevent the spread of viruses.
INTRODUCTION
Since the first outbreak of the novel coronavirus disease (COVID-19) in Wuhan, China, over 300 million people have been diagnosed with the virus as of January 2022 [1]. Countries worldwide adopted various quarantine measures, including social distancing guidelines, and made efforts to provide people with newly developed vaccines. However, several viral variants emerged worldwide, making it even more difficult to terminate the pandemic. The pandemic caused negative effects on various aspects of the global society, and psychological stress was one of them. According to a study conducted in the United Kingdom, over 1/4 of survey participants reported of having general psychiatric disorders, and over 1/3 reported of feeling loneliness during the COVID-19 pandemic [2]. Furthermore, a longitudinal study done among the general population in China showed that 28.8% and 16.5% of participants suffered from moderate to severe anxiety and depressive symptoms, respectively [3].
Social distancing phobia during the COVID-19 pandemic
Pandemics seen over past decades have had negative effects on individuals’ mental health and have led to worry, anxiety, and fear [4]. Experts emphasize that social distance and hygiene rules should be observed for protection against the coronavirus [5]. It is stated that transmission is easier with situations such as sneezing and coughing, especially by someone who is asymptomatic [6]. Additionally, the high rate of morbidity and mortality of the pandemic due to new viral variants is effective in imparting more intense stress and fear. In fact, this may cause individuals to develop a phobia of COVID-19 [4]. On the other hand, one of the reasons for the phobic situation experienced by individuals is the “social distance rule” that should be followed to reduce the risk of transmission of COVID-19. It is observed that individuals’ reactions are similar to the previously mentioned phobic situations in the literature [7]. Further, it is a more appropriate conceptualization to express social distancing phobia due to this rule that individuals must comply with against the risk of virus transmission [8,9].
Phobias manifest as unusual fears of particular objects or situations [10]. For the fear developed against a situation or object to be defined as a phobia, it must be different and longer lasting than usual and temporary fear. Additionally, disproportionate fear and anxiety in the face of a situation are sufficient to define a phobia [11]. In the current pandemic, individuals cannot prevent the thought and fear that the virus can be transmitted from others they encounter [12]. This situation reduces individuals’ functionality and psychological well-being [13]. In a study by GÜNLÜ [8], it was determined that individuals’ efforts to pay maximum attention to social distancing in the COVID-19 pandemic were effective in the development of new phobic tendencies. Social distancing phobia is the occurrence of phobic symptoms, which occurs because of paying attention to social distancing rules to the maximum extent to protect oneself from viral transmission, causing the individual to experience excessive stress, tension, and anxiety [9]. Additionally, “sodisphobia” is a term suggested by Günlü as an abbreviation for social distancing phobia. In the study, the participants stated that they felt extremely stressed and nervous when shopping or in the presence of other people. It has been determined that this process gets out of control and impairs an individual’s functionality. Subsequently, a literature review was conducted, and no scale that can measure individuals’ social distancing phobia was found.
Intolerance of uncertainty, viral anxiety, and physical distancing
Several aspects of life are associated with unexpected and ambiguous factors. This may be considered unpleasant or even unacceptable for some people, which leads to intolerance of uncertainty (IU) [14]. This term is defined as ‘the excessive tendency of an individual to consider it unacceptable that a negative event may occur, however small the probability of its occurrence [15]. Since the COVID-19 pandemic caused various unpredictable changes related to health, economic, social, and psychological factors, it was hypothesized that IU might also play a role in various psychological aspects related to the pandemic [16,17].
In the COVID era, each country adopted social distancing as a way to decrease the spread of COVID-19 among the general population. Whether individuals adhere well to social distancing measures has been considered one of the most important factors in deciding the success of COVID-19 prevention [18]. There is ongoing research as to which factors dictate adherence to social distancing guidelines, and IU is one of them. It can be assumed that those with high IU generally are more worried about the virus’s unpredictable and perhaps catastrophic consequences, which may lead to better adherence to social distancing. However, several studies showed no significant relationship between IU and adherence to social distancing.
In this COVID-19 pandemic, viral anxiety might also be an important factor governing adherence to physical distancing rules since it can influence an individual’s physical distancing behavior [19]. Recently, it was reported that anxious people are more likely to adhere to physical distancing policies [9,20]. Social distancing phobia, referring to the excessive anxiety of viral infection while being in public, is speculated to be associated with viral anxiety, though this association has not been well demonstrated yet. We observed that nursing students’ adherence to physical distancing was associated with their viral anxiety measured with a viral epidemic-specific rating scale (Stress and Anxiety to Viral Epidemics-6 items [SAVE-6] [21]) [22]. Additionally, among healthcare workers, we also observed similar results [23]. We can speculate that an individual’s elevated social distancing phobia may be related to their adherence to physical distancing, and we can hypothesize that viral anxiety might be associated with social distancing phobia among the general population.
This study aimed first to explore the reliability of validity of the Korean version of the Social Distancing Phobia scale among the general population in South Korea. Second, we aimed to examine the association of social distancing phobia of the general population with viral anxiety and depression. Third, we explored whether the IU mediates the influence of depression or viral anxiety on social distancing phobia.
METHODS
Participants and procedures
This anonymous online survey was performed among the general Korean population via a professional survey company, EMBRAIN (www.embrain.com), from the 10th to the 18th of January 2022. All 400 general population participated in this survey, and we collected participants’ information regarding age, sex, region of residence, and marital status. We asked questions regarding COVID-19, including “Did you experience being quarantined due to infection with COVID-19?” “Did you experience being infected with COVID-19?” and “Did you get vaccinated?” Participants’ past psychiatric history and current psychiatric distress were evaluated. The survey form was developed according to the Checklist for Reporting Results of Internet e-Surveys guidelines [24]. Furthermore, investigators (S.C. and IK.C.) checked the survey form’s usability and technical functionality before implementation. The study protocol was approved by the Institutional Review Board (IRB) of the Asan Medical Center (2021-1755), and the need for obtaining written informed consent was waived by the IRB.
The sample estimation was done based on the allocation of 40 samples for 10 cells (biological sex×five age groups) [25], and all 400 participants were selected from among the 14,000,000 individuals in the general population panels of the survey company. The company sent enrollment emails to 2,000–3,000 panelists, and 949 participants accessed the survey. All 400 responses were collected, and the company delivered the collected data after excluding all identifiable personal information.
Measures
Social Distancing Phobia scale
The scale is a tool developed by Gunlu [9] to measure individuals’ social distancing phobia, especially during the pandemic era. This scale aims to assess social distancing phobia levels. The Social Distancing Phobia scale is a self-report instrument with a 5-point Likert-type scale. There is no reverse-scored item on the scale. The total score ranges from 17–85 points. In addition to the scale’s total score, the scores obtained from factors vary between 4–20 points for physiological responses, 8–40 for emotional responses, and 5–25 for behavioral responses. Higher scores indicated greater social distancing phobia on the respectable factors and the total scale. Cronbach’s alpha reliability was calculated as 0.93 for the scale’s total score, 0.90 for the physiological response, 0.88 for the emotional response, and 0.86 for the behavioral response. High scores obtained from the Social Distancing Phobia scale indicate that the individual has a high level of social distancing phobia.
In this study, we translated the Korean version of the Social Distancing Scale using a translation and back-translation method. A bilingual expert translated the English version of the Social Distancing Phobia scale into the Korean version. Then another expert back-translated Korean versions into the English version without referring to the original English version of the scale. Lastly, a third party compared the original English and translated English versions to check for any discrepancy in meaning. After the process, the final Korean version of the scale was developed.
Stress and Anxiety to Viral Epidemics-6 items
The SAVE-6 scale is a self-report rating scale developed to assess one’s viral anxiety during the COVID-19 pandemic [21]. It was derived from the original SAVE-9 scale developed to measure healthcare workers’ work-related stress and anxiety response to the viral epidemic [26]. The SAVE-6 consists of six items rated on a 5-point Likert scale from 0 (never) to 4 (always). A higher total score, ranging from 0–24, reflects high levels of viral anxiety. The SAVE-6 scale was originally developed in the Korean language. Cronbach’s alpha was 0.789 in this sample.
Patient Health Questionnaire-9
The Patient Health Questionnaire-9 (PHQ-9) is a self-rating scale developed to assess the severity of depression [27]. It consists of 9 items that can be rated on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). We applied the Korean version of PHQ-9 in this study [28]. Cronbach’s alpha in this sample was 0.890.
Intolerance of Uncertainty-12 items
The Intolerance of Uncertainty-12 items (IUS-12) is a shortened version of the IUS [29] developed to assess one’s IU. It consists of 12 items rated on the type of agreement (1–7). A higher total score reflects a higher IU. In this study, we applied the Korean version of the IUS-12 scale [30] and Cronbach’s alpha among this sample was 0.905.
Statistical analysis
In the first step, we explored the validity and reliability of the Korean version of the Social Distancing Phobia scale. Sampling adequacy and data suitability for the factor analyses were checked based on Kaiser-Meyer-Olkin (KMO) value and Bartlett’s test of sphericity. Factor structure was explored using both exploratory factor analysis (EFA) (estimation method: maximum likelihood) following parallel analysis (using reduced correlation matrix), and confirmatory factor analysis (CFA) [estimation method: diagonally weighted least squares (DWLS)]. In parallel analysis, the total number of factors were determined through the number of factors having reduced eigenvalue 1 or above. In EFA, variance explained by factors and factor loadings of items were estimated. In CFA, satisfactory model fit was defined by a standardized root-mean-square residual (SRMR) value ≤0.05, root-mean-square-error of approximation (RMSEA) value ≤0.10, and comparative fit index (CFI) and Tucker Lewis index (TLI) values ≥0.90 [31,32]. A series of multi-group CFA was conducted to examine whether the Korean version of the Social Distancing Phobia scale can assess the social distancing phobia in a same way across sex, having viral anxiety (SAVE-6 ≥15), and having depression (PHQ-9 ≥10). Psychometric properties of the Korean version of the Social Distancing Phobia scale were also assessed through the Rasch model. In the Rasch model, infit mean square (infit MnSQ), outfit MnSQ, item difficulty, item and person separation index, and item and person reliability were estimated. Differential item functioning (DIF) bias across sex and having depression (PHQ-9 ≥10) estimated Mantel–Haenszel χ2. Internal consistency reliability was tested based on Cronbach’s alpha, McDonald’s omega, and split-half reliability.
In the second step, we examined the association of the Korean version of Social Distancing Phobia scale with various psychological factors such as viral anxiety, depression, IU or belongingness using the Pearson’s correlation coefficients. Linear regression analysis was conducted to explore the factors predicting the social distancing phobia. The mediation analysis was done to examine the mediating effect of the IU on the association between psychological factors and social distancing phobia by implementing the bootstrap method with 2,000 resamples. The SPSS version 21.0 (IBM Co., Armonk, NY, USA) was used to conduct basic statistical analysis, RStudio (Boston, MA, USA) was used to conduct the factor analyses and Rasch model analysis, and AMOS version 27 (IBM Co.) and Jamovi 1.6.23 (Sydney, Australia) were used to conduct the mediation analysis.
RESULTS
The 400 participants were residents of Seoul (n=133, 33.3%), Pusan (n=21, 5.3%), Daegu (n=4, 1.0%), Incheon (n=23, 5.8%), Gwangju (n=6, 1.5%), Daejeon (n=10, 2.5%), Ulsan (n=7, 1.8%), Gyeonggi Province (n=136, 34.0%), Gangwon Province (n=4, 1.0%), Chungcheong Province (n=21, 5.3%), Jeolla Province (n=13, 3.3%), Gyeongsang Province (n=17, 4.3%), and Sejong (n=5, 1.3%). Further, 204 (51.0%) were male, 52 (13.0%) participants had been quarantined, 8 (2.0%) experienced COVID-19 infections, and 368 (92.0%) had been vaccinated. Fifty-one (12.8%) participants reported that they had experienced past psychiatric symptoms, and 36 (9.0%) reported current psychological distress (Table 1).
Validity and reliability of the Korean version of the Social Distancing Phobia scale
Factor analysis
The sample’s adequacy and data’s suitability were evaluated based on the KMO measure (0.91) and Bartlett’s test of sphericity (p<0.001). Outputs from the parallel analysis suggested three factors. EFA with oblimin rotation showed that the three factors model (physiological, emotional, and behavioral responses; Tables 2 and 3) explained 70.71% variance. Factor loadings are ranged between 0.556 and 0.916 for physiological response factor, 0.408 and 0.854 for emotional response factor, and 0.526 and 0.854 for behavioral response factor (Table 2). The CFA with the DWLS methods showed a good model fit (χ2/df=2.648, CFI=0.98, TLI=0.98, RMSEA=0.06, SRMR=0.08). The multi-group CFA, with configural, metric, scalar invariance, revealed that the Korean version of Social Distancing Phobia scale can measure the social distancing phobia in a same way across sex, having viral anxiety, and having depression (Supplementary Table 1 in the online-only Data Supplement).
Rasch model
Supplementary Table 2 (in the online-only Data Supplement) presents the Rasch model outputs of the Korean version of the Social Distancing Phobia scale. Itfit and mean squares of all the items are between the recommended range (0.50–1.50) except item 5 (emotional response subscale). In the physiological response subscale, item 2 is the least difficult item and item 3 is the most difficult item. In the emotional response subscale, item 5 is the least difficult item and item 11 is the most difficult item, and in the behavioral subscale, item 15 is the least difficult item and item 13 is the most difficult item. All the subscales have acceptable item and person separation index (≥2) and reliability (≥0.7). DIF results (Supplementary Table 3 in the online-only Data Supplement) shows absence of DIF bias (p<0.01) in items across sex and having depression (PHQ-9 ≥10).
Reliability and evidence based on relations to other variables
The Korean version of Social Distancing Phobia scale showed good internal consistency based on Cronbach’s alpha, McDonald’s omega, and split-half reliability value in each factor (Table 3). Corrected item-total correlations are between 0.691 and 0.808 in physiological response factor, 0.604 and 0.857 in emotional response factor, and 0.595 and 0.755 in behavioral response factor. The Social Distancing Phobia scale score was significantly correlated with the SAVE-6 score (r=0.390, p<0.001) and PHQ-9 score (r=0.244, p<0.001; Table 4). Physiological response factor score was significantly correlated with the SAVE-6 (r=0.276, p<0.001) and PHQ-9 (r=0.279, p<0.01), emotional response factor with the SAVE-6 (r=0.402, p<0.001) and PHQ-9 (r=0.266, p<0.001), and behavioral response factor with the SAVE-6 (r=0.245, p<0.001) and PHQ-9 (r=0.103, p=0.039).
Social distancing phobia, viral anxiety, depression, and intolerance of uncertainty
As shown in Table 4, the Social Distancing Phobia scale score was significantly correlated with age (r=0.213, p<0.001), viral anxiety (r=0.390, p<0.001), depression (r=0.244, p<0.001), and IU (r=0.323, p<0.001). All three factors of the Social Distancing Phobia scale were significantly correlated with viral anxiety (all, p<0.001), depression (all, p<0.001), and IU (all, p<0.001). Three factors were also significantly correlated with each other.
A linear regression analysis with enter methods, conducted to explore the variables predicting the social distancing phobia, showed that age (β=0.235, p<0.001), viral anxiety (β=0.281, p<0.001), depression (β=0.121, p=0.009), and IU (β=0.200, p<0.001; adjusted R2=0.246, F=33.6, p<0.001; Table 5) predicted social distancing phobia.
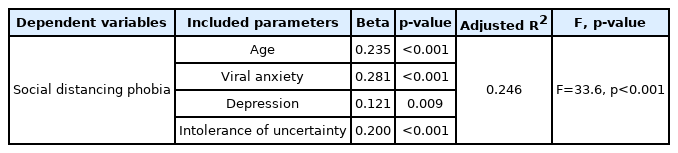
Linear regression analysis to explore the factors predicting social distancing phobia among the general population
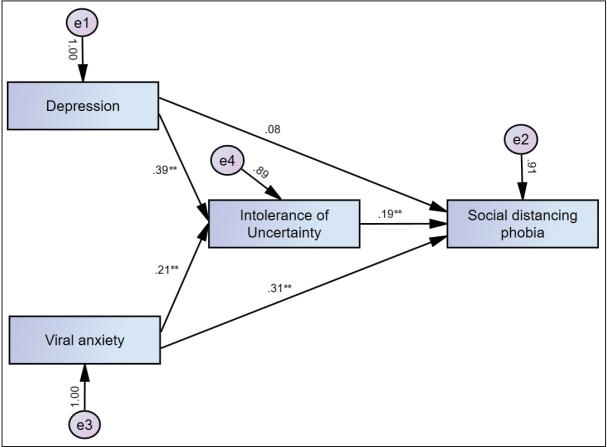
Mediation analysis (Table 6 and Figure 1) showed that viral anxiety directly influenced social distancing phobia (z=6.48, p<0.001), and IU partially mediated this association. Although depression did not directly influence social distancing phobia, IU totally mediated this association (z=3.42, p<0.001).
DISCUSSION
We observed that the Korean version of the Social Distancing Phobia scale was a valid and reliable tool for measuring individuals’ social distancing phobia in this COVID-19 pandemic. Additionally, social distancing phobia was predicted by age, viral anxiety, depression, and IU. Furthermore, IU partially mediated the influence of viral anxiety on social distancing phobia and completely mediated the influence of depression on social distancing phobia.
Validity and reliability of the Korean version of the Social Distancing Phobia scale
In the original study [9], items of the Social Distancing Phobia scale were clustered into three factors: physiological response (items 1–4), emotional response (items 5–12), and behavioral response (items 13–17). The physiological response factor aims to determine the individual’s level of physiological response, such as a change in heart rate and chest narrowing, in case of a decrease in social distance; higher scores indicate that the individual overreacts to reduced social distance. In other words, an excessive physiological response negatively affects the individual’s functionality. The emotional response factor aims to determine the individual’s emotional reactions, such as excitement, extreme stress, and fear, depending on their thoughts when they enter areas where social distance cannot be maintained (such as mixing with a crowd); higher scores indicate that, in cases of decreased social distance, the individual overreacts to the situation and is negatively affected by this process, thus negatively affecting their emotional health. The behavioral response factor determines the individual’s physical movements and actions taken to maintain social distance; high scores indicate that the individual makes excessive efforts to maintain social distance, thereby impairing their functionality.
In this study, we observed that items of the Korean version of the Social Distancing Phobia scale could be clustered well into three factors similar to the original study. The factor loading value (0.408) and a higher mean score (2.797±1.261) of item 5 of the emotional response factor (“When I go out, and someone I do not know coughs less than a meter away, I am afraid I will catch a virus”) might influence the result. Preventing viral transmission is critical in this pandemic, and participants’ phonic response to “someone coughing” might be higher than to other items in the emotional response factor. In general, items with factor loading values >0.6 [33] were accepted, but items with values >0.5 also can be acceptable when the consistency is good [34]. Although the factor loading value was low, we accepted item 5 because, first, it is an important issue in social distancing phobia, and second, the internal consistency reliability of the emotional response factor was good (Cronbach’s alpha=0.924, McDonald’s omega=0.919).
Age, viral anxiety, depression, and social distancing phobia
In this study, social distancing phobia was predicted by age, viral anxiety, depression, and IU. Though we did not present the mean Social Distancing Phobia scale score in each age group in the result section, the score was significantly lower in 28–29 years old group (33.9±10.9) than 40–49 years old group (42.7±12.2, p<0.001) and over 50 years old group (41.9±13.9, p<0.001).
The risk of COVID-19–related mortality increases with age, and it is stated that this is especially prevalent in people over the age of 60 years with chronic diseases [35,36]. In addition, because older adults are among the first group exposed to social isolation, psychological problems related to COVID-19 may be seen more in this demographic. Another study stated that the loneliness and social isolation experienced by older adults could increase depression, anxiety, heart disease, cognitive dysfunction, and psychological problems [37]. However, some phobias have also been shown to trigger anxiety disorder; depression; and physical, mental, or mood disorders [13]. All these results show that older adults should pay more attention to themselves. However, older adults who have to go out for limited or compulsory reasons (including shopping or withdrawing money) feel the need to protect themselves more than young people when they go out. In this case, it is thought that phobic behaviors are more prevalent in older adults than in the young. In addition, it has been concluded that a higher phobic tendency is observed in individuals at this age due to the increased risk of viral transmission, especially when adults and people in advanced adulthood have to leave the house, go to work and interact with society at large.
In this study, social distancing phobia was predicted by high levels of viral anxiety measured using the SAVE-6 scale. Since the Social Distancing Phobia scale consists of items for measuring fear or phobic responses to physical or social closeness in the COVID-19 pandemic, it is reasonable that high viral anxiety was significantly associated with social distancing phobia. It was reported that COVID-19–related anxiety was associated with adherence to physical distancing policies [38]. Physical distancing, a term used to exclude the meaning of social isolation from social distancing [39], is an essential policy in preventing viral transmission [40]. However, someone can feel anxious or depressed while staying at a distance or isolated [41]. Conversely, individuals who feel anxious about viral infection are more likely to adhere to physical distancing policies [19].
Conversely, depression was significantly associated with cores of the total scale and three scale factors. The relationship between depression and social distancing phobia is somewhat complicated. In general, depression may decrease compliance with medical advice [42] and adherence to physical distancing policy during this pandemic. Oppositely, forced social isolation might influence one’s depression [43], and an individual’s depression can induce self-isolation. Furthermore, depression is significantly correlated with viral anxiety [21]. Based on these results, fear or phobic responses to physical or social closeness, measured using the Social Distancing Phobia scale, was associated with depression.
Social distancing phobia and intolerance of uncertainty
In our study, IU partially mediated the influence of viral anxiety on social distancing phobia and completely mediated the influence of depressive symptoms on social distancing phobia. This means that people who are more anxious or more depressed about the virus tend to accept uncertainty as more uncomfortable, and this perception causes them to be disproportionately more fearful in terms of protecting themselves from the virus.
Even if an individual has greater levels of IU, it is possible that those with high viral anxiety may also have higher levels of social distancing phobia. This result is similar to a previous study conducted in Canada during the 2009 influenza A virus subtype (H1N1) pandemic [44], which showed a positive relationship between IU and H1N1-related anxiety, and those with a high IU perceived the pandemic as more threatening, which led to elevated levels of anxiety. Also, a study of 3,805 Argentinian participants showed that the participants with higher IU regarding the COVID-19 pandemic showed more anxiety and depressive symptoms. Our study might provide information regarding handling the COVID-19 pandemic. In order to alleviate the phobic symptoms many people experience due to the virus; it may be helpful to take care of their IU of anxiety.
On the other hand, IU completely mediates the influence of depression on social distancing phobia. Depression does not directly affect social distancing phobia in the mediation model. This means that although people who are more depressed tend to be more disproportionately worried about the virus, this is not due to the depression itself but because depression relates to higher IU. Previous studies also show the relationship between depression and IU. A study conducted in the United States suggested a significant association between depressive symptoms and IU [45]. Moreover, a cross-sectional study performed in Greece after the emergence of COVID-19 showed that higher IU was associated with more severe depressive symptoms and that the relationship was partially mediated by fear of the virus [46]. The results of our study are also in line with this conclusion.
Some limitations were noted in the study. Firstly, this study was restricted by its cross-sectional, anonymous online survey-based design. This study’s results do not indicate causal relationships between adherence to physical distancing and other variables. Further, self-reported responses to a web-based questionnaire can be biased. Nevertheless, we decided to conduct the survey online rather than face-to-face interviews to minimize the risk of promoting viral transmission. Secondly, a survey was conducted during January 10th–18th, 2022, which was 2 years after the initial outbreak. There might be a chance of people adjusting to the long duration of COVID-19, which may have affected our results. Third, the small sample size of 400 may have produced bias.
In conclusion, the Korean Social Distancing Phobia scale can measure individuals’ social distancing phobia with good validity and reliability. In addition, IU partially mediated the influence of viral anxiety on social distancing phobia and completely mediated the influence of depression on social distancing phobia. Social distancing phobia is a double-edged sword. It may cause psychological stress but may also increase adherence to physical distancing measures and prevent the spread of viruses. Managing people’s social distancing phobia might be a way to reduce their distress in living with the coronavirus policy in Korea.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2022.0124.
The results of the multi-group confirmatory factor analysis
Item fits and difficulties of the Korean version of the Social Distancing Phobia scale through the Rasch model among participants
The Mantel–Haenszel test for differential item functioning
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Seockhoon Chung, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Seockhoon Chung, Aykut Günlü. Data curation: Inn-Kyu Cho, Oli Ahmed, Dongin Lee, Eulah Cho, Seockhoon Chung. Formal analysis: Oli Ahmed, Seockhoon Chung. Funding acquisition: Seockhoon Chung. Investigation: Seockhoon Chung. Methodology: Oli Ahmed, Seockhoon Chung, Aykut Günlü. Project administration: Inn-Kyu Cho. Validation: Inn-Kyu Cho, Oli Ahmed. Visualization: Inn-Kyu Cho. Writing—original draft: all authors. Writing—review & editing: all authors.
Funding Statement
None