Does Psychodrama Affect Perceived Stress, Anxiety-Depression Scores and Saliva Cortisol in Patients with Depression?
Article information
Abstract
Objective
Little is known about the effects of psychodrama group therapy on the level of stress, anxiety and depression of the group members, and the biological markers of stress. The aim of this study test cortisol level as a biological reflection of some mental characteristics gained by the psychodrama method in coping with stress.
Methods
Depressive patients aged between 18 and 65 years, who diagnosed with depression according to DSM-5, without psychiatric comorbidity, who do not use drugs and were available for psychodrama were enrolled into the study. These patients were evaluated using the Perceived Stress Scale, State-Trait Anxiety Inventory and Beck Depression Inventory. In order to observe the circadian rhythm of cortisol, samples were collected from the participants before lunch, before dinner and before going to sleep on the day before psychodrama and on the 0, 15th, and 30th minutes after awakening in the morning of the psychodrama day; as well as just before and after the psychodrama session. Saliva cortisol level just before the initial session of psychodrama group therapy was compared with the saliva cortisol level just after the last psychodrama session at the end of 16 weeks.
Results
Statistically significant difference was determined between the scores of perceived stress scale, STAI-1, STAI-2, beck depression inventory and salivary cortisol level before and after psychodrama session. There was significant decrease in both the scale scores and salivary cortisol after vs. before psychodrama.
Conclusion
This results is important as it shows the biological aspect of clinical improvement. Further studies would provide us with better understanding of the effects of psychodrama group psychotherapy on depressive mood and biological projections by means of short-term and long-term follow-up studies.
INTRODUCTION
Major depression, in which biological susceptibility plays an important role, is a mood disorder usually triggered by unfavorable life events [1]. Conducting studies on the role of biological factors in the etiology of major depression has been possible with technological advancements. Abnormalities of the hypothalamic-pituitary-adrenal (HPA) axis are among the predictors demonstrated most commonly and consistently [2]. High cortisol level is determined in about 50% of depressive patients [3]. Cortisol level increases in the hypothalamic-pituitary-adrenal (HPA) axis as a response to stress and plays a critical role in hemostasis. It is known that stress has a significant role in the initiation and maintenance of depression. It is also known that there are severe stressor agents prior to the depression attacks [4] and that unpleasant experiences in early childhood enhance the risk of developing depression in the adulthood [5].
Psychotherapeutic interventions are the methods known to have favorable impacts on the patients’ coping with stress and on the quality of life and are recommended to be used particularly in depression [6,7]. Group psychotherapy is a psychotherapeutic method performed with 8–10 participants where the group rules such as respect, privacy and constructive feed-back, which in general help with establishing an environment of trust, are implemented. Proving the efficacy of group psychotherapies has always been the subject of interest for researchers. Early investigations have not confirmed the use of group therapies as an independent therapeutic method although they are auxiliary therapies [8]. In the recent years, however, it has begun to be defined that group therapies have the ability of making objectively measurable changes in the patient’s attitude, personality and behavior [9].
Psychodrama is an experiential method of group therapy, which uses the role play technique in a managed way to make the participants to be aware of personal and interpersonal problems and work on the probable solutions via acting method, to see themselves from the outside, to try new roles, to gain different points of view and to change. It allows the group members to see the results of different behaviors and problem solution methods via intra group activities. These methods include expression of emotions and thoughts, prediction of personal and social skills, adaptation of new behaviors, and rehearsal for potential problems [10]. Evidences indicating the efficacy of psychodrama group therapy are quite limited. In one of these limited studies, it was reported that drama-based interventions have significant impacts on self-conception and social functioning in the adolescents [11,12].
Nevertheless, little is known about the effects of psychodrama group therapy on the level of perceived stress, anxiety and depression scores of the group members, and the biological markers of stress. This pilot study tested the hypothesis that cortisol level decreases as a biological reflection of some mental characteristics gained by the psychodrama method in coping with stress.
METHODS
Depressive patients aged between 18 and 65 years, who visited a psychiatry clinic of a university hospital, evaluated by a psychiatrist and diagnosed with depression according to DSM-5 [using The Structured Clinical Interview for DSM-5 (SCID-5)], without psychiatric comorbidity, who do not use drugs and were available for psychodrama and willing to join the group were enrolled into the study. Patients had no drug use and no psychiatric comorbidity. Whereas the psychodrama group consisted of 10 patients initially, the study was carried out with 8 patients since 2 patients thereafter left the group. Additional physical disorders, neurological and endocrine disorders, receiving drugs that may interfere with cortisol levels, and presence of additional psychiatric diagnoses that might be confounding factors in both group dynamics and cortisol levels were predetermined as exclusion criteria. Prior to the study, all patients were informed about the procedure and their written consents were obtained (inönü university ethics committee, approval number:2013-204). They underwent minimal physical, neurological and psychiatric examination and laboratory testing.
Patients that agreed to participate in the study completed the following scales both prior to the psychotherapy process and after the group therapy sessions that lasted for 16 weeks.
Perceived Stress Scale (PSS) was developed by Cohen et al. [13] PSS, which consisted of a total of 14 items, was designed to measure to what degree a set of situations are perceived as stressful. Participants rate each item over 5-point Likert scale ranging from “Never (0)” and “Very often (4).” Among these items, positive statements are rated reversely. The scores of PSS-changes between 0 and 40. High scores indicate higher level of perceived stress. Validity and reliability of the Turkish version was performed by Eskin et al. [14]
State-Trait Anxiety Inventory (STAI-I and STAI-II) was developed in 1983 by Spielberger et al. [15] It was adapted into Turkish by Öner and Le Compte [16] and validity and reliability study was done. Each of the subscales consists of 20 items. Answers are scored between 1 and 4. Total score obtained from each subscale ranges from 20 to 80. High score indicates high anxiety level.
Beck Depression Inventory (BDI), which was developed by Beck and Steer [17] and consists of 21 items, was used to measure depressive symptoms. Each item indicates a depressive symptom. BDI, which is a self-report tool, is the most common tool used to measure depression worldwide. Total score changes between 0 and 63 with higher scores indicating severer depression. In the validity and reliability study, coefficient of internal consistency reliability was calculated to be 0.84 [18].
Practice of psychodrama group psychotherapy
Group practices were performed once in a week between 14:00 and 17:00 o’clock for 16 weeks in a place suitable for psychodrama group practice. Each session was managed by a therapist and a co-therapist under the supervision of a supervisor.
Analysis of salivary cortisol for cortisol levels
Cortisol level, which is one of the biological markers of stress, is determined by means of the salivary cortisol level. Saliva samples were collected according to the expert consensus guidelines reported by Stalder et al. [19] and following the rules explained by Ozgocer et al. [20] Experimental procedure and study protocol were briefly explained to the participants during face-to-face interview. Polypropylene tubes (1.5 mL, ISOLAB Laborgeräte GmbH, Wertheim, Germany) labeled with the participant’s ID and sample number (e.g. S1, S2, S3, S0, S15, S30, S4, and S5) were given to the participants. Passive drool method was used to collect saliva samples. Participants were warned to avoid any kind of activities such as eating, drinking, and brushing teeth in the first 30 min after waking up and before the collection of other samples. Drinking water was allowed, provided that it has been stopped at least 10 min before the next saliva sampling. Cortisol secretion shows a circadian rhythm; it peaks in the morning and then gradually declines during day time. An other aspect of cortisol secretion is called as cortisol awakening response (CAR). This acuterise, which is superposed on the normal cycle, reaches peak level about 30 min after awakening [21]. Attention was paid for the samples to be collected from all participants at the same hour, during fasting and after resting. In order to observe the circadian rhythm of cortisol, samples were collected from the participants before lunch, before dinner and before going to sleep on the day before psychodrama and on the 0, 15th, and 30th minutes after awakening in the morning of the psychodrama day; as well as just before and after the psychodrama session. Study design is illustrated in Figure 1.
However, as the number of saliva samples collected from the participants is not high enough to perform the statistical analyses, after session vs. before session comparison could not be performed. Saliva cortisol level just before the initial session of psychodrama group therapy was compared with the saliva cortisol level just after the last psychodrama session at the end of 16 weeks.
Saliva cortisol analysis
Salivary samples were analyzed for cortisol level by enzyme-linked immunosorbent assay (ELISA) developed in our laboratory [22]. In brief, cortisol-BSA stock solution was diluted with carbonate buffer and used at an amount of 200 μL/well in a 96-well microtiter plate. The plate was incubated overnight at +4 C and then washed with wash buffer. After blocking the unbound sites, standard solutions or samples were added in triplicate (40 μL/well). Addition of specific primary antibody (40 μL/well) was followed by addition of biotinylated secondary anti-rabbit antibody (100 μL/well). Incubations were carried out at 37°C for 45 min and at 37°C for 30 min, respectively for the last two stages. At the end of each stage, the plate was washed and finally streptavidin peroxidase solution (100 μL/well) was added and the plate was incubated at 37°C for 15 min. The plate was washed again and tetramethylbenzidine substrate (150 μL/well) was added, and then it was incubated in the dark medium for 10 min. After the addition of stop solution (sulfuric acid 10%, 50 μL/well), the absorbance was measured at 450 nm using a plate reader spectrophotometer (BioTek, Synergy HT, Winooski, VT, USA). Cortisol concentrations were quantified using the program in the spectrophotometer [22].
Statistical analysis
Statistical analyses were performed by the Statistical Program for Social Sciences-SPSS for Windows, version 17.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were presented as mean and standard deviation for numerical variables and as number and percentage for categorical variables. Nonparametric test was used to compare the numerical variables in casecondition for normal distribution was not met. A p value <0.05 was considered statistically significant.
RESULTS
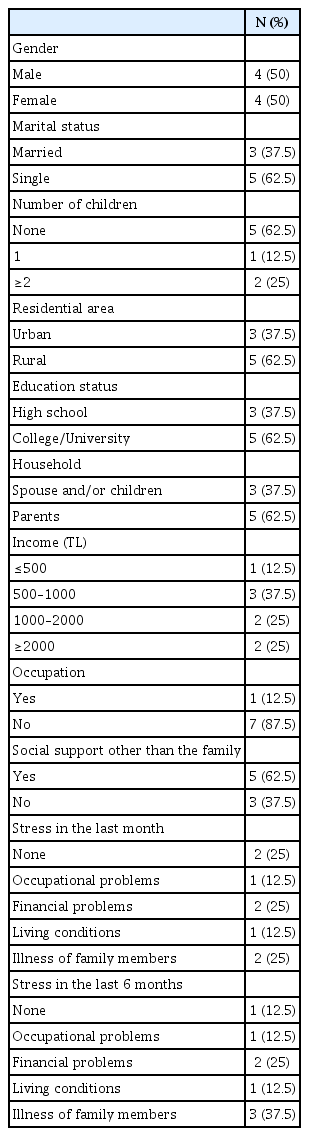
The psychodrama group consisted of 8 subjects, of which 4 were male and 4 were female. The mean age was 34.37±11.75 years. None of the participants had physical comorbidity. All of them were being followed for depression, and the mean follow-up period was 5.37±7.02 years. None of the participants were consuming alcohol or smoking. Other sociodemographic characteristics of the group are demonstrated in Table 1.
The mean diurnal salivary cortisol level of depressive patients participating in the 16-week psychodrama sessions are illustrated in Figure 2.
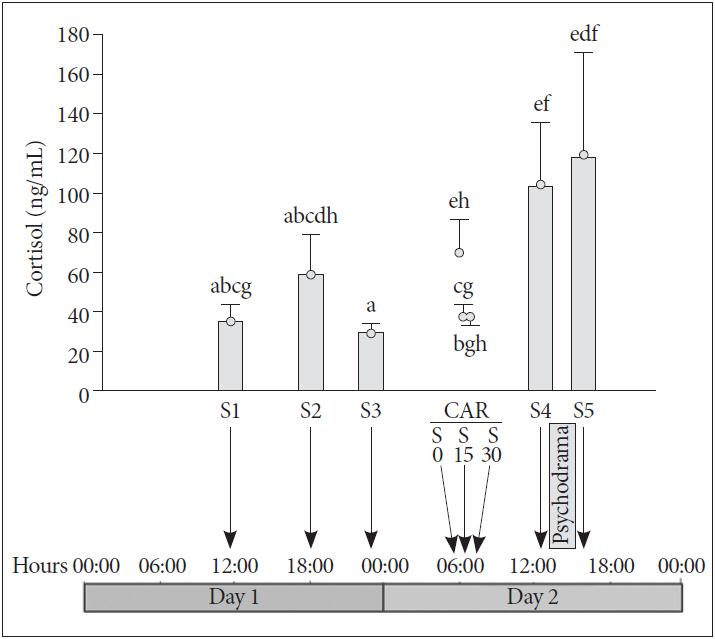
Mean diurnal salivary cortisol levels in depressive patients participated in the weekly psychodrama sessions for 16 weeks. Saliva samples were collected in two consecutive days every 4 weeks until the end of the study. Cortisol values represent the mean of entire study period. The S1-S3 denotes saliva sampling for the assessment of diurnal cortisol release; S4-S5 denotes saliva sampling before and after the psychotherapy session in the next day; S0, S15 and S30 denotes saliva sampling for cortisol awakening response (CAR) just after awakening (S0) and 15 (S15) and 30 (S30) min after awakening. Columns (or points) with different letters differ significantly by paired t-test. In summary, cortisol levels were the lowest in the midnight sample (S3) but the highest just before and after the group psychotherapy session. a: before lunch, one day before psychodrama, b: before diner, one day before psychodrama, c: before sleeping, one day before psychodrama, d: 0 minutes after waking in the morning, e: 15 minutes after waking in the morning, f: 30 minutes after waking in the morning, g: before psychodrama, h: after psychodrama.
Correlation between diurnal salivary cortisol levels is illustrated in Figure 3.
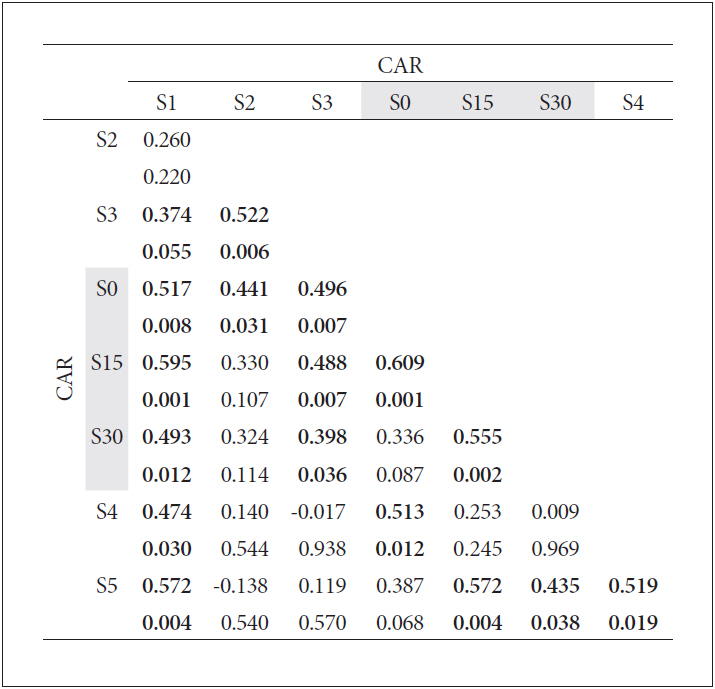
Pearson correlations among the log10-converted salivary cortisol data. In each cell, the upper value is the correlation coefficient (r) and the lower value is the p value. Significant correlations are shown in bold. In general, all data seem to be inter-correlated, but S1 cortisol levels (sample taken after the lunch on Day 1) best describe the data taken afterwards (except S2). Additionally, S3 level (sample at midnight) is positively and significantly correlated with all cortisol awakening response (CAR) data. Data before and after psychodrama session (S4 and S5, respectively) are also positively correlated.
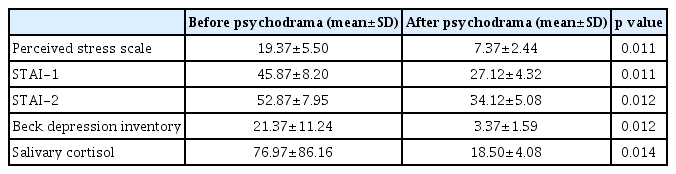
Statistically significant difference was determined between the scores of perceived stress scale, STAI-1, STAI-2, beck depression inventory and salivary cortisol level before and after psychodrama session. There was significant decrease in both the scale scores and salivary cortisol after vs. before psychodrama (Table 2).
DISCUSSION
The primary objective of the present study was to investigate the effect of psychodrama group therapy on the level of perceived stress, level of state-trait anxiety, Beck depression scores and accordingly salivary cortisol levels in depressive patients.
It is known that both biological and psychological factors play a role in the development of depression. The relationship between cortisol over secretion and depression is one of the oldest investigations in the field of biological psychiatry. Primarily the activation of HPA axis and increased glucocorticoid activity attract attention when the organism faces with stress. It is known that diurnal rhythm of cortisol is impaired in the subjects suffering from depression, or changes in cortisol level may lead to depressive symptoms [23]. Even though plasma cortisol levels are frequently measured in depressive patients, it is observed that the cortisol peaks in these patients do not increase in number compared to normals. For this reason, depressed cortisol hypersecretion is not due to the peak value of plasma cortisol, but is due to excess secretion on each peak [24]. Symptoms that accompany depression such as sleep disorders, decreased libido, cardiovascular changes and cognitive dysfunction indicate that HPA axis as well is involved in the development of depression. Plasma cortisol concentration is increased, metabolites of cortisol are increased, and 24-hour urinary free cortisol concentration is increased in the majority of patients with major depression [25]. Increased cortisol production during depression returns to the normal levels with resolution of depression; i.e., it appears to be a state marker [26]. Moreover, also the normal circadian rhythm of cortisol is impaired in depressive patients in addition to the increased basal cortisol levels. HPA axis changes are more prominent in the patients with severer depression and in older patients [27]. There is a very limited number of studies examining the effect of psychotherapies on cortisol levels. One of these studies examined the effect of SSRI and psychotherapy on cortisol levels in generalized anxiety disorder. Older adults with GAD who received both escitalopram and CBT demonstrated a significant reduction in peak cortisol levels at posttreatment compared to the group who received escitalopram without CBT augmentation [28]. Psychodrama group psychotherapy is a method used for the treatment of depression. It was determined that depressive symptoms are improved and symptom severity is decreased after treatment with psychodrama [29]. Huntley et al. [30] conducted a systematic review and meta-analysis to investigate the efficacy of group-based psychological therapy in depression and concluded that psychotherapies except for CBT have limited efficacy. Despite the outcomes that psychodrama group psychotherapy contributes to the decrease in depressive symptoms and increase in the subjects’ social adaptation [31], studies on this field are limited in number. Moreover, biological projection of clinical improvement as well has not been studied enough. It is reported that psychotherapies, which have different theories and methods of implementation known to be effective in the treatment of depression, have improving effect as in drug therapy on the abnormalities that occur with depression in the metabolism and activity of prefrontal cortex [32]. The present study aimed to test the hypothesis that psychodrama group therapy is clinically effective and that the changes in a biological marker like salivary cortisol accompany the improvement.
The results of the present study reveal statistically significant decrease in the level of perceived stress, state-trait anxiety scores and severity of depression with psychodrama group psychotherapy. Decrease in the same direction was determined also in the salivary cortisol level. This is important as it shows the biological aspect of clinical improvement.
The limitations of the present study include limited patient number, evaluation of only the patients with mild-moderate depression, and measurement of neurochemical abnormalities in depression only by means of salivary cortisol level.
Further studies would provide us with better understanding of the effects of psychodrama group psychotherapy on depressive mood and biological projections by means of short-term and long-term follow-up studies.