Effect Modification of Cortisol on the Associations Between Obsessive-Compulsive Symptoms on Suicidality in Patients With Acute Coronary Syndrome
Article information
Abstract
Objective
Obsessive-compulsive symptoms (OCS) and suicidal ideation (SI) are common in patients with acute coronary syndrome (ACS). This study investigated the associations of OCS and serum cortisol levels with SI, and further evaluated the possible modifying effects of cortisol on the associations between OCS and SI in acute and chronic phases of ACS.
Methods
In total, 969 ACS patients were recruited from a tertiary university hospital in Korea within 2 weeks of disease onset and evaluated in terms of OCS (using the OCS dimension of the Symptom Checklist-90–Revised), serum cortisol levels, and SI (using the “suicidal thoughts” item of the Montgomery–Åsberg Depression Rating Scale). Covariates included sociodemographics, depression, vascular risk factors, and disease severity. After 1 year, 711 patients were re-evaluated in terms of SI. Logistic regression analysis was performed with adjustment for covariates.
Results
Higher OCS was significantly associated with SI both at baseline and follow-up. Serum cortisol showed no such association, but modified the association between OCS and SI. That was the associations were significant only in the higher but not in the lower serum cortisol levels, with significant interaction terms after adjusted for relevant covariates.
Conclusion
Evaluating OCS and serum cortisol levels at the acute phase could improve the accuracy of clinical predictions of SI both in the acute and chronic phases of ACS.
INTRODUCTION
Acute coronary syndrome (ACS) is composed of a various range of clinical symptoms from ST-segment elevation myocardial infarction (STEMI) to non-STEMI or unstable angina [1]. ACS is a leading cause of morbidity and mortality in most countries with a significant burden on healthcare resources [2]. Patients with acute life-threatening physical diseases including ACS are at a significantly increased risk for suicidality [3,4]. Suicidal ideation is a prerequisite of more serious suicidal behavior including suicidal attempt or death but could be a treatment mark with pertinent detection [5]. Identifying possible risk factors of suicidality might be the beginning measure.
The etiology of suicidal behavior is multiple and heterogeneous, and diverse bio-psycho-social elements have been evaluated in connection to suicide risks [6-9]. Of the psychosocial factors, obsessive-compulsive symptoms (OCS) or disorder (OCD) increased significantly the odds of having a lifetime suicidal ideation and attempts as compared to the general population [10,11]. These close relationships between OCS/OCD and suicidality have been confirmed by a recent systematic review, and have indicated a common biological basis [12]. Cortisol is a major and effector hormone in the stress-response system via the hypothalamus-pituitary-adrenal (HPA) axis, and therefore has long been received particular research attention [13-15]. Cortisol plays an important role both not only in suicidality but also in OCS/OCD, hence it may be a candidate for the common biological link. Although impaired HPA axis activity and increased circulating levels of cortisol are not consistently found across OCS/OCD studies [16,17], a recent meta-analysis concluded that cortisol levels are significantly higher in OCS/OCD patients than healthy individuals [18]. Based on these lines of evidence, it could be postulated that higher rates of suicidal behavior in relation to OCS/OCD are possibly mediated by altered cortisol activity. However, to our best knowledge, this hypothesis has not been investigated. Moreover, the roles of OCS/OCD and cortisol on suicidal behavior have not been formally tested in patients with ACS, who are at high risks of both OCS/OCD [19] and suicidal behavior [3,4].
To bridge the research gap, we hypothesized that cortisol might modify the impacts of OCS on suicidal behavior in patients with ACS. Using data from a prospective Korean cohort with ACS, we investigated associations of OCS and serum cortisol levels measured in the acute phase of ACS with suicidal ideation evaluated in both the acute and chronic phases, and then evaluated the potential modifying effects of serum cortisol levels on the association between OCS and suicidal ideation.
METHODS
Study overview and participants
The present analyses were carried out using data from a larger naturalistic prospective observational study of patients with ACS—the Korean Depression in ACS study—which were to investigate the prevalence, risk factors, and longitudinal course of mental disorders in survivors of recently developed ACS [20]. In summary, patients with recent ACS were approached at the Department of Cardiology of Chonnam National University Hospital, Gwangju, South Korea from 2006 to 2012 and invited to participate in this study. Participants who met the eligibility criteria (Supplementary Materials in the online-only Data Supplement) and agreed to participate were examined as inpatients at the baseline evaluation within 2 weeks (acute phase) of ACS onset. Follow-up assessments were performed as outpatients at 1 year thereafter (chronic phase) of ACS. OCS and serum cortisol levels were estimated at baseline, and suicidal ideation was evaluated in both phases. This study was approved by the Chonnam National University Hospital Institutional Review Board. All participants reviewed the consent form and provided written informed consent (IRB No.06-026).
OCS
OCS were evaluated using the Symptom Checklist-90–Revised (SCL-90-R) [21]. This is a self-administered 90-item questionnaire consisting of multiple-choice questions with a 5-point (1–5) scale of distress, ranging from “not-at-all” to “extremely distressed.” The OCS dimension of the SCL-90-R consists of 10 of the total 90 items. The SCL-90-R is used widely in clinical situations and in research because of its appropriate design for use in individuals with medical conditions [18] including cardiac disorders [22,23]. The time frame of the OCS measure was the most recent one week after ACS, as recommended by the scale developer. Since there have been no validated cutoffs published to categorize the severity of OCS, scores on the OCS dimension of the SCL-90-R were dichotomized at the median value into lower vs. higher OCS groups. Although this classification was arbitrary, it has been used in previous studies [24].
Serum cortisol levels
Based on psychobiological assumptions regarding HPA dysregulations in stress-related disorders [25,26], as well as findings from prior studies conducted by our own workgroup [27] and other researchers [28] we posited that subgroups of patients could be identified based on their unstimulated cortisol levels. Participants were fasted from the night before the morning blood sampling. They were asked to quietly relax before sample collection. Serum cortisol levels were measured using the Elecsys Cortisol II assay (Roche Diagnostics GmbH, Mannheim, Germany) at the Global Clinical Central Lab (Yongin, South Korea). Based on the median cortisol levels, participants were divided into low- vs. high-cortisol groups for analysis. Given the lack of an absolute cutoff value for cortisol levels and the goal of maximizing statistical power by increasing the number of patients in both groups, we divided the two groups based on the median cortisol value, as we have previously done in a similar study [27].
Suicidal ideation
Suicidal ideation was identified using the “suicidal thoughts” item of the Montgomery–Åsberg Depression Rating Scale (MADRS-ST) [29], which consists of 10 items ranked for severity on an ordinal scale ranging from 0 to 6. The MADRS is used extensively globally in clinical research to assess the severity of depression, and has good reliability and validity. The “suicidal thoughts” item assesses the feeling that life is not worth living and plans for suicide, with scores ranging between 0 (life satisfaction) and 6 (explicit plans for suicide). Suicidal ideation was considered to be present if the patient scored ≥2, where a score of 2 reflected fleeting suicidal thoughts, following previous studies [30,31].
Baseline covariates
Sociodemographic characteristics of interest included age, sex, duration of education, living status (living alone or not), housing status (owned or rented), and current occupation (employed or not). Depression-related characteristics included previous and family history of depression, and current Diagnostic and Statistical Manual of Mental Disorders, 4th edition depressive disorder [32]. The following vascular risk factors were evaluated: previous and family history of ACS or stroke, diagnosis of hypertension or diabetes mellitus, hypercholesterolemia (defined as fasting serum total cholesterol >200 mg/dL), obesity (defined as body mass index >25 kg/m2), and current smoking status. To evaluate current cardiac status, ACS severity was estimated using the Killip classification [33], the left ventricular ejection fraction was estimated based on echocardiography results, and the serum cardiac biomarkers troponin I and creatine kinase-MB were measured.
Statistical analyses
Baseline covariates were compared according to OCS and suicidal ideation at baseline and follow-up using Student’s t-tests or χ2 tests, as appropriate. Covariates for further adjusted analyses were selected from among the characteristics significantly associated with OCS and suicidal ideation (p<0.05), and other variables with potential effects on suicidal behaviors [5,30], with consideration of the potential for collinearity between the variables. Correlations between OCS and serum cortisol levels were estimated by using Spearman’s rho. The individual associations of OCS (lower vs. higher scores) and serum cortisol (lower vs. higher levels) with suicidal ideation were analyzed at both baseline and follow-up using logistic regression models, before and after adjusting for covariates. Modifying effects of serum cortisol levels on the associations of OCS with suicidal ideation were analyzed using multinomial logistic regression with adjustment for the same factors. All statistical tests were two-sided, with a significance level of p<0.05. Statistical analyses were performed using IBM SPSS 27.0 software (IBM Corp., Armonk, NY, USA).
RESULTS
Recruitment
Participant recruitment process and prevalence rates of suicidal ideation are shown in Supplementary Figure 1 (in the online-only Data Supplement). Of 1,152 ACS patients met the eligibility criteria, 969 (84%) agreed to offer blood samples and comprised the baseline sample. No significant differences in any baseline characteristics were found between those who agreed to blood collection and those who refused (all p>0.15). Of these, 711 (73%) who were successfully re-evaluated 1 year later comprised the follow-up sample. Older age and higher Killip class contributed the attrition between 258 patients lost to follow-up and those who followed-up (all p<0.05).
Baseline characteristics by OCS and suicidal ideation
Median (interquartile range [IQR]) and mean (standard deviation [SD]) scores of the OCS dimension of the SCL-90-R were 13.0 (11.0–15.0) and 13.9 (4.1), respectively. Baseline characteristics were compared according to the lower (<13) vs. higher (≥13) OCS scores in the Table 1. Higher OCS scores were significantly associated with current unemployment and present clinical depression. Suicidal ideation was present in 195 (20.1%) and 87 (12.2%) patients with ACS at baseline and follow-up, respectively. The baseline characteristics of patients with and without suicidal ideation at baseline and follow-up are listed in Supplementary Table 1 (in the online-only Data Supplement). Suicidal ideation at baseline was significantly associated with female sex, lower education level, rented housing, current unemployment, and previous and present depression, whereas suicidal ideation at follow-up was significantly associated with female sex, family history, and present depression. Considering these and previous findings [5,30], and the collinearity between variables, 10 covariates were selected for subsequent adjusted analysis: sex, education, housing, current employment, previous and family history of depression, present clinical depression, hypertension, diabetes, and serum troponin I levels.
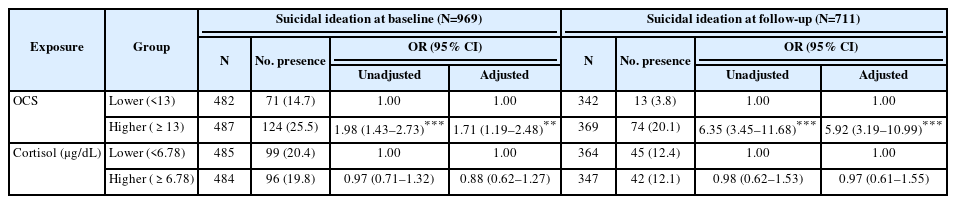
Individual associations with suicidal ideation
Median (IQR) and mean (SD) levels of the serum cortisol were 6.78 (3.60–12.06) and 8.1 (5.5), respectively. Serum cortisol levels were significantly correlated with OCS scores (Spearman’s rho=0.063; p=0.045). The individual associations of the lower (<13) vs. higher (≥13) OCS scores and lower (<6.78 μg/dL) vs. higher (≥6.78 μg/dL) cortisol levels with suicidal ideation are described in Table 2. Higher OCS scores were significantly associated with suicidal ideation at baseline and at follow-up before and after adjustment. No association was found between serum cortisol levels and suicidal ideation before or after adjustment (all p>0.3).
Modifying effects of serum cortisol
The modifying effects of serum cortisol on the association between OCS and suicidal ideation at baseline and follow-up are shown in Figure 1. Higher OCS scores were significantly associated with suicidal ideation at baseline in the presence of higher cortisol levels but in that of lower cortisol levels with significant interaction terms after adjustment. Higher OCS score were significantly associated with suicidal ideation at follow-up regardless of serum cortisol levels. However, the strengths of the associations were more severe in the higher than in the lower cortisol levels with significant interaction terms after adjustment.
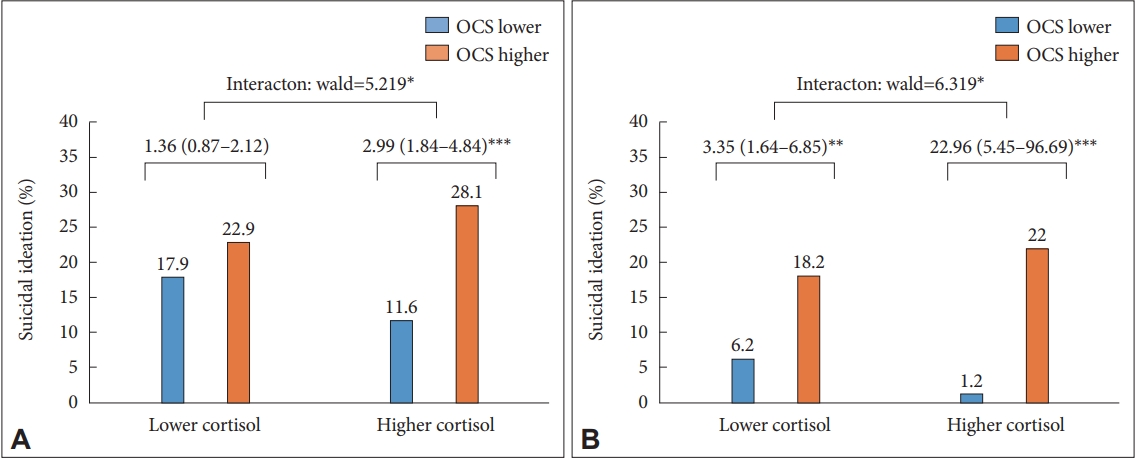
Modifying effects of serum lower vs. higher cortisol levels on the associations between obsessive-compulsive symptoms (OCS) at baseline and suicidal ideation both at baseline (N=969) (A) and at follow-up (N=711) (B) in patients with acute coronary syndrome. Data are odds ratios (95% confidence intervals) adjusted for sex, education, housing, current employment, previous and family history of depression, present clinical depression, hypertension, diabetes, and serum troponin I levels. *p<0.05; **p<0.01; ***p<0.001.
DISCUSSION
In this longitudinal study of ACS patients, OCS were significantly associated with suicidal ideation at baseline and at follow-up. Although serum cortisol levels were not associated with suicidal ideation, it modified the impacts of OCS with suicidal ideation both at baseline and at follow-up in that the associations were significantly more strengthened in the higher than in the lower serum cortisol levels with significant interaction terms after adjustment for relevant covariates.
OCS/OCD have been consistently associated with suicidal behaviors in various populations [12]. Particular OCS such as unacceptable thoughts on aggressive, sexual, or religious obsessions may be associated with increased suicidality [34]. Our findings supported the well-known associations even in these patients with ACS both at acute and chronic phases. Particularly, OCS rather than a formal diagnosis of OCD were used for exposure variables, but subjective OCS shown significant associations with suicidal ideation. The strengths of the observations were remained significant after adjustment for relevant covariates including depressive variables. Our novel results underscore the importance of evaluating OCS in the early stage of ACS considering its associations with suicidal ideation both at acute and chronic phases.
A main model of suicidality is a stress-diathesis component which states that suicidal behavior is a result of an interaction between acutely stressful events and a susceptibility to suicidal behavior (a diathesis) [6]. Since cortisol is a major hormone in the stress-response system, it has been widely investigated as a potential biomarker of suicidality [15]. In this study, there were no significantly associations between serum cortisol levels and suicidal ideation. Discrepancy in study population (general population vs. ACS patients) and suicidality definition (suicidal attempt vs. suicidal ideation) might account for the different observations. In addition, a meta-analysis reported an age specific association in that the associations between cortisol and suicidality were significant in the sample with age less than 40 years but were not in that with age 40 years or over. Since the mean (SD) age of this study was 58.2 (11.1) years, our negative findings were in keeping with the meta-analytic results.
Despite of no direct influence, significant modifying effects of serum cortisol levels were found on the associations between OCS and suicidal ideation. Several pathophysiological mechanisms are plausible. First, based on the stress-diathesis model, the negative impacts of OCS (stress) could be aggravated in the presence of higher cortisol levels (diathesis) on suicidal ideation in these participants. Second, the possible relationship between cortisol and OCS might be considered. That was, cortisol levels were significantly correlated to OCS in this study, consistent with previous investigations on the connections between HPA system and OCD [18]. Consequently, the two adverse status arisen from mutual influences might have synergy effects on suicidality. Third, cortisol has been considered as a common biomarker for both OCS and suicidality [12,18].
The limitations of this study were as follows. First, OCS rather than the diagnosis of OCD were used as an exposure variable. OCS are less formal than OCD for classifying the abnormal state, thus this classification may have led to overestimates of the strength of the association. A transdiagnostic approach, which focuses on common symptoms and processes across different diagnostic categories, has recently emerged and takes into account the complexity and multi-faceted nature of mental health problems [35]. By targeting the underlying mechanisms that contribute to the development and persistence of OCS, a transdiagnostic approach has the potential to lead to more effective and efficient treatment and management strategies. For example, cognitive-behavioral therapy is often used to treat OCS by focusing on changing negative thought patterns and behaviors [36]. Second, the primary outcome variable was suicidal ideation; although suicidal ideation is closely related to more severe suicidal behavior [5], no data concerning suicidal attempts or death were acquired. However, previous researches of patients with ACS or other severe somatic diseases also used suicidal ideation as a phenotype, because more severe forms of suicidal behavior are scarce in this kind of study [37,38]. Third, suicidal ideation was recognized via the “suicidal thoughts” item of the MADRS not by a specific instrument. However, this measure was used in previous studies of patients with severe somatic diseases [37]. Moreover, a recent study asserted that a depression rating scale item related to suicidal thoughts had good validity [39]. Fourth, recruitment was conducted at a single hospital, which may limit the generalizability of our findings; while, this may also be a strength as it increased the consistency and reliability of the evaluations. Finally, the older age and higher Killip class were significantly associated with no followed-up at 1-year. This suggested that more severe ACS pathology may be related to attrition, which could reduce the statistical significance. However, there were no significant differences in any other baseline characteristics, including suicidal ideation, between those who exited and those followed-up.
Our study had several strengths. Participants were recruited consecutively from among all eligible patients with recent ACS, which reduced the risk of error arising from sample heterogeneity. Evaluations at baseline and at follow-up were conducted similar time points, which improved the consistency of observations. All measurements of psychiatric and cardiovascular status were well validated, and a range of covariates was considered in the analyses.
In conclusion, we found that higher cortisol levels at baseline strengthened the widely known association between OCS and suicidal ideation both at acute and chronic phases of ACS. With respect to pathophysiology, our findings provide understanding into the pathogenic effects of OCS on suicidality, suggesting a modifying role of cortisol. In clinical practice, the prediction of suicidality could be enhanced by evaluating OCS and serum cortisol levels in the acute phase of ACS. Because ACS in a principal cause of morbidity and mortality, this procedure could significantly diminish the disease burden. This is particularly important in cardiovascular clinics because interviews to evaluate suicidality can be difficult for untrained clinicians, and OCS/OCD are common in patients with ACS compared to healthy subjects [19]. Our study represents an important first step toward fully explaining the modulatory role of cortisol in the association between OCS and suicidality. Future multi-center studies in other settings are needed to confirm the generalizability of the present findings.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2023.0085.
Eligibility criteria for patients with acute coronary syndrome (ACS)
Baseline characteristics by suicidal ideation (SI) status in patients with acute coronary syndrome (ACS)
Recruitment process and prevalence of suicidal ideation (SI) in participants with acute coronary syndrome (ACS).
Notes
Availability of Data and Material
The data that support the findings of study are available from the corresponding author (J-M Kim) upon reasonable request.
Conflicts of Interest
Jae-Min Kim declares research support in the last 5 years from Janssen and Lundbeck. Sung-Wan Kim declares research support in the last 5 years from Janssen, Boehringer Ingelheim, Allergan and Otsuka. Also, Sung-Wan Kim and Jae-Min Kim, a contributing editor of the Psychiatry Investigation, were not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: all authors. Data curation: Jae-Min Kim. Formal analysis: Hee-Ju Kang, Jae-Min Kim. Funding acquisition: Jae-Min Kim. Investigation: Sung-Wan Kim, Il-Seon Shin, Youngkeun Ahn, Myung Ho Jeong, Jae-Min Kim. Methodology: Wonsuk Choi, Ju-Yeon Lee. Project administration: Sung-Wan Kim, Il-Seon Shin, Youngkeun Ahn, Jae-Min Kim. Resources: Jin-Young Park, Ju-Wan Kim, Hee-Ju Kang, Jae-Min Kim. Software: Jin-Young Park, Ju-Wan Kim, Jae-Min Kim. Supervision: Myung Ho Jeong, Jae-Min Kim. Validation: Wonsuk Choi, Ju-Yeon Lee. Visualization: Jin-Young Park, Ju-Wan Kim. Writing—original draft: Jin-Young Park, Ju-Wan Kim, Jae-Min Kim. Writing—review & editing: Jin-Young Park, Ju-Wan Kim, Jae-Min Kim.
Funding Statement
The study was funded by a grant of National Research Foundation of Korea Grant [NRF-2020M3E5D9080733] and [NRF-2020R1A2C2003472].