Embitterment in Vietnam War Veterans Predicted by Symptoms of Posttraumatic Stress Disorder
Article information
Abstract
Objective
Research on the association between posttraumatic embitterment disorder (PTED) and other psychopathologies in veterans and adults aged ≥65 years is lacking. This study aimed to assess embitterment among elderly war veterans and its association with major psychopathological factors.
Methods
Participants included Vietnam War veterans who visited a psychiatric clinic. Based on the Posttraumatic Embitterment Disorder Self-Rating Scale (PTEDS) score, the participants were divided into the embitterment (PTED(+), mean score of PTEDS items [mPTEDS] ≥1.6) and non-embitterment (PTED(-), mPTEDS <1.6) groups. Demographic characteristics, combat exposure severity, depression, anxiety, sleep, and alcohol use disorder symptom scores of the participants were collected and compared between the PTED(+) and PTED(-) groups. A correlation analysis between symptom measure scores and the mPTEDS was conducted. The influence of psychopathology on embitterment was investigated using stepwise multiple linear regression analysis.
Results
In total, 60 participants (28 in PTED(+) and 32 in PTED(-)) were included. Among those in PTED(+), 21 (35.0%) showed mild embitterment symptoms (1.6≤ mPTEDS <2.5) and 7 (11.7%) reported moderate or severe embitterment symptoms (mPTEDS ≥2.5). The mean scores of posttraumatic stress disorder (PTSD), depression, and anxiety were significantly higher in the PTED(+) than in the PTED(-) group. The mPTEDS were significantly correlated with PTSD, depression, anxiety, and sleep disorder scores. The PTSD symptoms significantly explained the higher mPTEDS score in a regression model.
Conclusion
Embitterment symptoms were associated with PTSD, depression, anxiety, and insomnia symptoms in elderly veterans, similar to the results of prior studies involving only the general population.
INTRODUCTION
Embitterment is a persistent feeling of being disappointed, insulted, feeling like a “loser,” or having a desire for revenge while also feeling powerless [1]. Linden [1] introduced the concept of posttraumatic embitterment disorder (PTED) to describe reactive symptoms following a significant event in an individual’s life, such as, unexpected job loss or uncertainty during German reunification. PTED is not included in the International Classification of Diseases, Tenth Revision (ICD-10) [2] or the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) [3]; however, it is presented as a subset of adjustment disorders that can be triggered by negative experiences in daily life. The core diagnostic criteria for PTED are presented in Table 1 [1].
A person is diagnosed with posttraumatic stress disorder (PTSD) or acute stress disorder, if they have witnessed or experienced a traumatic event that caused serious injury or was life-threatening that meet the diagnostic criteria [4]. Conversely, PTED can be diagnosed when a traumatic event does not meet the diagnostic criteria for PTSD or acute stress disorder but is preceded by an exceptional and negative event that occurs in daily life [1]. Linden and Maercker 5 suggested that PTED would best fit into the subtype of adjustment disorders. However, in the current DSM-5-TR and ICD-10 diagnostic criteria, adjustment disorders require a temporal link to a stressful event within 6 months before symptom onset, while PTED requires a temporal precedence of a stressful event but does not impose a time limit on the duration of the event to symptom onset. For adjustment disorders, the definition of a stressful negative event is vague. Adjustment disorder is also a diagnosis of exclusion, meaning it cannot be diagnosed if a depressive or anxiety disorder is diagnosed. In depressive or anxiety disorders, a stressful event often precedes the onset of an episode or symptom, but whether the stressful event precedes the episode does not affect the diagnosis. In depressive disorders, it is a matter of mood regulation, and the predominant emotional tone is depressed. In PTED, the predominant emotion is the anger at injustice, and mood dysregulation is not essential [5].
Although PTED is diagnostically distinguished from depressive disorders, anxiety disorders, and PTSD, it has also been associated with higher depressive, anxiety, and PTSD symptoms [1,6]. In the general population, people with PTED have a higher severity of perceived stress and depressive symptoms [7]. A recent study of war veterans found that those with PTSD had more symptoms of PTED [8]. In a study that examined comorbid mental disorders and psychometric characteristics of PTED, participants with PTED displayed significantly higher levels of depression, anxiety, somatization, PTSD, and obsessive-compulsive symptoms [9]. Insomnia has been proposed as an additional symptom of PTED [1], but no studies have explored the association between PTED symptoms and insomnia. Most research on the association between PTED and major psychopathology has been done in adult populations before old age [6-8,10-14]. The clinical presentation of psychiatric disorders in old age often differs from that in younger age [15-18]. Therefore, exploring the clinical presentation and association with other psychopathologies in the old age is important.
Korean veterans of the Vietnam War have experienced psychological trauma due to their participation in the war and have experienced a series of negative events (e.g., health-related issues due to aging and defoliant damage [19], unsatisfactory rewards for war participation [20]), including major disasters in Korea’s modern history (e.g., experiencing Korean war [1950–1953] [21] during their childhood; several economic crises and unemployment, such as the Oil crises [1973–1974, 1979–1981] [22] and the Asian economic crisis [1997–1998] [23]; and the recent coronavirus disease pandemic [24]). Therefore, high levels of embitterment symptoms are predicted among this population. Other than the study by Sabic [8], there is a lack of research on the association between PTED and other psychopathologies in veterans. Most Korean veterans of the Vietnam War are in their 70s. Research on the association of PTED with other psychopathologies in older adults is also lacking. Thus, it is necessary to study the association between embitterment and psychopathology in Korean veterans of the Vietnam War population.
The aim of this study was to examine the association between PTED symptoms and major psychopathologies in Korean veterans of the Vietnam War. The primary hypothesis was that people with significant levels of PTED symptoms would complain of more severe depression, anxiety, PTSD, and insomnia symptoms than would those with no or less PTED symptoms. To test our hypotheses, we compared the levels of depression, anxiety, PTSD, and insomnia symptoms between individuals who reported significant PTED symptoms and those who did not. We also examined the association between PTED symptoms and the symptoms of major psychopathologies.
METHODS
Ethics statements
Written informed consent was obtained from all the participants before participating in the study, and all study procedures were reviewed and approved by the Veterans Health Service (VHS) Medical Center Institutional Review Board (IRB) (IRB number: BOHUN 2021-08-020-002).
Study design and population
Patients who served in the Vietnam War and visited a psychiatric clinic at the VHS Medical Center in Seoul, Republic of Korea, were recruited. Participation in the Vietnam War was confirmed via registration for veterans compensation at the Ministry of Patriots and Veterans Affairs, Republic of Korea. Patients with cognitive decline to the extent that they had difficulty understanding or completing informed consent and questionnaires or conducting interviews were excluded. Participants provided demographic information on sex, age, education level, perceived economic status, and marital status during an outpatient visit to a psychiatric clinic at the VHS medical center. All participants completed the following self-report measures: Posttraumatic Embitterment Disorder Self-Rating Scale (PTEDS), Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), Combat Exposure Scale (CES), Posttraumatic Stress Disorder Check List-5 (PCL-5), Alcohol Use Disorder Identification Test (AUDIT), and Pittsburgh Sleep Quality Index (PSQI).
Assessment tools
PTEDS
Linden et al. [25] developed the PTEDS to measure PTED symptoms. This 19-item questionnaire was designed to assess PTED symptoms. Each question is answered on a Likert scale ranging from 0 to 4. In a standardization study of the scale, a mean score of ≥1.6 for each item was reported as clinically significant embitterment, and a score of ≥2.5 was reported as moderate to severe embitterment [25]. The PTEDS was translated into Korean and standardized. The internal consistency of the Korean version of the PTEDS, represented by the Cronbach α, was 0.962 [26]. We considered PTED to be present in individuals displaying a mean score of ≥1.6 on the PTEDS (PTED(+)). Participants who did not display PTED comprised the control group (PTED(-)).
PCL-5
The PCL-5 is a 20-item self-report questionnaire developed to measure the DSM-5 symptoms of PTSD. It is used in the screening and diagnostic assessment of PTSD and is appropriate for monitoring changes in PTSD symptoms. Participants rated how distressed they had been in the past month because of symptoms caused by past traumatic psychological experiences on a Likert scale from 0 to 4, with a total score ranging from 0 to 80 [27]. The Korean version of the PCL-5 was translated and standardized from the original English version by Kim et al. [28] It demonstrated good internal consistency (α=0.972) and test-retest reliability (r=0.96) in a validation study on elderly Korean Veterans of the Vietnam War [28].
CES
The CES is a 7-item self-reported questionnaire that assesses combat exposure. Each item measures exposure to a different combat-related situation (e.g., have you seen someone get shot or been in a dangerous situation, such as a prisoner of war), and each item is rated on a scale from 1 to 5, weighted by the severity of the experience, resulting in a total score of 0–41. A score of 0–8 points was categorized as mild, 9–16 points as mild-moderate, 17–24 points as moderate, 25–32 points as moderate-to-severe, and 33–41 points as severe [29]. We used the Korean version of the CES standardized by Kim et al. [30] The internal consistency of the Korean version of CES represented by Cronbach α was 0.85, and the test-retest reliability was 0.94 [30].
BDI
The BDI is a self-reported scale developed to assess depressive symptoms and their severity, and the BDI-II was later developed to align with the diagnostic criteria of the DSM-IV [31]. The Korean version of the BDI-II has been translated and validated, in which internal consistency using Cronbach α was 0.834 in the depressive patient group and 0.880 in the normal control group. The total score ranges from 0 to 63 when the 21 items are summed on a 0–3 scale [32].
BAI
The BAI is a widely used self-reported measure for assessing anxiety. The questionnaire consists of 21 items that reflect how participants felt over the past week. Each item is scored from 0 to 3, with the total score ranging from 0 to 63. Higher scores indicate higher anxiety symptoms [33]. We used a revised version of the BAI as standardized by Lee et al. [34], in which the internal consistency of the Korean version of BAI represented in Cronbach’s α was 0.91 and the test-retest correlation was 0.84.
AUDIT
The AUDIT was developed and standardized by the World Health Organization as a standardized test to screen for alcohol use disorders and problematic alcohol use [35,36]. In a standardization study of the Korean version of the AUDIT, the threshold score to screen for problematic alcohol use was estimated to be 12, with sensitivity and specificity of 0.84 and 0.86, respectively [37,38]. Indicating the internal consistency of the Korean version of the AUDIT, Cronbach’s α coefficient was 0.92 [38].
PSQI
The PSQI is a subjective assessment of sleep quality, including the duration, depth, and satisfaction with sleep for a month, and has been widely used in various clinical settings and studies [39,40]. Cronbach’s α coefficient for internal consistency of the total score of the Korean version of the PSQI was 0.84 in the validation study, showing high reliability [41].
Statistical analysis
For each sociodemographic and symptom scale examined, we first calculated the means and standard deviations for continuous data and proportions for nominal data. The proportion of individuals reporting clinically significant PTED symptoms (mean score of PTEDS items ≥1.6) and moderate or greater PTED symptoms (mean score of PTEDS items ≥2.5) in the overall sample was determined. Demographics and scores on depression, anxiety, PTSD, sleep, and alcohol use disorder symptom scales were compared between the PTED(+) and PTED(-) groups based on PTEDS scores using the chi-square test, Fisher’s exact test, independent t-test, and Mann–Whitney U test. Pearson’s correlation analyses between each of the depression, sleep disorder, and combat exposure scales and PTEDS scores were performed to explore correlations; multiple linear regression analyses of PTEDS scores were performed to explore the effects of possible confounding variables and psychiatric symptom scales. All analyses were performed using the Statistical Package for the Social Sciences, version 18.0 for Windows (SPPS Inc., Chicago, IL, USA) and R version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org).
RESULTS
Participants
From November 1, 2021, to January 3, 2022, 63 patients who visited the psychiatric clinic at the VHS Medical Center were recruited. Of the 63 consenting participants, 3 refused to complete the self-report questionnaires, leaving 60 participants who completed the interview and self-report questionnaires.
Of the 60 participants, 28 reported significant embitterment symptoms (mean item score of ≥1.6 on the PTEDS), among whom, 21 (35.0%) reported mild embitterment symptoms (mean item score of ≥1.6 but <2.5 on the PTEDS) and 7 (11.7%) reported moderate embitterment symptoms (mean item score of ≥2.5 on the PTEDS) (Table 2).
The demographic characteristics of the PTED(+) and PTED(-) groups are presented in Table 2. There were no significant differences in age, education, employment, marital status, perceived economic status, or combat exposure, as measured by the CES, between the groups.
Comparison of psychopathology between the groups
The PTED(+) group showed significantly higher mean scores for the PTSD, depression, anxiety, and insomnia symptom measures than did the PTED(-) group (Figure 1 and Supplementary Table 1 in the online-only Data Supplement). There was no significant difference in the total score of AUDIT (Supplementary Table 1 in the online-only Data Supplement) and the proportion of participants with problematic alcohol use (AUDIT score≥12 is considered as problematic alcohol use; PTED(-): 3(9.30%); PTED(+): 7(25.00%); p=0.165) between the PTED(+) and PTED(-) groups.

The comparison of psychological measure mean score between PTED(+) and PTED(-); PTSD, depression, and sleep disturbance symptom scales. PTED, posttraumatic embitterment disorder; PCL-5, Posttraumatic Stress Disorder Check List-5; BDI, Beck Depression Inventory; PSQI, Pittsburgh Sleep Quality Index; PTSD, posttraumatic stress disorder.
Correlation between PTED symptoms and major psychopathologies
The Pearson’s correlation analysis showed that the PTEDS scores were significantly correlated with the PCL-5, BDI, and PSQI scores. The PTEDS scores were not significantly correlated with the CES scores. Meanwhile, PCL-5 scores were correlated with PTED, BDI, PSQI, and CES (Table 3). Among the variables, BAI and AUDIT were excluded from the Pearson’s correlation analysis because they did not follow a normal distribution (Supplementary Table 1 in the online-only Data Supplement).
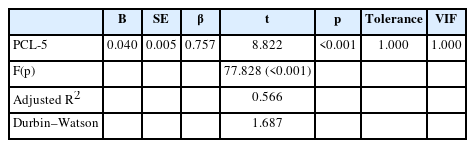
Multiple linear regression model
To explore the contribution of variables that may influence embitterment symptoms, stepwise multiple linear regression analysis of PTEDS scores as dependent variables was performed, with BDI, PCL-5, PSQI, and CES scores used as covariates to consider the effects of depression, PTSD, insomnia, and combat exposure. Multiple regression analyses showed that PCL-5 scores explained statistically significant variations in the PTEDS scores (Table 4). The regression coefficient and variance inflation factor of included and excluded variables in the stepwise linear multiple regression model indicated no significant inter-correlation between covariates arising multicollinearity (Table 4 and Supplementary Table 2 in the online-only Data Supplement).
DISCUSSION
The main finding in this study is that embitterment symptoms were associated with PTSD, depression, anxiety, and insomnia symptoms in elderly veterans. In particular, high PTSD symptom scores significantly explained elevated PTED symptom scores, indicating a strong association between the two symptom groups. Depression, anxiety, PTSD, and insomnia are common in veterans [42,43]. The severity of these symptoms increases with high levels of PTED symptoms, suggesting that embitterment symptoms should be closely monitored in psychiatric evaluations of veterans.
In a previous study using an e-mail survey of the Korean general population, 42.7% reported mild to moderate embitterment (PTEDS items with a mean score of ≥1.6), and 13.3% reported moderate to severe embitterment (PTEDS items with a mean score of ≥2.5) [7]. Among the recruited older veterans, the proportion of those who displayed significant PTED symptoms was comparable with that in the general population. In the study on the general population in South Korea, the use of an internet-based survey with email replies limited participants to the internet-using population and skewed the sample toward more highly educated users; the response rate was lower than that in a typical paper survey at 11%, which may not have been representative of the general population and may have exaggerated the proportion of those with significant PTED symptoms [7]. The proportion of participants with moderate to severe PTED symptoms in the current study was higher than that (2.5%) of the general German population with moderate-to-severe PTED in 2009 [25]. In a study on active duty members in South Korea, whose mean ages were 21.32±1.57 years, 11.5% of the soldiers displayed mild PTED symptoms, and 4% of them had moderate to severe PTED symptoms; this indicated that the proportion of individuals with more severe embitterment symptoms was lower among active duty members than among older veterans with PTED. Considering the result from previous studies evaluating PTED prevalence in non-elderly populations, our participants, who were elderly Korean Vietnam War veterans, had a relatively high level of PTED symptoms.
Lee and Kim [11] examined the relationship between negative life events and PTED symptoms in young adults and found that the cumulative and differential effects of negative events increased the risk of embitterment. Our participants were older war veterans who experienced psychological trauma due to their service in the war and a series of negative events, including health related issue due to defoliant damage [19] and unsatisfactory reimbursement of war particaipation [20,44]; this factor may have affected high PTED prevalence.
Depressive symptoms were significantly increased in patients with significant PTED symptoms. In a general population study in South Korea, embitterment symptoms were positively correlated with depressive symptoms [7]. In active duty military personnel in South Korea, depressive symptoms were positively correlated with the severity of embitterment symptoms, and in regression analysis, increase in depressive symptoms explained increase in the PTEDS scores [14]. In Linden et al.’s study [9], the comorbidity prevalence rate of major depressive disorder and dysthymia in patients with PTED was not significantly different from that of major depressive disorder and dysthymia in patients without PTED. However, in the same study, patients with PTED exhibited significantly higher levels of depressive symptoms than did those without [9]. Linden and Maercker [5] stated that, unlike depression, PTED does not involve impaired emotional regulation, and a person with PTED can be in a normal mood even if they are vengeful. These findings from current and previous studies support the idea that PTED appears to be strongly associated with depressive symptoms, although it is distinct from depressive disorders.
In the present study, anxiety levels, as measured by the BAI, were higher in the PTED(+) group than in the PTED(-) group. This supports the finding that older men with PTED have higher levels of anxiety symptoms, similar to previous findings in a population that was not elderly. In a previous study, based on the Symptom Check List-90-Revised scores, there were increased levels of anxiety and phobic anxiety and higher rates of panic disorder, as confirmed by the Mini International Neuropsychiatric Interview, in younger people with PTED than in those without PTED [9].
The PTED(+) group had higher PCL-5 scores than did the PTED(-) group despite no significant differences in combat exposure or other sociodemographic characteristics. Furthermore, in multiple regression analysis, increased PTSD symptoms explained higher PTED symptom levels. In Sabic et al.’s study [8] comparing PTED symptoms in veterans with PTSD (mean age: 52.78±5.99 years) and those without PTSD (mean age: 51.42±5.98 years), those with PTSD had more PTED symptoms. Linden et al. [9] found that intrusion, hyperarousal, and avoidance symptoms, as measured using the Impact of Event Scale, were increased in patients with PTED. The diagnostic criteria for both PTSD and PTED include a series of negative emotions and thoughts that occur after a negative event. However, PTSD is caused by terrifying, life-threatening experiences that cause intense anxiety, dominated by memories and intrusions, whereas PTED is triggered by events that challenge a person’s psychological integrity, such as experiences of injustice, humiliation, or breach of trust [1]. In PTSD, anxiety is the dominant emotion, whereas in PTED, embitterment and a desire for revenge are predominant [5]. Considering that combat exposure level, which can be considered psychological trauma shared by the study population, was not significantly different between PTED(-) and PTED(+) groups, more severe PTSD symptoms in the PTED(+) group could be attributed to other life events that happened during participant’s lifetime which may or may not fulfill the requirement of psychological trauma to cause PTSD.
Among the additional signs and symptoms of PTED suggested by Linden et al. [25] that include sleep disturbance as one of the various unspecific somatic complaints, there are sparse data on sleep disturbance in PTED. To the best of our knowledge, this is the first study to examine sleep disturbance in patients with PTED using a self-questionnaire. Participants with PTED had higher PSQI scores, indicating more complaints of sleep disturbance. Sleep disturbances in patients with PTED may arise from other comorbid mental conditions, e.g., depression, anxiety, PTSD, and PTED, as secondary insomnia. Moreover, primary insomnia may be increased in patients with PTED. Because of the retrospective nature of self-reported questionnaires and the lack of other sleep measures, there is a limit to deducing hypotheses on the relationship between sleep disturbance and PTED. Further studies are warranted to determine the association between sleep disturbances and embitterment.
The proportion of problematic alcohol use was not significantly different between the PTED(+) and PTED(-) groups. Contrary to the well-known relationship between alcohol use and other mental disorders such as depression [45-48], anxiety disorders [48-50], PTSD [51-53], there are sparse data on the relationship between problematic alcohol use and PTED in previous studies. In the study on PTED patients admitted to a psychiatric department at a German hospital, 6.8% were co-diagnosed with alcohol abuse via Mini International Neuropsychiatric Interview [6]. No comparable study sought the prevalence of alcohol abuse in non-PTED psychiatric inpatients. In a systematic review on the impact of alcohol problems in major depression, where most included studies were conducted in psychiatric inpatient settings, the prevalence of current alcohol problems in depression was 16% (range, 5–67) [54]. Furthermore, current alcohol problem prevalence among depression was 21%, while it was 7% in the general population [53]. Thus, PTED may have a relatively weaker effect on problematic alcohol use than do other mental disorders such as depression, anxiety disorders, and PTSD.
Most research on Vietnam War veterans has been conducted in the United States and has focused on the course of PTSD symptoms [55,56], factors contributing to PTSD symptom severity [56], and the physical and mental health and social impact of PTSD symptoms [57]. However, to date, no studies have measured embitterment in Vietnam War veterans and explored its association with other psychopathological factors. In a study on non-Vietnam War veterans, when embitterment symptoms were measured in Bosnian War veterans with and without PTSD, these symptoms were significantly higher in those with PTSD [8]. This is consistent with the present results, in which higher PTSD symptoms explained more PTED symptoms.
This study has several limitations. Self-reported questionnaires are subject to recall bias and underreporting due to the retrospective nature of symptom measures, and causal inferences may be limited because of the cross-sectional nature of the study. Symptom scales based on self-report measures of major psychiatric disorders were used to examine symptoms of depression, anxiety, PTSD, and insomnia, allowing us to infer the extent of participants’ symptoms, but a limitation is that clinician diagnoses were not investigated. Despite the fact that several studies on Korean population [11-14,26] consider a PTEDS score of 1.6 or higher as significant embitterment symptoms and 2.5 or higher as moderate to severe embitterment symptoms following the result from Linden et al.’s study [25], a cutoff score according to symptoms severity of PTEDS has not been defined in Korean population. This limits the reliability of the cutoff points. The anxiety and problematic alcohol use scale variables were not normally distributed and were not included in the correlation and multiple regression analyses, limiting our ability to assess the impact of anxiety and alcohol use on PTED symptoms. Additionally, the small sample size limited the power of the statistical analysis. All study participants were male and ≥70 years old, which confers limitations in generalizing the present findings to other populations (e.g., women or non-elderly individuals). Assessments of stress, negative life events, and psychological trauma were lacking; this limited evaluation of the effects of negative life events other than combat exposure on embitterment severity.
Nevertheless, this study is valuable because it is the first investigation on embitterment symptoms in older Asians, specifically Korean veterans who served in the Vietnam War. The study population experienced psychological trauma by engaging in combat situations and also a series of negative events, which is subthreshold to be acknowledged as psychological trauma (e.g., health related issue due to Agent Orange damage [19] and inadequate compensation for participation in the war [20,44]). The current study also has its strength in that it examined the association of PTED symptom level with psychopathology, such as depression, anxiety, PTSD, and sleep disturbance in the elderly population with the same type of psychological trauma.
Significant PTED symptoms were associated with increased depression, anxiety, sleep disturbance, and PTSD symptoms among older men in a clinical psychiatric population who had experienced various stressors and psychological trauma: war participation. More severe PTSD symptoms explained the higher PTED symptom levels. In a population that has experienced psychological trauma that may cause PTSD, significant embitterment can be predicted when PTSD symptoms are severe.
Most studies on embitterment or PTED are cross-sectional. Future prospective studies are needed to investigate the natural course of PTED in various populations, including the general population, and the efficacy of treatments that are thought to be effective in PTED, e.g., wisdom therapy, as proposed in a previous study [58].
Supplementary materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2023.0299.
The result of normality test and mean comparison of continuous variables
Regression coefficient and variance inflation factor of variable excluded variables in step-wise linear multiple regression model
Notes
Availability of Data and Material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
Changsu Han, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Seung-Hoon Lee. Data curation: Seung-Hoon Lee. Formal analysis: Seung-Hoon Lee, Changsu Han, Junhyung Kim. Funding acquisition: Seung-Hoon Lee. Investigation: Seung-Hoon Lee, Jin Hee Choi, Hayun Choi. Methodology: Seung-Hoon Lee, Changsu Han, Junhyung Kim. Project administration: Seung-Hoon Lee. Resources: Seung-Hoon Lee. Software: Seung-Hoon Lee. Supervision: Hyun-Ghang Jeong, Moon-Soo Lee, Jin Hee Choi, Hayun Choi. Validation: Seung-Hoon Lee, Changsu Han, Junhyung Kim. Visualization: Seung-Hoon Lee. Writing—original draft: Seung-Hoon Lee. Writing—review & editing: Changsu Han, Junhyung Kim, Hyun-Ghang Jeong, Moon-Soo Lee, Jin Hee Choi, Hayun Choi.
Funding Statement
This study was supported by a VHS Medical Center Research Grant, Republic of Korea (VHSMC21012).