Initial Psychometric Properties of the Korean Altman Self-Rating Mania Scale: Preliminary Validation Study in a Non-Clinical Sample
Article information
Abstract
Objective
We aimed to examine the reliability and validity of the Korean Altman Self-Rating Mania Scale (K-ASRM) in a large sample of Korean non-clinical undergraduates.
Methods
Participants (n=1,091) filled out the K-ASRM with other self-report questionnaires assessing bipolarity, mood symptoms and affect. Reliability test, exploratory factor analysis and correlation analyses were conducted to examine its psychometric properties.
Results
The reliability of the K-ASRM was adequate (Cronbach’s α=0.73, item-to-total correlation 0.53–0.78) and the exploratory factor analysis yielded one factor of mania. The K-ASRM demonstrated significant associations with measures of hypomanic personality (r=0.33), lifetime history of hypomanic symptoms (r=0.23). Also, the K-ASRM was significantly correlated with positive affect (r=0.53), negative affect (r=-0.17) and depressive symptoms (r=-0.35).
Conclusion
These results suggest preliminary possibility that the K-ASRM can be utilized as self-rating tool for mania in Korea as well as future directions for further validation.
INTRODUCTION
Is self-rating of mania reliable and valid?1 The obvious scarcity of mania self-rating scales reflects the common notion that mania cannot be measured by self-rating. To date, mania has been primarily measured by clinician rating scales such as Young Mania Rating Scale (YMRS),2 Bech-Rafaelsen Mania Rating Scale (MRS)3 or Clinician Administered Rating Scale for Mania (CARS-M).4 Lack of illness insight, uncooperative attitude of manic patients were mentioned as possible reasons why reliability and validity of self-report method could be hampered.
Recently, a few self-rating scales for mania have been developed and demonstrated promising results. The Internal State Scale (ISS) developed by Bauer et al.5 includes ‘activation’ subscale which constitutes core characteristics of mania. The Self-Report Manic Inventory (SRMI) is another self-report scale assessing mania.6 These scales evidenced concurrent validity with clinician rating scales of mania and scores of these scales could correctly classify manic patients against other psychiatric patient groups. Moreover, the finding that endorsing lack of insight item was not significantly related to self-reported symptom severity levels on the SRMI challenged the pre-existing notion that self-reporting of mania is unreliable. However, omission of prominent manic symptoms (e.g., decreased sleep, pressured speech) and absence of dropout information were discussed as limitations of these scales.7
Among the self-report scales for mania, the Altman Self-Rating Mania Scale (ASRM) is a 5-item questionnaire designed to assess the presence and/or severity of manic symptoms in accordance with the Diagnostic and Statistical Manual of Mental Disorders-fourth edition (DSM-IV) criteria.7 The ASRM comprises of 5 groups of statements asking how often respondents experienced elevated mood, increased self-esteem, less need for sleep, pressured speech and psychomotor agitationduring the past week. In the development study by Altman et al.7 the score of the ASRM demonstrated strong positive correlation of 0.7–0.8 with scores of the YMRS and the CARS-M. In addition, the score of the ASRM was sensitive to changes following treatment. Moreover, similar to the results obtained from the SRMI (c.f. although this study used subjective item of insight),6 whether manic patients had insight on the objective measure (item 15 on the CARS-M) did not differently influence theself-reported ASRM score, thereby suggesting appropriateness of the ASRM as self-report measure.
Since the ASRM is a very brief questionnaire which requires only a few minutes to complete, it possesses practical strength for screening and monitoring manic symptoms in either in/outpatient clinical settings as well as research settings.7 Also, good psychometric properties of the ASRM strengthen its utility as a self-rating measure of mania. The comparative superiority of the ASRM over other self-rating scales for mania (ISS, SRMI) has been reported by Altman et al.8 Basically, all three scales showed satisfactory reliability and validity but the ASRM outperformed in terms of screening patients in acute mania with brevity. In these regards, the ASRM has been widely utilized in a number of bipolar researches910111213 and it was recently recommended by the DSM-514 as self-report tool of manicsymptom severity.
To the best of our knowledge, there are even fewer self-rating options available for mania especially in Korea. At present, most validated self-report tools for mania or hypomania (e.g., Mood Disorder Questionnaire, Hypomania Checklist-32, Bipolar Spectrum Diagnostic Scale) are screening instruments.151617 Since these instruments were developed to sensitively detect under-recognized bipolar patients primarily in patients with depressive episodes, they cannot be used to measure current symptom severity. Of exception, Cha et al.18 developed the Patient Mood Chart (PMC), which is an adapted version of the Prospective Life-Chart Method (LCM-P).19 In this development study, manic symptoms ratings on this mood chart showed significant correlation of 0.7–0.8 with the YMRS. However, the main purpose of the PMC was to monitor mood symptoms on a daily basis and the format is somewhat different from other self-report scales of mania.
The main objective of this study is to test reliability and validity of the Korean version of ASRM (K-ASRM) in large non-clinical samples of undergraduates as a preliminary step of validation. To this end, the internal consistency, factor structure and correlation of the K-ASRM with theoretically-relevant constructs were examined. Given that the ASRM intends to assess mania, the K-ASRM was expected to show positive correlation with hypomanic personality, lifetime history of hypomanic symptoms and positive affect. On the other hand, the K-ASRM was expected to demonstrate negative correlation with negative affect and depressive symptoms.
METHODS
Participants
In total, 1,091 Korean undergraduates from 3 universities located in Seoul and Gyeonggi Province participated in this study (54% female, mean age=20.58). All procedures and materials were approved by the Institutional Review Board (IRB) and informed consent was obtained prior to participation. Study participants received credits for completing the questionnaires as partial fulfillment of undergraduate psychology course requirements.
Measures
The Korean Altman Self-Rating Mania Scale
The K-ASRM is a 5-item self-report questionnaire to assess the presence and/or severity of manic symptoms (elevated mood, increased self-esteem, less need for sleep, pressured speech and psychomotor agitation) over the past week. In the beginning of the original scale construction, 14 groups of statements were contained.7 Subsequently, the principal component analysis (PCA) of the 14 items revealed 3 separate factors-mania, psychosis and irritability. Given that the other 2 factors (psychosis, irritability) failed to distinguish manic from non-manic patients, these items were excluded in the final scale. Finally, the 5 items comprising mania factor were chosen. Each item is scored on the 5-point Likert scale (0=absent to 4=present to a severe degree). Total scores range from 0 to 20, with higher scores indicating the presence of more severe manic symptoms.
Permission for validation was obtained from the original author, Dr. Altman (personal communication, March 24, 2015). The first author translated the English items into Korean and a bilingual person checked if the meaning of translated items matched the original contents (Supplementary Material in the online-only Data Supplement).
The Hypomanic Personality Scale
The HPS is a 48-item self-report questionnaire, developed by Eckblad and Chapman20 to identify individuals at risk for bipolar disorder. Each item is answered on the true-or-false format and contents of the items include episodic fluctuations in affect, behavior and energy level. Reliability and validity of the HPS were widely tested in numerous studies.212223242526 Among them, Kwapil et al.23 showed that high scorers of the HPS reported more bipolar disorders and major depressive episodes than the control group in the 13-year-follow up to demonstrate predictive validity. Recently, high scorers on the HPS is considered to belong to the softer spectrum of bipolar disorder.2427 Korean version of the HPS was translated by Kim and Oh28 and Cronbach's α in this study was 0.85.
The Hypomanic Symptom Checklist-32
The HCL-32 is a 32-item self-report screening tool for hypomania, developed by a group of international bipolar researchers29 to increase the detection of bipolarity among depressed patients. Sensitivity and specificity of the HCL-32 were examined in the receiver-operating characteristic (ROC) curve analysis and the total score is shown to discriminate bipolar patients from unipolar depression patients.29 It is not appropriate to use the HCL-32 for screening purpose in non-clinical samples.3031 We chose this scale not to screen but to measure lifetime history of hypomanic symptoms, based on the fact that the HCL-32 adopted a dimensional view of bipolarity in construction and that previous studies showed that the factor structure is fairly similar in clinical and non-clinical samples.2931 Korean version of the HCL-32 was translated and validated by Oh et al.16 and Cronbach's α in this study was 0.80.
Positive and Negative Affect Schedule
The PANAS is developed by Watson et al.32 and comprises of 10 positive-affect and 10 negative-affect items. This scale was constructed on the empirical and conceptual basis that positive and negative affect emerge as two dominant and relatively independent dimensions.32 Each item is rated on the 5-point Likert scale. Korean version of the PANAS was validated by Lee et al.33 and Cronbach's α in this study was 0.86 for positive, 0.90 for negative affect.
Center for Epidemiologic Studies Depression Scale
The CES-D is a 20-item self-report questionnaire, developed by Radloff34 to assess the severity of behavioral, somatic and cognitive symptoms of depression. The Korean version of the CES-D was validated by Chon et al.35 and Cronbach's α in this study was 0.90.
Statistical analysis
To verify reliability, internal consistency (Cronbach's α) and item-to-total correlations were computed. Exploratory factor analysis (EFA) was performed to explore the factor structure. In the original development study, Altman et al.7 performed the PCA to extract the mania factor; however, they did not exactly carry out factor analysis. In those days, the PCA and factor analysis were interchangeably used in some studies; however, nowadays it is increasingly recognized that those methods have separate statistical assumptions and implications.36 Strictly speaking, the PCA is a means of data reduction by extracting ‘component’; whereas, factor analysis is used in order to derive latent construct, ‘factor’ from manifest variables. In the EFA of the K-ASRM, principal axis factoring extraction extraction was used and the minimum threshold for a significant factor loading was defined 0.30 and above.37 Afterwards, correlation analyses with other questionnaires (HPS, HCL-32, CES-D, PANAS) were carried out to demonstrate the convergent validity of the ASRM.
Data were analyzed using the SPSS 18.0 and statistical significance was defined at 0.05 level. The whole sample (n=1,091) was divided into two groups, because the first group answered only the K-ASRM and the second group completed the other questionnaires along with the K-ASRM. Data from the first group (n=536) was used for reliability test and exploratory factor analysis. Correlation analyses were performed using the data from the second group (n=555). There was no significant group difference in demographic variables.
RESULTS
Reliability
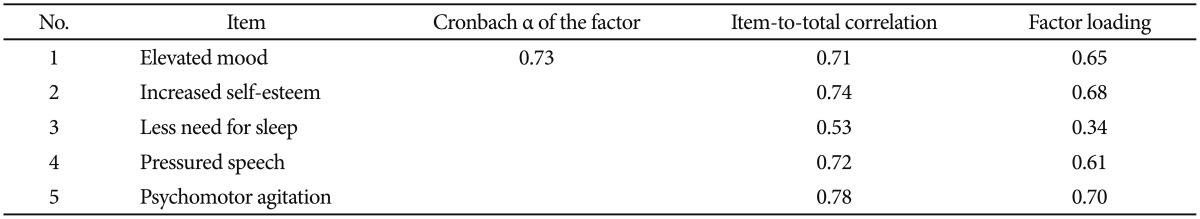
As can be seen in the Table 1, internal consistency the K-ASRM was appropriate (Cronbach's α=0.73), which was comparable to that of the original version (Cronbach's α=0.79; Altman et al.7). In addition, the range of the item-to-total correlation was from 0.53 (item 3) to 0.78 (item 5) and all of the correlations were significant at p<0.01 level.
Exploratory factor analysis
In order to explore factor structure of the K-ASRM, EFA of all the five items was conducted. The Kaiser-Meyer-Olkin (KMO) of sampling adequacy was 0.7638 and the Bartlett's test of sphericity was significant, χ2 (10, n=536)=565.49, p<0.0001, indicating a high level of inter-item correlation required for factor analysis.
In determining the number of factor, the following three criteria were applied. Firstly, in terms of theoretical interpretability, the five items were constructed to represent uni-factor of mania.7 In addition, both the rule of the Eigen value ≥1.0 and the scree plot analysis also supported the existence of one factor in the K-ASRM. Therefore, the number of factor was determined as one and the factor was extracted via principal axis factoring. The results of the EFA are reported in the Table 1. All items loaded on the factor ‘mania’ and the range of factor loading was 0.34–0.70, p<0.01.
Descriptive statistics
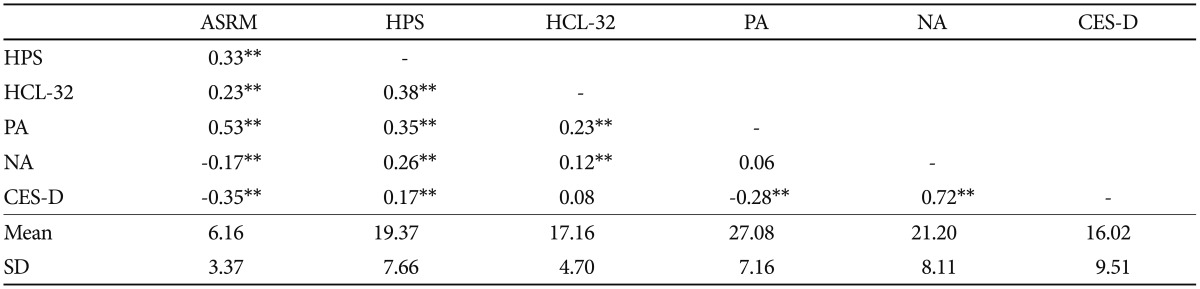
Prior to correlation analyses, descriptive statistics of the K-ASRM and other questionnaires were computed (Table 2). There was no gender difference in the scores of K-ASRM, CES-D, HPS, HCL-32 and NA subscale of the PANAS (p>0.05). The only gender difference emerged in the PA subscale of the PANAS and male participants tended to show higher PA scores (t=3.36, p<0.01), which is in line with previous reports.39
In addition, in order to describe sample characteristics, distribution of the CES-D and HCL-32 scores were examined. Results showed that 43.6% of participants belonged to the ‘probable depression‘ range (CES-D≥16) and 17.6% were classified as ‘definite depression’ (CES-D≥25).40 Considering that the prevalence estimates on the CES-D peaks around the age from 16 to 19 in Korea (46.8% for probable depression, 22.7% for definite depression),41 these somewhat high estimates from undergraduate samples in young adulthood (mean age=20.58) seem understandable. In regard of the HCL-32, there are previous investigations suggesting that not sum score but ‘duration’ and ‘presence of impairment’ items may be more informative in non-clinical samples to identify ‘probable hypomania’ group.3031 Taking this recommendation into account, 4.6% of the participants belonged to probable hypomania group.a, This estimate corresponds to the recent report that prevalence rate of wider bipolar spectrum including bipolar not otherwise specified (NOS), cyclothymia is approximately 4.4% in general population.42
Convergent validity
Correlation analyses were performed to explore the relationship between the K-ASRM and other relevant variables (Table 2). As expected, the K-ASRM correlated positively with adjacent constructs of bipolarity. The K-ASRM was significantly associated with both hypomanic personality and lifetime history of hypomanic symptoms (r=0.33, r=0.23, p<0.01, respectively). Also, the K-ASRM had considerable positive association with positive affect (r=0.53, p<0.01). Conversely, the K-ASRM showed negative associations with negative affect and depressive symptoms (r=-0.17, r=-0.35, p<0.01, respectively), as expected.
DISCUSSION
The ASRM is a brief yet psychometrically-sound self-rating scale of mania, recommended by the DSM-5.14 The present study is the first report of psychometric properties of the K-ASRM. The K-ASRM had adequate internal consistency and one-factor structure. In addition, the K-ASRM was significantly associated with measures of bipolarity, depressive symptoms and affect in the expected direction. Taken together, these results indicate that the K-ASRM possess reliability and preliminary validity.
However, in a sense, the results of this study should be deemed a preliminary step of validating the K-ASRM. These results should be interpreted within some limitations that also suggest future directions for further validation of the K-ASRM. Firstly, we used only non-clinical samples and demographic variables other than gender, age were not collected. Usage of large non-clinical sample has practical advantage to increase statistical power and can be justified as entry point in the validation process. But it is necessary to emphasize that these results from non-clinical sample should be cautiously interpreted, because the original ASRM was developed for use in clinical samples and its clinical utility in general population has not been empirically tested yet. Therefore, it is not certain whether the items derived from the response of bipolar patients actually tap the identical concept, ‘mania’ in non-clinical samples as well. For example, item 1 (elevated mood) asks if one felt happier or more cheerful than usual. Shall this item be perceived in the same manner by non-clinical participant to signify pathological mood elation rather than normal happier mood? In this regard, we cannot conclude with confidence that the scores of the K-ASRM has equivalent meaning in measuring mania at this stage. Strictly speaking, the validity of the K-ASRM as mania self-rating remains half-answered until results from bipolar sample supplement the aforementioned gap.
Therefore, next step of the validation process should be recruiting a well-defined clinical sample of bipolar disorder patients along with other major psychiatric control group. Validation study in clinical samples would allow one to test not only reliability, validity but also feasibility of the K-ASRM asmania self-rating; that is, if in/outpatients can actually self-report their manic symptoms following the instruction. After data in clinical samples are obtained, optimal cutoff score of the K-ASRM should be analyzed to aid its interpretation in clinical and research settings.
Secondly, the present study can be criticized for entire reliance on self-report measures. In particular, in order to verify the concurrent validity of the K-ASRM, clinician rating scales of mania such as YMRS, MRS or CARS-M should be utilized in the future researches in clinical samples. It should be directly examined if scores of the K-ASRM well correspond to other clinician rating scales of mania. Thirdly, the cross-sectional design of the present study limits the chance of examining sensitivity-to-change issue. It is necessary to examine if the K-ASRM is sensitive to change in manic symptoms following treatment.
Lastly, in terms of coverage, one can argue that the K-ASRM does not fully encompass a wide range of manic symptoms. Since the K-ASRM has only 5 items, its brevity has both advantages and disadvantages. Previous investigations indicated that mania is a multifaceted construct composed of distinct factors,43 and factor analyses of hypomania revealed dual structure of bright side (active/elated factor) and dark side (irritable irritable/risk-taking factor).44 According to this distinction, it is true that the item contents of the K-ASRM mainly pertain to the bright side.b Therefore, in using the K-ASRM, one should be aware of the limitation that this measure may overlook the dark side of mania.
Nevertheless, this study is meaningful to provide the initial psychometric properties of the K-ASRM. Although it was common to measure the severity of manic symptoms through clinician-rating interviews, recently-developed self-report measures demonstrate promising psychometric support.12 If adequate psychometric support is warranted, self-report method has practical advantages, which can contribute to research and clinical practice. Self-report method is less time and effort-consuming than clinician ratings. Therefore, self-reports can be easily used in cases of initial mass screening and repeated symptom monitoring. Also, self-reports can be used as adjunct assessment to clinician-ratings so as to capture subjective experience of respondent. We hope that the current study could serve as the first step of validation so that the K-ASRM can be utilized as valid self-report measure of manic symptom in Korea in the near future.
Notes
aMeyer et al.31 defined ‘probable hypomania’ as reporting highs that lasted at least 4 days and that accompanied negative consequences. However, it is a common notion that hypomania is not necessarily experienced as being negative and it can be subjectively perceived to be even positive. Therefore, we adapted the probable hypomania criteria: (a) lasting at least 4 days, (b) presence of functional change whether it is either negative or positive.
bIn these regards, it is understandable that the positive association of the K-ASRM is stronger with the positive affect (r=0.53) than with hypomanic personality (r=0.33) or lifetime history of hypomania symptoms (r=0.23) which include both bright and dark sides of hypomania. We thank the anonymous reviewer for providing extended view of our results.
References
Supplementary materials
The online-only Data Supplement is available with this article at https://doi.org/10.4306/pi.2017.14.5.562.
Supplementary Material
Korean Altman Self-Rating Mania Scale