|
 |
- Search
| Psychiatry Investig > Volume 20(7); 2023 > Article |
|
Abstract
Objective
Methods
Results
Conclusion
Supplementary Materials
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Euitae Kim, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Seoyoung Kim, Michael Bloomfield, Euitae Kim. Data curation: Hyejin Sim, Paul Guyun Jung. Formal analysis: Hyejin Sim. Funding acquisition: Michael Bloomfield, Euitae Kim. Investigation: all authors. Methodology: Hyejin Sim. Project administration: Michael Bloomfield, Euitae Kim. Resources: Seoyoung Kim, Euitae Kim. Software: Hyejin Sim. Supervision: Michael Bloomfield, Euitae Kim. Validation: Hyejin Sim, Paul Guyun Jung. Visualization: Hyejin Sim. Writing—original draft: Hyejin Sim. Writing—review & editing: Hyejin Sim, Seoyoung Kim, Paul Guyun Jung, Euitae Kim.
Funding Statement
The study was supported by the National Research Foundation of Korea (NRF) grants funded by the Korean government (MSIT) (No. NRF2019M3C7A1032472, NRF-2022R1A2B5B02002400).
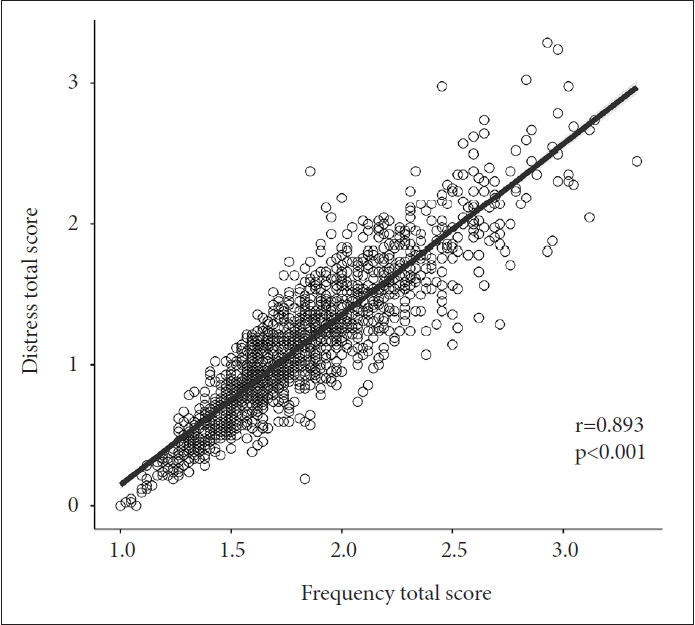
Figure 1.
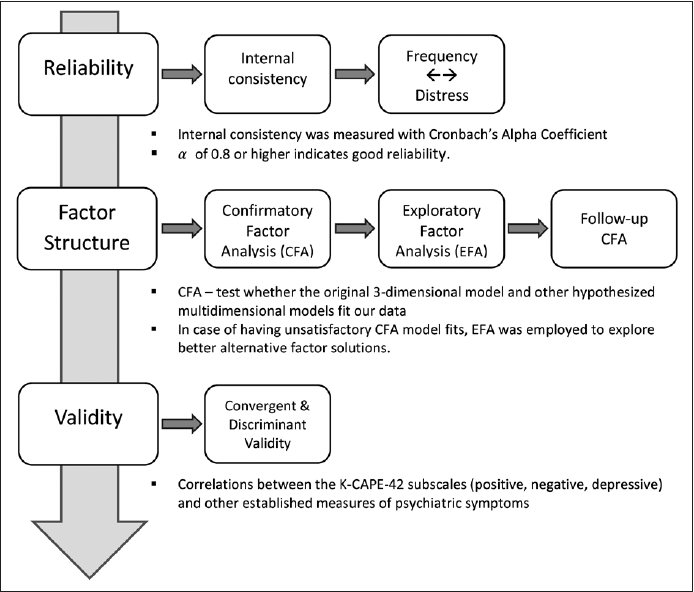
Table 1.
|
Original |
Hypothesized multidimension |
||
|---|---|---|---|
| 3-Factor* | 5-Factor† | 7-Factor‡ | 9-Factor‡§ |
| Positive | Delusional Ideations | Paranoia | Paranoia |
| Grandiosity | Grandiosity | ||
| Bizarre Experiences | Bizarre Experiences | Bizarre Experiences | |
| Hallucination | Hallucination | Hallucination | |
| Negative | Negative | Negative | Social Withdrawal |
| Affective Flattening | |||
| Avolition | |||
| Depressive | Depressive | Depressive | Depressive |
Table 2.
Values are presented as mean±standard deviation or number (%).
Before any further analysis, the entire sample was randomly divided into two subsamples. Sample 1 was used for EFA while Sample 2 was used for the follow-up CFA. Among 1,467 participants, 17 were excluded according to the inclusion criterion. K-CAPE-42, Korean version of the Community Assessment of Psychic Experiences; EFA, exploratory factor analysis; CFA, confirmatory factor analysis
Table 3.
Before any further analysis, the entire sample was randomly divided into two subsamples. Sample 1 was used for EFA while Sample 2 was used for the follow-up CFA. Cronbach’s alpha values greater than 0.70 were considered to be acceptable for further anlaysis. KCAPE-42, Korean version of the Community Assessment of Psychic Experiences; EFA, exploratory factor analysis; CFA, confirmatory factor analysis
Table 4.
| Number of factors |
Goodness-of-fit index |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| χ2 | df | p | RMSEA | GFI | TLI | CFI | SRMR | RMR | |
| 3 | 6,925 | 816 | <0.001 | 0.074* | 0.775 | 0.695 | 0.711 | 0.074* | 0.049* |
| 5 | 6,702 | 809 | <0.001 | 0.071* | 0.792 | 0.723 | 0.740 | 0.071* | 0.047* |
| 7 | 5,175 | 798 | <0.001 | 0.062* | 0.828 | 0.791 | 0.807 | 0.060* | 0.038* |
| 9 | 3,752 | 783 | <0.001 | 0.051* | 0.883* | 0.856 | 0.869 | 0.054* | 0.033* |
| 3-factor solution | 3,618 | 816 | <0.001 | 0.069* | 0.789 | 0.747 | 0.760 | 0.077* | 0.051* |
Meeting minimally acceptable fit criteria: RMSEA ≤0.08, GFI ≥0.85, CFI ≥0.90, TLI ≥0.90, SRMR ≤0.08, RMR ≤0.05. RMSEA, root mean square error of approximation; GFI, goodness of fit Index; TLI, Tucker-Lewis index; CFI, comparative fit index; SRMR, standardized root mean square residual; RMR, root mean square residual
Table 5.
Only items with factor loadings ≥0.30 are shown. K-CAPE-42, Korean version of Community Assessment of Psychic Experience; Depressive, depressive symptoms; Pos, positive symptoms; Neg, negative symptoms; Soc. Withd, social withdrawal; Biz. Exp, bizarre experience; Mag. Think, magical thinking; Aff. Flat, affective flattening; SS loadings, the sum of squared loadings; Var, variance
Table 6.
|
Positive |
Negative |
Depressive |
|||
|---|---|---|---|---|---|
| Paranoia Scale | DES-II-DD | O-LIFE-UE | O-LIFE-IA | PHQ-9 | |
| K-CAPE-Pos | 0.643* | 0.595* | 0.639* | 0.241 | 0.455 |
| K-CAPE-Neg | 0.582 | 0.404 | 0.407 | 0.566* | 0.623 |
| K-CAPE-Dep | 0.633 | 0.409 | 0.438 | 0.434 | 0.726* |
K-CAPE-42, 42-item Korean version of Community Assessment of Psychic Experiences; Pos, positive domain; Neg, negative domain; Dep, depression domain; DES, Dissociative Experiences Scale; DD, depersonalization/derealization; O-LIFE, Oxford-Liverpool Inventory of Feelings and Experiences; UE, unusual experience; IA, introvertive anhedonia; PHQ-9, 9-item Patient Health Questionnaire
REFERENCES