Prolonged Unmet Mental Health Needs of the 2017 Pohang Earthquake Survivors
Article information
Abstract
Objective
Two years after the 2017 Pohang earthquake, some people sought follow-up mental health support. The demographic and clinical characteristics of this unique group of people were investigated to identify some insights on the predisposing factors of the long-term need for psychiatric help after a severe earthquake disaster.
Methods
De-identified data from those seeking mental health support 2 years after the 2017 Pohang earthquake were used. The descriptive statistics of demographic and clinical characteristics of the study group was identified and paired with general population data obtained from open and public governmental websites. Sex, age distribution, destruction of house, and psychiatric disorder were compared between the follow-up sample and general population.
Results
The proportion of women in the group seeking support was two times higher than that in the general population, and people ages between 50 and 70 years commonly sought support. The severity of home destruction was higher among people who sought and needed follow-up mental health support programs than in the general population. There was a higher proportion of people with psychiatric disorders in the group seeking support than in the general population.
Conclusion
The need for long-term mental health support 2 years after an earthquake was higher in women than in men and those aged between 50 and 70 years, and those with a previous psychiatric history and with a higher severity of home destruction, which lead to necessitating leaving the home. Future earthquake response should include screening and psychiatric treatment referral and residential support in vulnerable people.
INTRODUCTION
The 2017 Pohang earthquake occurred in Pohang city, located on the southeast coast of South Korea, of which overall area is 1128.8 km2, number of population is about 500,000, and its industry comprises metal manufacturing, agriculture, and fishing. It is the second strongest earthquake on record in South Korea [1]. A 5.4 magnitude earthquake struck the city. Thereafter, aftershocks ranging from 2.5 to 4.6 magnitude took place. The mortality rate was not high with only one death. However, it caused massive destruction of buildings, including residential and public facilities. Due to the earthquake, approximately 2,000 people were forced to flee their homes.2 People who had to leave their homes due to residential destruction and damage moved to temporary shelters made of small tents in indoor gyms [3].
Local and central government-administered aid provided food and emergency mental health support programs during the immediate aftermath of the earthquake [2]. Data from this initial period after the earthquake showed that 9,086 people sought mental health support [2]. This is three times higher than the incidence of seeking mental health support in a similar but stronger, earthquake in Kyungju city in 2016 (2,498 cases between September and October of 2016) [2]. In a combined sample of data on both earthquakes, 25.64% and 13.85% people were positive for post-traumatic disorders at 7 and 22 months [4]. Thus, about half of people who initially had psychiatric distress no longer screened positive. Nevertheless, over 13% remained needful in mental health support after almost 2 years.
The Pohang Earthquake Trauma Center again offered a follow-up mental health support program in 2019 for people who had trauma after the 2017 Pohang earthquake [2]. This mental health support program provided various tools to improve the psychiatric well-being of individuals. These included non-clinician conducting group and individual therapy such as yoga and aromatherapy based on a post-trauma stress relief program, referral to psychiatric clinics and local social services, and intensive psychiatric interview. The greatest difference in 2019–compared to 2017–was the use of intensive psychiatric interviews by an on-demand psychiatrist. In 2017, a psychiatrist within the mental health support program provided intensive diagnostic and therapeutic psychiatric interviews.
Only few studies have examined long-term psychiatric complications after earthquake disasters, and the results are controversial. One study examined psychological wellness 7 years after an earthquake. Results showed that earthquake exposure was correlated with long-term psychological disturbances [5]. However, a more recent study about 2011 Great East Japan earthquake showed that the prevalence of depression among residents in the disaster area 5.5 years after a tsunami did not increase [6] compared to before tsunami. Two studies were conducted in Turkey. Each of these studies showed that the treatment seeking and non-treatment seeking groups, which comprised people had been exposed to the same earthquake, had a high need for long-term mental health support [7,8].
The current study investigated the demographic and clinical characteristics of the unique group of people who have a high need for psychiatric help 2 years after the 2017 Pohang earthquake. Previous studies showed that women sex and previous history of psychiatric illnesses [9] were correlated with a high incidence of post-traumatic stress disorders (PTSD) after earthquakes. We sought to identify the characteristics of people who demonstrated a prolonged need for psychiatric services after surviving a major disaster, in this case an earthquake. We generated recommendations for establishing future public health policies that address the psychological sequelae of earthquake disasters. We hypothesized that individuals who sought out intensive psychiatric services following the 2017 Pohang earthquake were disproportionately women, elderly, and demonstrated a higher prevalence of pre-earthquake psychiatric issues. These individuals tended to experience more-severe damage to their homes and exhibited more psychiatric symptoms than the general South Korean population. We compared the following variables in individuals with new-onset psychiatric illness following the earthquake and the general Korean population: sex, age group, pre-earthquake history of psychiatric illness, severity of residential building damage, and symptoms of psychiatric illness.
METHODS
Data
The Pohang Earthquake Trauma Center approved the use of these data, collected under the auspices of the Pohang Earthquake Project. Ethical approval for this analysis was obtained from the Institute Review Board at Asan Medical Center (Study #2022-0962) and the University of California San Diego Human Research Protections Program (Study #804676).
A flow chart of 2019 mental health program is displayed in Figure 1. Total 1,200 visited the Pohang Disaster Center for the public mental health support program in 2019, which was held between December 4, 2019 and March 26, 2021. People who used the 2019 mental health support program were not necessarily those who have used the 2017 crisis intervention mental health support program. This program was advertised via on-site and cyber postings, pamphlets distributed in the centers, and mass media advertisement through local broadcastings and local newspapers. The participants were provided with the following mental health support services: transcranial direct current stimulation, eye movement desensitization and reprocessing, biofeedback training, vibroacoustic therapy, sound-bathing therapy, yoga, meditation, aromatherapy, physical activity, gardening therapy, psychodrama, occupational rehabilitation and volunteer experience, case management, and group psychotherapy. Services were first listed and recommended by mental health public officials who are trained staff (nurses or social workers) in the Pohang Earthquake Trauma Center. The participants could freely select and use one or more of those programs regardless of therapist’s referral.
Of 1,200 people, 300 requested an intensive professional psychiatric interview in addition to the offered treatment programs. Individuals could request to use programs multiple times at any point during the 16 months without any limitation on number of requests. One of the authors, who is a psychiatrist, performed an intensive 45–60-min diagnostic and therapeutic psychiatric interviews on each person. This group of people included those who seek and have a high need for psychiatric help. Public, de-identified data obtained from the Pohang Earthquake Trauma Center were used for mining data on the demographic and clinical characteristics of this group. Interviewers produced and handled data. None of the authors managed original data containing personal identifiable data, which were deleted by interviewers before research use. All sensitive personal data were not included if delivered to the researchers. In this study, the following data were used: sex, age, previous history of lifetime trauma, PTSD before the earthquake, psychiatric disorder before the earthquake, chronic illness, severity of residential damage, suicidal ideation, and high risk of suicide based on the objective determination of the interviewer.
The paired data of the general population with the above mentioned data of the 2019 Pohang Earthquake Mental Support Program were obtained from governmental data on the websites open to the public [10-12]. We used 2021 data of prevalence of psychiatric disorders in the general population of South Korea as controls in all cases except comparison of bipolar disorders. In this case, 2018 data, which is the second recent public data available, were utilized for prevalence of bipolar disorder because 2021 data about bipolar disorder could not be obtained from public databases. In the general population, we could only obtain data from the number of houses damaged according to the degree of damage. We replaced the number of people whose house is damaged due to the earthquake with this number.
Tools
All data were obtained from people who used mental health support programs via short surveys and one-on-one interviews. Mental health support primary providers were trained center staffs (nurses and social workers) and they did face to face survey about psychiatric symptoms, and emotional and social difficulties.
The governmental rescue project determined the severity of the destruction of the building, which was rated as one of three levels: moderate, severe, and complete. Moderate destruction is the degree of destruction that prevents people from residing unless there should be significant repair. Severe destruction is defined as the degree of destruction that exceeds the condition of moderate destruction and that has ≥50% destruction but less than complete destruction. Complete destruction is defined as the degree of destruction in which whole walls and pillars were destroyed. Minimal destruction was defined as all other destructions other than those previously mentioned.
Mental health support primary providers directly questioned suicide ideation. The objective measure of high-risk suicide was determined by mental health support providers based on two or more of the following symptoms: 1) depression disturbing social and occupational function, 2) suicide ideation with impulsiveness, and 3) persistent suicide ideation or suicide planning.
All intensive psychiatric interviews were performed by a psychiatrist with more than 30 years’ experience. These one-on-one, in-person interviews took place within a secure and quiet room at the Pohang Earthquake Trauma Center and generally lasted 45 minutes to one hour. Following the unstructured psychiatric diagnostic and therapeutic interviews, diagnosis was determined according to the interviewing psychiatrist’s diagnostic impression. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition diagnostic criteria were used for the clinical diagnosis. All of the diagnoses were made by one psychiatrist.
Statistics
The chi-square test was used to compare categorical variables between the study group and the general population. The Kruskal–Wallis test was used to determine differences in age distribution between the study group and the general population. Further, the chi-square test was applied to explore potential sex differences in psychiatric history. A p<0.05 is considered statistically significant. Stata13-SE (StataCorp LP., College Station, TX, USA) was used for analysis.
RESULTS
Table 1 shows the demographic and clinical (particularly a previous history of psychiatric illnesses) characteristics of the study group (n=300) who sought mental health support in 2019 and requested a psychiatric interview.

Demographic and clinical (particularly a previous history of psychiatric illness) characteristics of the study group who sought mental health support in 2019 in the 2019 Pohang mental support program for the 2017 Pohang earthquake survivors and who requested an intensive psychiatric interview
There was a statistically significant difference (chi-square test, p<0.0001) in terms of sex proportion between the study group and the general population (Figure 2). That is, the proportion of women who sought help in the study group was significantly higher than that in the general population.
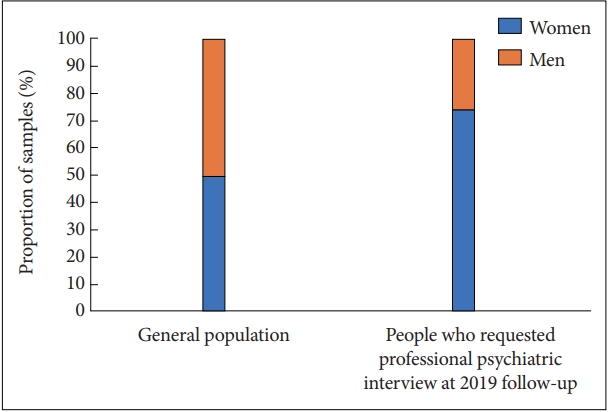
Comparison of the proportion of women between the people who requested a professional psychiatric interview at the 2019 follow-up (N=300) and the general population in Pohang (N=547,247) (chi-square test, p<0.05).
The participants were aged 4–107 years. Their median age was 62 years old. Figure 3 shows the age distribution according to 10-year intervals. There was a statistically significant difference in terms of age distribution between the general population and people who requested intensive psychiatric interview (p<0.001). That is, the study group was older than the general population.

Age distribution of people who required professional psychiatric interview at the 2019 follow-up (N=300) and general population in Pohang (N=547,247).
Figure 4 shows an uneven proportion in terms of sex according to age group. The differences in the distribution of sex according to age significantly differed (Kruskal–Wallis test, chi-square test=22.8, df=8, p=0.004). The preponderence of women among those requesting intensive interviews was most significant among people in their 50s to 70s.
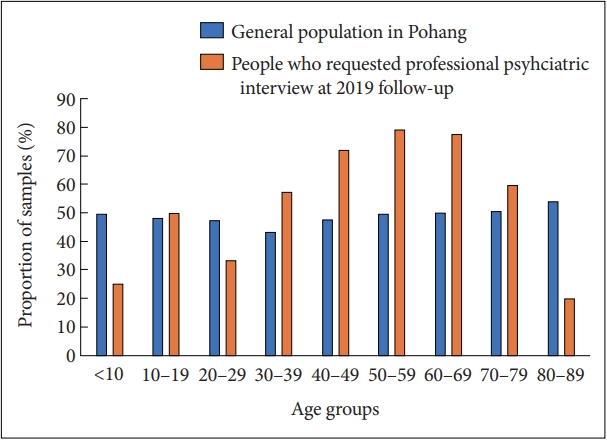
Age distribution of the proportion of women who participated in the follow-up mental health support program 2019 for psychiatric trauma caused by the 2017 Pohang earthquake (N=300) and general population in Pohang (N=547,247).
The extent of residential building damage in 272 people in the study group was assessed. Figure 5 depicts the distribution of people according to the severity of damage. An official public showed the damage to the residential buildings of families living in the Pohang area in 2017. The distribution of the extent of damage between two groups significantly differed (p<0.001).

Levels of residential building damage caused by the earthquake in individuals who requested professional psychiatric services at their 2019 follow-up appointments (N=272; the number of participants who officially reported and evaluated the degree of damage by public officials) and general population in Pohang (N=202,469; we used house number instead of the number of people due to the lack of available data about the number of people in each house. The severity of damage to a residential building in the general population per family was reported).
Considering the higher proportion of women seeking psychiatric interview, particularly among those aged between 50 and 70 years, we explored whether there were sex and age differences in any of the clinical characteristics or in the degree of household destruction. Results showed no difference for any of the variables (all p>0.05). Hence, the demographic characteristics of the study group did not explain the other unique clinical and experiential characteristics of individuals seeking interviews.
Most people in the study group were newly diagnosed with psychiatric disorders by the psychiatrist (Table 2). Anxiety disorders were the most prevalent diagnoses, Followed by depressive disorders and PTSD. Approximately one-fifth of patients had two or more simultaneous disorders. Compared with the number of people who had a previous psychiatric history before earthquake (n=26), the study group had a significant increase (p<0.001) in the number of people who had a new psychiatric diagnosis (n=261). Among people who had a new psychiatric diagnosis, 50 (19%) were already treated by psychiatrists. Of the remaining 211 (81%) people who were newly diagnosed with psychiatric disorder and were not receiving treatment, 170 (65% of those with new diagnoses) were considered in need of immediate psychiatric treatment and were recommended to start psychiatric treatment as early as possible and referred to psychiatrists if they provided consent.
People who needed psychiatric treatment before and after the Pohang earthquake were included in this figure, and the total number of people in this figure is 224 (75% of 300 subjects). Among them, 159 (71% of 244 people) subjects in the solid red box is the number of subjects who newly developed a diagnosis of psychiatric disorders untreated at the 2019 follow-up psychiatric interview.
In total, 221 of 300 participants (74%) who requested psychiatric interviews needed psychiatric treatment based on the interviewing psychiatrist. Among them, 50 (23%) were already receiving psychiatric treatment. However, 171 (76%) were not (Figure 6). In addition, most interviewees were never diagnosed a psychiatric disorder before (n=273, 91.0%). Most participants who did report a previous history of psychiatric illness (n=27) required psychiatric treatment during the 2019 Pohang earthquake follow-up (n=24, 88.9%). Of 273 participants who did not have any psychiatric history before the 2017 Pohang earthquake, 221 (81.0%) required psychiatric treatment at the 2019 Pohang earthquake follow-up.

Number and proportion of participants who had a previous history of psychiatric illness before the 2017 Pohang earthquake (previous history), participants who currently required psychiatric treatment in 2019 (current need), and participants who were already receiving psychiatric treatment in 2019 (in treatment).
DISCUSSION
The current study first investigated the demographic and clinical characteristics of people who want to receive psychiatric intervention and undergo assessment 2 years after the 2017 Pohang earthquake. While 8,977 respondents used the crisis intervention mental health support program immediately after the 2017 Pohang earthquake, there were 1,200 who accessed the mental health support program in 2019. These results suggest that a subset of survivors required prolonged mental health support, even 2 years after the earthquake. Most people in the study group were diagnosed with clinically significant PTSD, depressive disorders, and anxiety disorders, and they required psychiatric treatment. We found an over-representation of women and people aged between 50 and 70 years old in this group compared with the general population. Most people desiring psychiatric interview received new diagnoses, and they needed treatment. However, most were previously undiagnosed and untreated. There is persisting needs of mental health support for these population. Suicidal ideation (high severity) was more prevalent in the study group than in the general population. This group had a greater severity of residential destruction than the general population.
The proportion of women in the group who needed mental health support was higher than that of men. Further, the proportions of women were significantly greater, particularly among those aged 30–60 years, than those of in the general population. Women had higher requests for further professional psychiatric help. However, there were no significant sex differences in the rate of newly developed psychiatric disorders and suicide risk. There are two possible hypothesis explaining this finding.
First, it can be explained by the biopsychosocial vulnerability theory, which is consistent with a well-known finding that that the prevalence of depressive disorders and PTSD is approximately two times higher in women than in men [13-16]. In addition, a previous report showed that women have higher levels of post-traumatic stress symptoms related to earthquakes than men [17]. Nevertheless, this observation is not well established yet. However, sex differences can be explained by several hypotheses. The proposed explanations for the higher incidence of depression in women are hormonal differences, different socioeconomic stresses, higher sensitivity to interpersonal relationships among women, and women’s propensity to internalize symptoms. Regarding PTSD, women may have different PTSD-eliciting processes compared with men. Women are more likely to re-experience symptoms in response to physiological cues [18], and they present with different retrieval of trauma-related memory [19-22]. In women, neuro-endocrinological differences in response to trauma [23], oxytocin-related sex-specific response in the amygdala and vmPFC [24], and heightened sensory strength and mental imagery based on sex hormones in women25 are the possible underlying biological mechanisms [26].
Second, men may less likely seek psychiatric help than women because seeking psychiatric interview may be a sign of inner weakness or failure or defect in masculinity [27]. This may lead to the low requests of psychiatric service and underestimation of psychiatric disorders among men who have trauma than women. Further research about the prevalence of psychiatric disorders after earthquake in terms of sex differences is necessary. Moreover, future public mental health support program should exert effort on identifying undetected newly developed psychiatric disorders in men after severe earthquakes.
The age distribution significantly differed between people who seek and need mental health support 3 years after the 2017 Pohang earthquake and the general population in the disaster area. People who are in their 50s, 60s, and 70s were at highest risk for the persistent need for mental health support. People who are aged less than 50 years were not at high risk for prolonged need for mental health support. Previous reports have contrasting results. Some studies showed that older adults are at higher risk of PTSD [28,29]. Moreover, several studies have shown that the vulnerability of elderly survivors from earthquake is correlated with more functional disability [30] and cognitive decline [31] based on age. However, others have revealed that younger age is a risk factor [32]. This inconsistency may be attributed to differences in the characteristics of each disaster and the socioeconomic or cultural background of the massive disaster area.
The study group had a significantly higher prevalence of depressive disorders alone than the general population. Previous studies have reported that a history of previous psychiatric illnesses including depressive disorders can be a predisposing factor for PTSD after earthquakes [33]. People who have a previous history of depressive illness is more likely to seek psychiatric help 2 years after the earthquake. Nevertheless, further investigation about the predisposing effect of depressive illness compared with other psychiatric illnesses should be performed.
The casualty rate after the 2017 Pohang earthquake was not high. There was only recorded one death correlated with the earthquake, and only 135 people had injuries [2]. However, 57,039 buildings were severely destroyed. Hence, they could not be used without repairs or reconstructions [2]. The earthquake damaged the residences of 202,469 families, and 1,797 people became homeless [2]. The current study showed that the residential building of most people in the study group seeking psychiatric help were destroyed. Hence, people could not reside there without significant repair. In contrast, in most cases in the general population, the destruction of residences was minimal. The residence is not just a building or personal property. It is a vital element of our physical and social lives. The 2017 Pohang earthquake impacted this point in people’s lives. While the local and central governments had plans to help residents repair or rebuild their houses, people who were homeless lived in small tents provided by the government, each of which can just accommodate one or two people in 39 public indoor gyms [34]. People stayed in these tents for approximately 4 years (1,435 days, 11 people from 9 families), which was the longest duration [35]. There was no facility for private baths and cooking. Moreover, the number of bathrooms was extremely few, and the heating and air conditioning system was poor [34]. There was no privacy, and people had poor hygiene. These factors likely contributed to poorer mental health and low resilience among people with greater building damage.
There was a significant unmet need for mental health treatment in the group of people who requested intensive psychiatric interviews 2 years after an earthquake. Most people in this group were newly diagnosed with psychiatric disorders. About three-quarters (73.7%) of people required immediate psychiatric treatment. Only 20% of people who needed immediate psychiatric treatment were currently receiving it. Approximately two-thirds (71.3%) of people presented with anxiety disorders and one-third (34.3%) with depressive disorders by a psychiatrist’s diagnostic assessment. This finding is consistent with previous research results [5,36-38]. That is, earthquake survivors are at risk of not only post-traumatic disorders but also depressive and anxiety disorders. In addition, there were high rates of suicidal ideation among the study group compared to general population (37.7% vs. 1.3%). More than one-third (36.3%) of people who reported suicidal ideation were clinically at high risk of suicide. These people needed psychiatric crisis intervention and further psychiatric follow-up at 2 years after the earthquake.
The prevalence of PTSD after an earthquake ranged from 1.2% to 82.6% [39]. The diversity of influence of earthquakes on mental health is determined by different factors, including the severity of exposure to the disaster and post-earthquake socioeconomic state. In particular, the loss of residence and property-related problems can enhance post-traumatic stress [28,36]. In this study group, the prevalence rate of persisting PTSD after 2 years was 23.3%. The prevalence of PTSD was higher than that of PTSD based on a previous study with long-term follow-up. The prevalence is similar to that of post-traumatic disorder among people whose house was destroyed by the 1999 Taiwan earthquake (20.9%), which caused significant public criticism on the unsatisfactory governmental performance for recovery from the disaster [36]. However, the prevalence rate (11.1%) of post-traumatic stress symptoms is relatively low among elderly individuals affected by the Great East Japan earthquake, which caused massive destruction of houses [31]. Moreover, the closure of emergency shelter was performed approximately 10 months after the earthquake [31]. However, it took almost 4 years until emergency shelters were closed after the Pohang earthquake [35]. The study results indicated that post-disaster residential support and mental health care service might help prevent the long-term disturbance of mental health and decrease the need for mental health support.
There are several limitations of current study when interpreting the results. First, this is not a designed or controlled study, and publicly available data were used. Second, the authors presented paired data from the general population. However, these data were not statistically processed with the study data. Third, the discrepant accessibility of mental health support programs among victims might have influenced the study results. Treatment accessibility might be limited by transportation difficulty due to physical disability or financial disruption and lack of time to visit the Pohang Earthquake Trauma Center. In addition, this study did not provide information about the group of people who participated in the 2019 Pohang mental health support program but did not request intensive psychiatric interview. Therefore, further study should compare the group of people who requested intensive psychiatric interview and the group of people who did not.
Conclusions
There was a significant unmet need for psychiatric treatment among people who sought professional psychiatric help 2 years after the 2017 Pohang earthquake. Almost all people in the study group required psychiatric treatment. However, only few were receiving intervention. Among them, women, those aged between 50 and 70 years, and those who experienced more severe damage to their residential building were more likely to have long-term psychiatric needs after the earthquake. Therefore, future public mental health support after earthquake disasters should focus on follow-up screening and referral of earthquake survivors, particularly those in high risk groups, to psychiatric treatment and the establishment of a comprehensive residential support plan to help survivors immediately return to their normal way of life. Public mental health support programs can serve as “bridges” to accessing psychiatric treatments while providing needed mental health services, from community to clinic. Assistance with activities of daily living (including the repair of residences damaged by earthquake disasters) is important and may help prevent the need for prolonged mental health services following a earthquake disaster.
Notes
Availability of Data and Material
Participant data is not publicly available due to privacy protection reasons and governmental policy of public official data protection.
Conflicts of Interest
Jungsun Lee, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Soohyun Joe, Lisa T. Eyler. Data curation: Soohyun Joe. Formal analysis: Soohyun Joe, Lisa T. Eyler. Funding acquisition: Youngryeol Lee. Investigation: Soohyun Joe, Youngryeol Lee. Methodology: Soohyun Joe, Lisa T. Eyler. Project administration: Lisa T. Eyler, Youngryeol Lee. Resources: Youngryeol Lee. Software: Soohyun Joe, Lisa T. Eyler. Supervision: Lisa T. Eyler, Youngryeol Lee. Validation: Soohyun Joe, Jungsun Lee, Lisa T. Eyler, Youngryeol Lee. Visualization: Soohyun Joe. Writing—original draft: Soohyun Joe. Writing—review & editing: Jungsun Lee, Federica Klaus, Hui Xin Ng, Lisa T. Eyler, Youngryeol Lee.
Funding Statement
None
Acknowledgements
This study is performed and supported from Pohang Earthquake Trauma Center with the data use permission for the research as a part of the R&D project in Pohang earthquake project.


