Occupational and Psychological Factors Associated With Burnout in Night Shift Nurses
Article information
Abstract
Objective
Providing inpatient nursing care inevitably involves night shift work. However, night shift work nurses often face psychiatric health problems such as burnout. If night shift work is an essential work type for nurses, it is necessary to select personnel suitable for night shift work or establish improvement measures such as psychiatric intervention through psychiatric evaluation. The objective of this study was to identify factors that could be interventional among factors affecting burnout in shift-working nurses.
Methods
A total of 231 night shift female nurses participated in this study. A questionnaire survey was given to assess their general characteristics. To assess burnout, the Maslach Burnout Inventory–General Survey Korean version was adopted. In addition, several mental health scales were used to identify individual psychological characteristics. To identify variables associated with the presence of burnout, odds ratios were calculated using a logistic regression model taking three dimensions of burnout as a dependent variable after adjusting for psychological and occupational factors.
Results
High resilience was a significant preventive factor in the three dimensions of burnout. Regarding occupational factor, the longer the duration of employment, the higher depersonalization, but the professional efficacy was good.
Conclusion
Our results indicate that resilience and social support could be prevention factors for burnout. This study is meaningful in examining items that require active intervention and support for burnout targeting night shift nurses who are indispensable for patient care.
INTRODUCTION
Providing inpatient nursing care inevitably involves night shift work. However, night shift work is included in workplace hazards that can cause sleep disturbance, endocrine disturbance, gastrointestinal disease, cardiovascular disease, and psychological problems [1,2]. Night shift work might have a variety of adverse health effects. South Korea authorities have also recognized its seriousness. South Korean workers receive occupational hazard-related special medical examinations annually according to the law from the Occupation Safety and Health Acts (where “hazard-related” is defined as direct exposure to any of 109 chemicals including toluene, 20 metals, seven dusts including mineral dust, eight physical agents including noise and vibration, and others). The special health examination for night-shift work started in 2013 [3]. However, there is no examination or evaluation of mental health of night workers except for sleep disorders.
Night shift work nurses often face psychiatric health problems such as sleep disturbance, depression, occupational stress, and anxiety. Among psychiatric health problems, emotional exhaustion of nurses is a major concern because of its potential impact on quality and safety of patient care [4]. Moreover, emotional exhaustion is one of the reasons why nurses leave their job and the profession [5]. High turnover is an important nursing workforce issue in South Korea. Night shift and night work patterns have been identified as important factors in determining well-being and satisfaction among nurses [6]. Rotating shift work can result in longer reaction time, reduced alertness, judgement problems, and impairments of concentration, memory, and information processing, which can undermine nurse and patient safety [7]. Clearly, rotating night shift is a critical factor that can increase nurses’ exhaustion. In addition, emotional exhaustion affects patient care and job turnover. In South Korea, demand for healthcare is expected to increase because of the rapidly aging population and increasing number of people with a chronic disease. However, nurses in South Korea are known to have high stress and high turnover [8]. Recently, different factors, including the emergence of new infectious diseases, certification evaluations of medical institutions, and high work stress, are accelerating burnout of nurses [9].
That night shift work is a major risk factor for burnout has been suggested in many previous studies, and there is no doubt that night shift work is a risk factor for burnout [5]. However, there are not many studies on which work-related factors are risk factors or which individual characteristics are preventive factors for burnout in performing night shift work. If night shift work is an essential work type for nurses, it is necessary to select personnel suitable for night shift work or establish improvement measures such as psychiatric intervention through psychiatric evaluation. Emotional exhaustion in nurses could be prevented with proper interventions if psychological factors associated with burnout are known. In terms of occupational environment, evaluation for improvement is also needed. Thus, it is necessary to find factors contributing to burnout of night shift work nurses and determine which nurses are more affected by burnout. By identifying exacerbating factors, psychiatric intervention treatment and working environment can be improved. Therefore, the aim of this study was to identify factors that could be interventional among factors affecting burnout in shift-working nurses.
METHODS
Study population
In this study, the survey was conducted over two years, 2015 and 2016, before the coronavirus disease-2019 (COVID-19) pandemic began. A hospital was the research site. It is a tertiary care university hospital with more than 900 night-shift nurses at the time of this study. This study included all night shift nurses (intensive care unit, intermediate care unit, operating room, recovery room, general ward, and emergency department) who were willing to participate in the study. A total of 235 night shift nurses participated in this study. We selected 231 subjects after excluding four male nurses. This study and all protocols were approved by the Institutional Review Board and Ethics Committee of Soonchunhyang University Hospital (IRB number: 2015-05-013). This study was performed in accordance with approved guidelines.
Questionnaire and psychological measures
A questionnaire survey was given to assess general characteristics. The questionnaire included general questions pertaining to age, duration of employment, working hour per month, amount of exercise, smoking, drinking, house income, marital status, religion, job rank, department in hospital, and education. To assess burnout, the Maslach Burnout Inventory–General Survey (MBI-GS) Korean version was adopted. The MBI has been considered the standard tool for research in burnout. It has been translated to many languages and validated. MBI-GS was developed by Maslach and Jackson [10]. The Korean version of the MBI-GS was modified by Shin [10], which also has good validity and reliability. The MBIGS Korean version, a 15-item questionnaire designed to assess the presence of burnout in general worker, contains three dimensions for evaluating underlying constructs of burnout: emotional exhaustion, depersonalization, and professional efficacy. Each dimension comprises several items. Each item was rated by the respondent on a 7-point Likert scale according to the frequency of their occurrence (0: ‘‘never’’ to 6: ‘‘every day’’). Professional efficacy was inversely calculated.
To measure the severity of depressive and anxiety symptoms, the Patient Health Questionnaire–9 (PHQ-9) [11] and Generalized Anxiety Disorder–7 (GAD-7) [12] scale were used. The Davidson Trauma Scale with 18 items is a commonly used measure of traumatic experiences. To assess secondary traumatic stress, a 17-item secondary traumatic stress scale was administered [13]. A 25-item Connor-Davidson Resilience Scale, [14], a self-rated measure used for evaluating resilience, was also used. To assess individual stress, a 10-question Perceived Stress Scale (PSS) [15] was applied. A 16-item World Health Organization Quality of Life Scale-Abbreviated Version (WHOQOLBREF) [16] was used to evaluate quality of life. A 14-item version of Duke-UNC Functional Social Support Questionnaire (FSSQ), a self-administered, multidimensional questionnaire, was used to assess functional social support [17]. The FSSQ was developed as a 5-point Likert scale with each item rated from 1 (as much as I would like) to 5 (much less than I would like).
Classification of variables
Participants were classified by age as 29 years or younger, 30–39 years old, and 40 years or older. Amount of exercise was divided into >1 time/week and ≤1 time/week. Times of alcohol intake were divided into >2 times/week and ≤2 times/week. The duration of employment was divided into less than 4 years, 4 to 9 years, and more than 10 years. Marital status was classified into unmarried and married. Monthly household income level was categorized as follows: less than 3 million Korean won (KRW), 3–5 million KRW, and 5 million KRW or above. Work departments were divided into emergency/intensive care unit part and others. Education level was classified into college and above. Job rank was classified into staff nurse and manager (nurse in charge and above). MBI-GS is not a clinical diagnostic tool for burnout. The authors who have developed the MBI-GS recommend using it as a continuous variable. However, in several studies, a cutoff value was set and attempted in dichotomous or trichotomous categories. There is no set standard for this cutoff value. Cutoff values for emotional exhaustion, depersonalization, and professional efficacy were dichotomized at the median (low vs. high). PHQscores was divided into two categories: 0–9 and 10 or greater [11]. Other psychological measures were dichotomized at the median (low vs. high).
Statistical analysis
There is a general consensus in the literature that emotional exhaustion is the central or core dimension of burnout [18]. However, studies using Maslach’s theory have suggested that all three MBI dimensions should be used and reported [4]. Student’s t-test and χ2 test were used to examine general characteristics of study subjects according to their current status of night shift work. The test was conducted to examine night shift work-related variables of study subjects according to the grade of their burnout. Comparative analysis between highand low-exhaustion groups in this study was conducted using a χ2 test. To identify variables associated with the presence of burnout, odds ratios were calculated with a logistic regression model taking the three dimensions of burnout as dependent variables after adjusting for sociodemographic and occupational factors. When estimating linear trends, the duration of employment grade was considered a continuous variable. All statistical analyses were performed with IBM SPSS version 26.0 (IBM Corp., Armonk, NY, USA) and p-values of less than 0.05 were considered to be statistically significant.
RESULTS
General characteristics and psychological measures
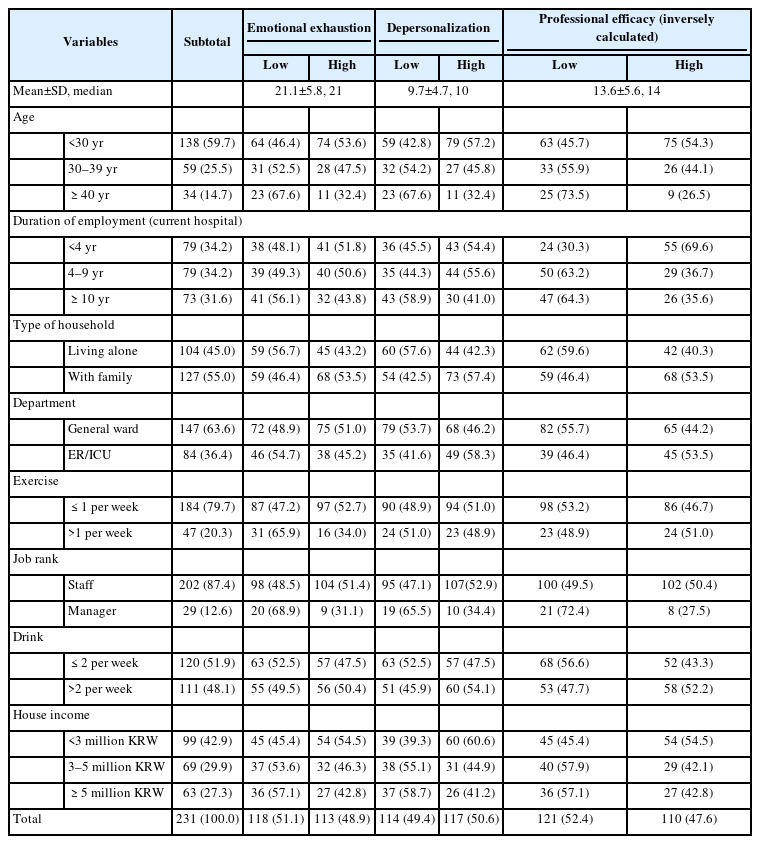
Sociodemographic and occupational characteristics of enrolled subjects are summarized in Table 1. The most common age group was <30 years (138 [59.7%]). The most common duration of employment among participants was between 1 and 5 years. Table 2 shows psychological characteristics of all study participants. Of the group with high depression, 73.7% had high emotional exhaustion, which was more than twice higher than the low depression group. Resilience seemed to have significant correlations with the three dimensions of burnout among personal characteristics (Table 3).
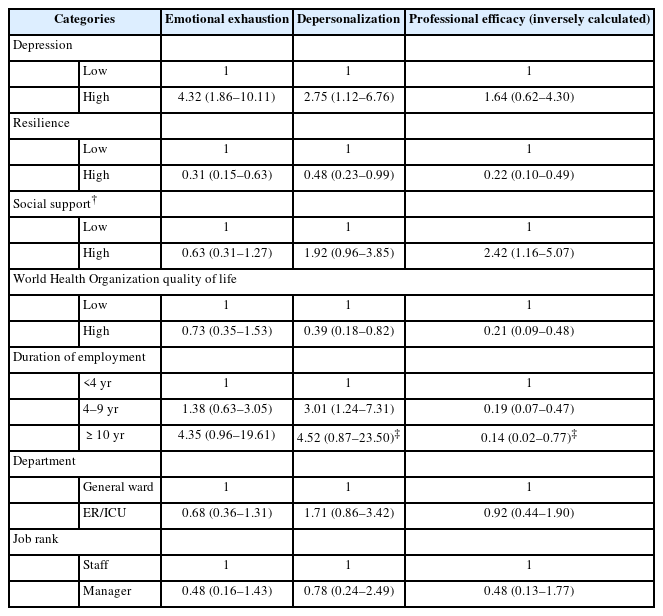
Comparison between high- and low-exhaustion participants
After controlling variables related to psychological characteristics, a logistic regression analysis was performed. Compared to the low depression group, the high depression group had an odds ratio of 4.32 (95% confidence interval [CI] 1.86– 10.11) for developing emotional exhaustion and depersonalization. High resilience was a significant preventive factor in the three dimensions of burnout. The better the social support, the better the job efficacy. Quality of life showed an effect of preventing an increase in depersonalization and a decrease in job efficacy. In the case of occupational factor, the longer the duration of employment, the higher the depersonalization, but the better the professional efficacy. Other occupational characteristics showed no significant association with burnout (Table 3).
DISCUSSION
Burnout has three main dimensions of response: emotional exhaustion, depersonalization and a sense of detachment from work, and feelings of inefficiency and lack of fulfillment [19]. The main interest in this study was to determine what factors might affect burnout in night shift nurses. Workload and characteristics of jobs contributing to the workload were factors investigated the most in previous studies. Workload has been associated with emotional exhaustion in several studies [20]. Some studies have also reported a relationship of workload with depersonalization [21]. There is evidence that a high workload and nurse staffing levels are associated with burnout. Time pressure is also associated with emotional burnout [4]. To determine the degree of burnout according to work load, nurses working in emergency and intensive care units (known to be relatively difficult departments) were compared with nurses working in general wards. However, there was no significant difference. In addition, working hours identified in this study were about 40 hours per week on average. Differences among nurses could not be confirmed. The longer the duration of employment after joining the company, the higher the distribution of groups with high levels of burnout and depersonalization. Long duration of employment is known to be a risk factor for emotional burnout [22]. However, in our study, the longer the duration of employment, the better the professional efficacy. It can be interpreted that nurses with a longer duration of employment can continue to work because of their good professional efficacy, although they are emotionally exhausted. However, more research is needed on this. Insufficient recognition and reward (whether financial, institutional, or social) can increase people’s vulnerability to burnout because it devalues both the work and workers. It is closely associated with feelings of inefficacy. It is known that a higher score on the reward disparity scale is related to emotional burnout [23]. However, this study did not show a significant correlation between household income and burnout. Night shift work nurses also experience a fragmented work process, interpersonal relationships that are often conflictive, low wages, a highly demanding environment, and emotional stress. They want to work the day shift even if the pay level is lower [24,25]. Autonomy is known to play an important role in the three main dimensions of burnout [4], but we did not investigate autonomy in our study. However, autonomy has been shown to be related to job rank in previous studies [26]. Meanwhile, research results on the relationship between job rank and burnout are sparse. One study has reported that having opportunities for promotion is not associated with burnout [27]. In our study, there was no significant difference according to job rank; this was likely due to the widened CI associated with the small number of subjects with manager rank or higher.
In terms of psychological factors, the present study showed that greater resilience and social support was associated with reduced emotional exhaustion, depersonalization, and increased professional efficacy. This result was consistent with previous research studies [28,29]. Resilience can be defined as an ability to adapt and successfully cope with acute or chronic adversity [30]. High resilience and social support were associated with a lower risk of burnout, supporting the need for developing a resilience training program to promote a lifetime of mental wellness for nurse’s assignment to night shiftwork. Previous studies have shown that social support could have a buffering effect against burnout in nursing personnel [31]. Social support is needed to alleviate nurses’ occupational stress, emotional stress, and improve their mental health [32]. Our study has revealed that conditions such as depression are related to greater emotional exhaustion and depersonalization. A literature review has noted that depression and burnout are distinct concepts [33], although the causal relationship between them remains unclear. However, each state has implications for the other. We found no association between emotional exhaustion and traumatic stress. The prevalence of burnout is highly associated with poor quality of life as well as physical and psychological health. In WHOQOL-BREF results, poor quality of life is associated with high depersonalization and low professional efficacy. A previous study has shown positive associations of personal accomplishment with all dimensions of quality of life and a negative association of personal accomplishment with depersonalization [34].
Our study has several limitations. It is known that the fewer patients a nurse is in charge of, the lower the overall burnout score is [35]. However, this study has a limitation in not being able to quantitatively evaluate the workload, such as the number of patients in charge per nurse. Working hours of nurses identified by us might have been underestimated compared to actual working hours. To offset these limitations, various nurse departments were classified according to the level of work loading in previous studies, and job rank was also corrected in the statistical analysis. In this study, the question was asked about household income, not personal income, due to refusal to respond to personal information. Thus, there was a lack of understanding of the relationship between individual burnout and compensation.
Our results indicate that resilience and social support could be prevention factors for burnout. Increasing nurse resiliency is critical to improving the quality of patient care and reducing nurse burnout [36,37]. It is necessary to prevent burnout due to essential nursing work by examining resilience prior to assignment, by continuously monitoring relatively low groups, and/or by attempting an interactive program to reduce depression and increase resilience. Many studies have suggested ways to increase social support to prevent depression and burnout [38,39]. Hospital supervisor should recognize that social support affects mental and physical health, and consider how to maintain social support or form a support group by selecting a group with low social support among night shift nurses. This study is meaningful in that it examines items that require active intervention and support for burnout targeting night shift nurses who are indispensable for patient care.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Ji Sun Kim, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Young-Sun Min, Hwa-Young Lee. Data curation: Young-Sun Min, Kiseok Kim, Hwa-Young Lee. Formal analysis: Young-Sun Min, Ji Sun Kim. Funding acquisition: Hwa-Young Lee. Investigation: Hwa-Young Lee. Methodology: Soon-Chan Kwon, Inho Lee. Project administration: Hwa-Young Lee. Validation: Hwa-Young Lee. Writing—original draft: Young-Sun Min, Hyeon-Ah Lee, Ji Sun Kim, Jae Hyun Han. Writing—review & editing: Young-Sun Min, Hwa-Young Lee.
Funding Statement
This study was supported by the grants from the National Center for Mental Health Research & Education, the Seoul National Hospital, Republic of Korea (HM15C1113) and Soonchunhyang University Research Fund.