Factor Structure of the Clinician-Rated Dimensions of Psychosis Symptom Severity in Patients with Schizophrenia
Article information
DSM-5 has proposed the use of the Clinician-Rated Dimension of Psychosis Symptom Severity (CRDPSS) for evaluating the various symptoms of schizophrenia.1 The 8-domain CRDPSS was developed from the perspective of deconstructing the psychopathology of schizophrenia and would be expected to provide baseline data for further advances in psychiatric nosology.2 In considering trends in psychiatric nosology, Panas3 has suggested that phenomenological Gestalt has faded into oblivion in the diagnostic criteria for schizophrenia and that psychiatric nosology has regressed to a pre-Kraepelinian state. To our knowledge, despite these discussions, the dimensional structure of the CRDPSS has hardly been studied.
We therefore aimed to identify the factor solution of the CRDPSS. As described elsewhere,4 166 in patients with schizophrenia (diagnosed with the DSM-5),5 age ≥18 years and ≤65 years, and length of hospital stay ≥2 weeks were recruited in Korea. Half were men (51.5%). Their mean age and age at onset were 46.5 (SD=11.2) and 25.2 (SD=13.2) years, respectively, and the mean chlorpromazine equivalent dose of antipsychotic prescriptions was 921.1 (SD=952.0) mg.
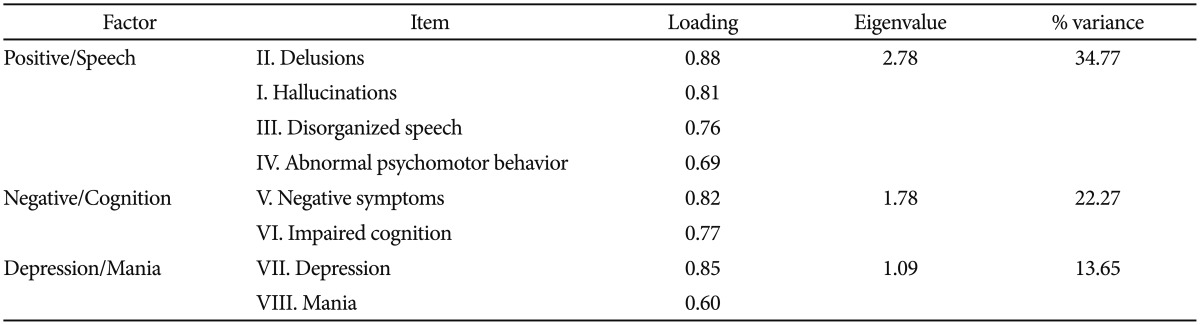
Mean scores on the hallucinations, delusions, disorganized speech, abnormal psychomotor behaviors, negative symptoms, impaired cognition, depression and mania were 2.04 (SD=1.30), 2.27 (SD=1.16), 1.62 (SD=1.35), 1.16 (SD=1.16), 2.01 (SD=1.24), 1.22 (SD=1.22), 0.51 (SD=0.70) and 0.19 (SD= 0.48), respectively. An exploratory factor analysis (EFA) was conducted on the CRDPSS, with principle components extracted by the varimax method. The number of factor in the solution was estimated on a scree plot, using eigenvalues >1.6 In addition, only a loading >0.40 was considered to reveal a clear factor structure and content. As a result, Bartlett's test for sphericity was significant [χ2 (166)=468.72, p<0.001], and the total variance of the factor solution was 70.69%. Table 1 gives the factor loadings for a three-factor solution. The first factor consists of the domains for delusions, hallucinations, disorganized speech and abnormal psychomotor behavior, and is designated "positive/speech". The second factor consists of the domains for negative symptoms and impaired cognition, and is named "negative/cognition". The third factor consists of the domains for depression and mania, and is designated "depression/mania". In addition, Pearson's correlations between the factor scores on the CRDPSS and the total and subscale scores on other measurement tools were obtained. Scores on the positive/speech factor were significantly correlated with scores on the positive symptoms subscale [Brief Psychiatric Rating Scale (BPRS)]7 (r=0.81, p<0.01), negative symptoms subscale (BPRS)7 (r=0.62, p<0.01), resistance subscale (BPRS)7 (r=0.44, p<0.01), Scale for the Assessment of Thought, Language and Communication (TLC scale)8 (r=0.64, p<0.01), Calgary Depression Scale for Schizophrenia (CDSS)9 (r=-0.32, p<0.01), Young Mania Rating Scale (YMRS)10 (r=0.58, p<0.01) and Clinical Global Impression of severity (CGI-S)11 (r=0.85, p<0.01). Scores on the negative/cognition factor were correlated with scores on the negative symptoms subscale (BPRS) (r=0.35, p<0.01), resistance subscale (BPRS) (r=0.38, p<0.01), TLC scale (r=0.40, p<0.01) and CDSS (r= 0.17, p=0.03), and scores on the depression/mania factor were correlated with scores on the psychological discomfort subscale (BPRS)7 (r=0.25, p<0.01), the CDSS (r=0.17, p<0.01) and the YMRS (r=0.81, p<0.01).
Our investigation has the virtue of pioneering research into the evaluation of patients with schizophrenia using the CRDPSS. In summary, it shows that the 8-domain CRDSS has a three-factor structure, consisting of positive/speech, negative/cognition and depression/mania factors. Pearson's correlations indicate that all three factors have favorable concurrent and divergent validity. Hence, our findings shed light on the heterogeneous symptom components of schizophrenia.
Acknowledgments
This research was supported by the 2015 Research Fund of the Korean Society for Schizophrenia Research.