|
 |
- Search
| Psychiatry Investig > Volume 21(4); 2024 > Article |
|
Abstract
Methods
Results
Notes
Availability of Data and Material
All data generated or analyzed during the study are included in this published article (and its supplementary information files).
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Tao-Hsin Tung, Ching-Wen Chien, Ping Tao. Data curation: Zhu Liduzi Jiesisibieke, Ho-Shan Wei, Pei-En Chen. Formal analysis: Zhu Liduzi Jiesisibieke, Ho-Shan Wei. Methodology: Tao-Hsin Tung. Supervision: Tao-Hsin Tung. Writing—original draft: Meixian Zhang, Zhu Liduzi Jiesisibiek. Writing—review & editing: Meixian Zhang, Tao-Hsin Tung.
Funding Statement
None
Figure 2.
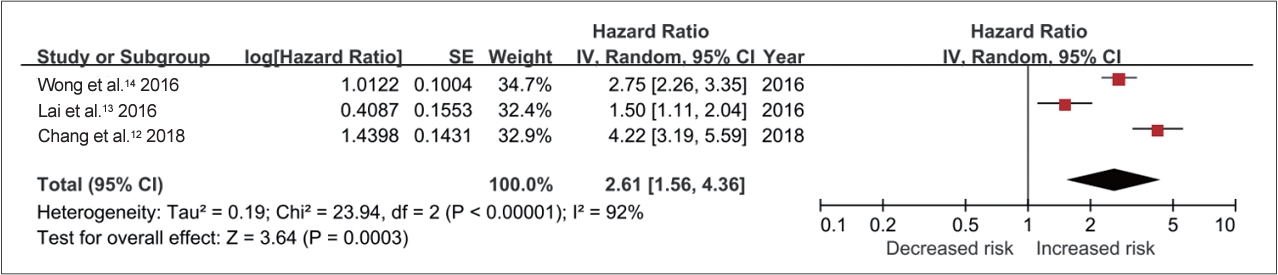
Figure 3.
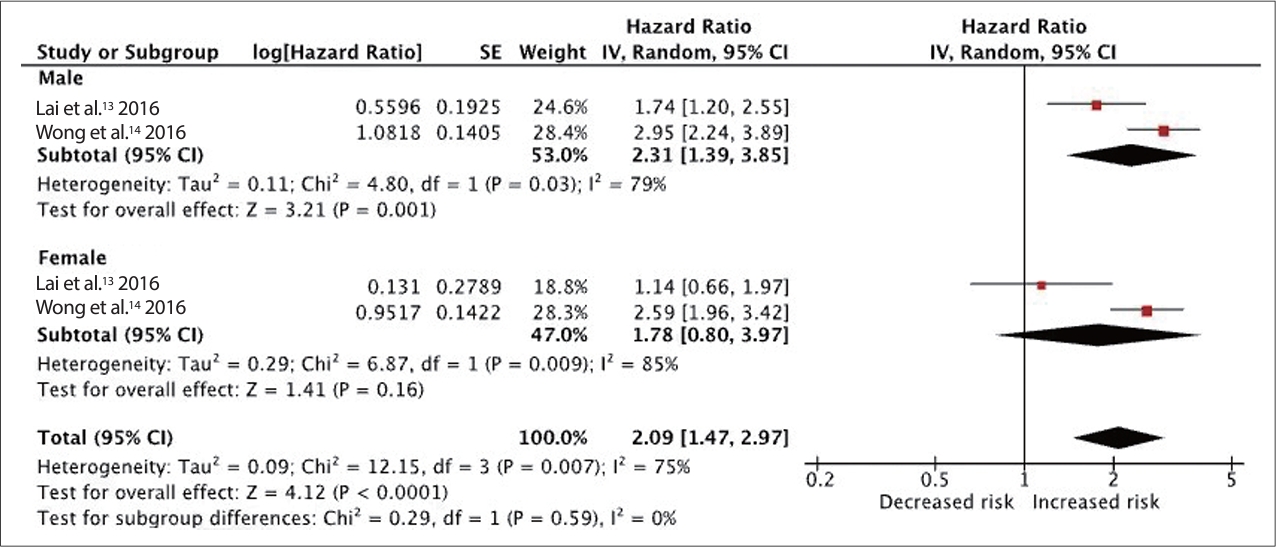
Figure 4.
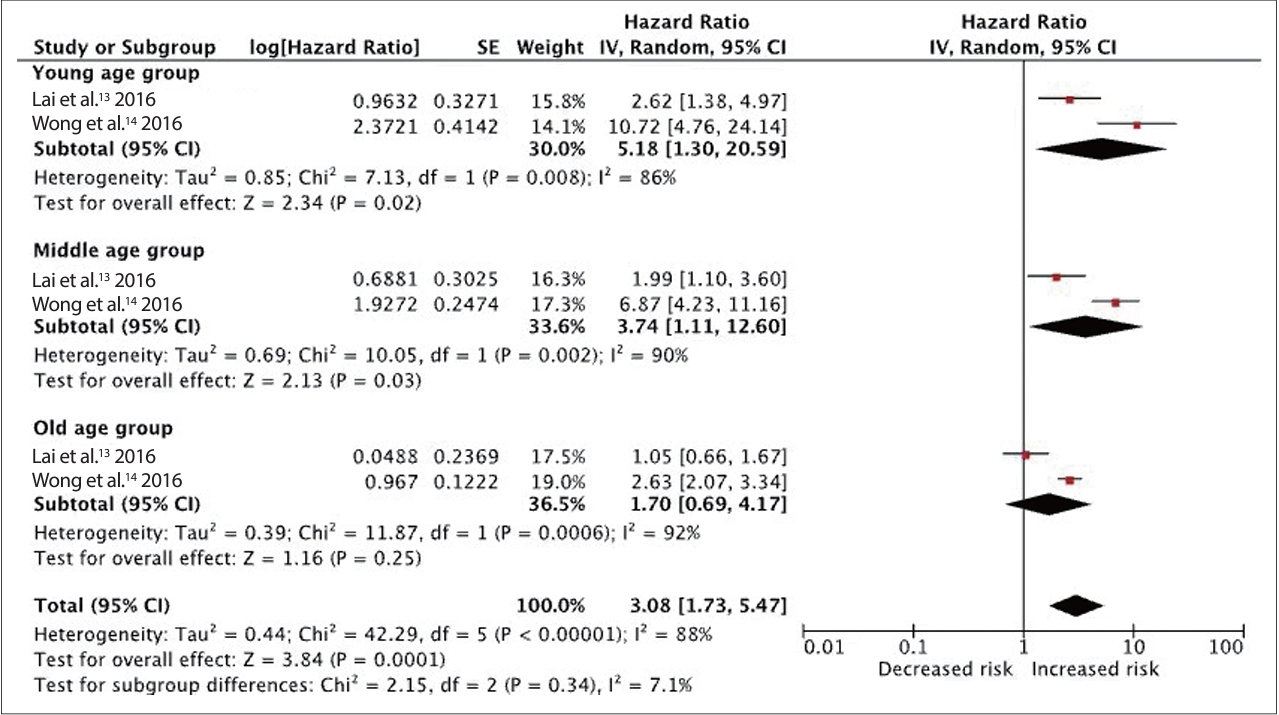
Table 1.
| Study, year, database used | Inclusion criteria | Subjects | Outcome measures | Study endpoint | NOS score | Effect size |
|---|---|---|---|---|---|---|
| Lai et al. [13] 2016 Taiwan’s NHIRD 2000-2011 | New inpatient patients diagnosed with CO poisoning (ICD-9-CM 986) | 4,103 patients with newly diagnosed charcoal-burning suicide attempts, 12,309 controls individual-matched by sex, age, and index year without charcoal-burning suicide attempts in a ratio of 1:3. | Dementia ICD-9-CM 290.0-290.4, ICD-9-CM 294.1, 331.0-331.2 | Diagnosis of dementia, death, withdrawal from the insurance program, or December 31, 2011 | S | HR: 1.50, 95% CI: 1.11-2.04 |
| C | ||||||
| O | ||||||
| Wong et al. [14] 2016 Taiwan’s NHIRD 2005-2010 | Inpatient and outpatient patients diagnosed with CO poisoning (ICD-9-CM 986, E868.8) | 14,590 patients with CO poisoning, 58,360 controls individual-matched by sex, age (±1 year), and index date without CO exposure in a ratio of 1:4 | Dementia ICD-9-CM 290.0-290.4, ICD-9-CM 294.1, 331.0-331.2 | Diagnosis of dementia, death, or December 31, 2013 | S | HR: 2.75, 95% CI: 2.26-3.35 |
| C | ||||||
| O | ||||||
| Chang et al. [12] 2018 Taiwan’s NHIRD 2000-2010 | ≥20 years Diagnosis of charcoal-burning suicide attempts (ICD-9-CM code: E952) | 9,041 adults newly diagnosed with CO poisoning, 36,160 controls frequencymatched by sex, age (every 5 years), and hospitalization year with non-CO poisoning in a ratio of 1:4 | Dementia ICD-9-CM 290.0-290.43, ICD-9-CM 290.8, 290.9, 331.0 | Diagnosis of dementia, withdrawal from the insurance program, or December 31, 2010 | S | HR: 4.220, 95% CI: 3.188-5.586 |
| C | ||||||
| O |
Scale domains: S, selection of study groups; C, comparability; O, outcome assessment. NHIRD, National Health Insurance Research Database; CO, carbon monoxide; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis codes; NOS, Newcastle-Ottawa Scale; HR, hazard ratio; CI, confidence interval
REFERENCES