The Relationship Between the Oxytocin Level and Rejection Sensitivity, Childhood Traumas, and Attachment Styles in Borderline Personality Disorder
Article information
Abstract
Objective
In this study, it is aimed to investigate the relationship between the oxytocin level and the rejection sensitivity, childhood mental traumas, and attachment styles in patients diagnosed with borderline personality disorder (BPD).
Methods
Participants between the ages of 18–30 were included in the study. The patient group consists of 31 participants and the healthy control group consists of 31 participants. Sociodemographic/Clinical Variables Questionnaire, Relationship Scales Questionnaire, Rejection Sensitivity Questionnaire and Childhood Trauma Questionnaire were administered to the participants included in the study. Serum oxytocin levels of the participants were measured using the Elisa method.
Results
The oxytocin levels were found to be significantly lower in patients with BPD than in healthy control subjects, whereas the rejection sensitivity and childhood traumas were found to be significantly higher. No difference was found between the patient and control groups in terms of attachment styles, yet it was determined that there may be differences between the oxytocin levels of the BPD patients according to the attachment styles the patients have.
Conclusion
In conclusion, the findings of this study revealed that the rejection sensitivity in BPD patients is not associated with oxytocin levels and childhood traumas, indicating the need to assess the BPD patients in terms of other biopsychosocial factors related to the etiopathogenesis of BPD.
INTRODUCTION
Borderline personality disorder (BPD) is a syndrome with an onset in young adulthood, characterized by excessive impulsivity, imbalance in affect and interpersonal relationships, inadequate self-perception, and hypersensitivity to abandonment [1]. It has been reported in the literature that the behaviors characterized by unstable self-esteem, negative affect, and sensitivity to feelings of rejection, which are considered as the building blocks of BPD, cause deterioration in interpersonal relationships that significantly affect functionality as an inevitable consequence [2,3]. It is known that patients with BPD can change their attitudes and feelings towards others rapidly and drastically [4], and that minor emotional symptoms of others may cause great sensitivity in individuals with BPD. It has also been reported that the patients with BPD do not want to be alone due to the fear of abandonment, that the temper tantrums experienced in a possible abandonment situation may pose a significant problem in interpersonal relationships, and that patients with BPD may harm themselves or others in such situations [1,5]. The problems experienced in interpersonal relationships in the context of BPD have been clearly described; however, the underlying mechanisms are still not fully clarified [6].
Rejection sensitivity is characterized with behaviors such as anxiously expecting rejection, readily perceiving rejection, and overreacting to rejection. Once this dynamic is formed in a person, it seems to persist throughout one’s life [7]. It has been reported that rejection sensitivity may in fact be an adaptive response that is exhibited to keep the individual safe from the childhood experiences related to rejection, such as having been neglected and/or abused. In addition, it was determined that emotional neglect and/or abuse experienced in childhood in particular were associated with the rejection sensitivity, and that rejection sensitivity formed as a result of such negative experiences may be a factor in the development of BPD later [6].
A number of studies conducted on humans and animals have demonstrated that oxytocin plays a role in attachment and social behavior. It was reported that the administration of oxytocin have increased looking others in the eye and enhanced the ability to recognize the faces of others and to understand their emotions. It was also found that oxytocin reduces anxiety by suppressing the release of cortisol triggered by stress and creates a sense of trust [8]. In a study conducted on female patients with BPD, plasma oxytocin levels were found to be statistically significantly lower in the patient group than in the control group [9]. Additionally, in a functional magnetic resonance imaging study, it was observed that looking at angry faces heightened the activation of the amygdala in patients with BPD, and that oxytocin reduced the activation of the amygdala as well as the hypersensitivity to social threats [10].
A thorough review of the literature revealed a number of studies on attachment styles, early childhood traumas, and rejection sensitivity in relation to BPD; however, no studies were found on the relationship of attachment styles, early childhood traumas, and rejection sensitivity with oxytocin level, which is known to have an effect on social behaviors. Accordingly, in this study, in line with the relevant results reported in the literature, it was hypothesized that patients with BPD would have lower oxytocin levels along with higher rejection sensitivity, higher prevalence of childhood traumas, and more insecure attachment styles compared to the healthy control subjects. In parallel with this hypothesis, it has been aimed to determine the relationship between low oxytocin levels and the rejection sensitivity, childhood traumas, and attachment styles in patients with BPD.
METHODS
Population and sample
The population of this study consisted of female participants aged between 18 and 30. The patient group was selected from among the individuals who presented the Malatya Training and Research Hospital Psychiatry Outpatient Clinic between 01/08/2020 and 01/01/2021 with depressive, anxiety, obsession or compulsion symptoms, sleep problems, and who were subsequently assessed by a psychiatrist and were found to have met the diagnostic criteria for BPD according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) [1]. The healthy control group was selected from among the individuals with demographic characteristics that have matched the patient group in terms of age range and gender, who did not meet the diagnostic criteria in respect of any psychiatric disorder, and who were working as a healthcare professional in the hospital, where the study was conducted. Furthermore, it was checked on the basis of participants’ own statements and medical records whether all the participants included in both the patient and the control groups were literate and whether they were being followed up for any neurological or chronic physical diseases. Accordingly, the participants who were not literate and who were being followed up for a neurological or chronic physical disease were excluded from the study. Additionally, it was also checked whether the participants included in the control group have applied to a psychiatry outpatient clinic in the past, and the participants who were determined to have applied to a psychiatry outpatient clinic in the past were excluded from the control group. Lastly, the participants who were found not to have a menstrual cycle (participants that entered menopause, participants who had amenorrhea, participants who did not menstruate after ovarian surgery, pregnant participants, etc.) were not included in any of the two groups.
The minimum sample size that should be met was found to be 40 (20 patients and 20 controls) as a result of the sample size analysis carried out within the scope of the power analysis, which was performed with reference to α=0.05, 1-β=0.8, 80% power and 95% confidence interval between the groups. In line with the said minimum sample size that should be met, 57 patients diagnosed with BPD according to DSM-5 criteria by two psychiatrists were determined. Out of these 57 patients, 8 patients were excluded from the study due to additional physical illnesses, 6 patients were excluded from the study since they did not answer some of the items in the questionnaires administered, and 5 patients were excluded from the study since their blood samples were incomplete. In addition to the diagnosis of BPD according to DSM-5, 31 patients with a diagnosis of 16 depressive disorder, 13 anxiety disorder, 2 obsessive compulsive disorder were included in the study. In addition, 3 patients with a diagnosis of psychotic disorder and 4 patients with a diagnosis of bipolar affective disorder were not included in the study. In consequence, 31 patients and 31 healthy controls were included in the study.
Research methods
All participants were first evaluated by a psychiatrist, and then a specific date & time was scheduled for each of the participants to separately come to the clinic and to participate in the study on the specified day and time. The clinical interviews were conducted by Dr. K.U. and Dr. F.K. for a duration of approximately 30–45 minutes with each participant. After the interviews, the participants, who were diagnosed with BPD according to DSM-5 diagnostic criteria, were asked to come to the outpatient clinic the next day to give blood samples and to fill in the questionnaires. The participants were administered the Sociodemographic/Clinical Variables Questionnaire by the psychiatrist, and were asked to fill in the Rejection Sensitivity Questionnaire, Childhood Trauma Questionnaire-28 Item Short Form (CTQ-28), and the Relationship Scales Questionnaire on their own. The 10 mL venous blood samples, which were taken from the participants into biochemistry tubes between 08:00 and 09:00 in the morning in order to test their serum oxytocin levels, were let sit for 20 minutes for coagulation. After coagulation had occurred, blood samples were centrifuged at 377.3×g for 10 minutes in order to separate the serums. Serums were then divided into eppendorf tubes, provided that there are two eppendorf tubes for each sample, and stored at -80°C until they were analyzed. Analysis of all blood samples were studied at the same time when the research period was completed. The biochemical analysis of the serum samples were carried out in the biochemistry research laboratory. Oxytocin levels were measured using a BioTek ELx800 (BioTek Instruments, Santa Clara, CA, USA) branded device and an oxytocin human elisa (enzyme-linked immunosorbent assay) kit (Elabscience brand, catalog number: E-EL-0029; Houston, TX, USA) that is specific to the device.
This study was conducted in accordance with the Helsinki Declaration. The ethics committee approval (protocol dated 17/06/20220 numbered 2020/100) of this study was obtained from the Malatya Clinical Research Ethics Committee. Furthermore, written informed consents of all participants were obtained prior to the study.
Data collection tools
Sociodemographic/Clinical Variables Questionnaire
The Sociodemographic/Clinical Variables Questionnaire, which was created by the authors of the study, included sociodemographic data such as gender, educational level, marital status, and employment status as well as clinical data such as the status of receiving any treatment, duration of the medical treatment, if any, familial history of psychiatric illnesses, attempted suicide history and hospitalization history.
Rejection Sensitivity Questionnaire
The Rejection Sensitivity Questionnaire was developed by Downey and Feldman [11], and its Turkish validity and reliability studies were carried out by Göncü Köse et al. [12]. The questionnaire is a self-report 6-point rating scale, which includes 18 items to assess the probable rejection situations. Part (a) of each item assesses the degree of anxiety experienced in a given situation, whereas part (b) of each item assesses the expectations in respect of acceptance or rejection. Eight more items were added to the Turkish version of the scale to account for the differences in respect of the Turkish culture. However, in order not to deviate from the original version of the scale and to render possible the comparison of the Turkish version of the scale with other versions of the scale available in other languages, both the version that include the additional eight items and the version that does not include these additional eight items were taken into consideration. The internal consistency coefficients of these two versions were found as 0.85 and 0.82, respectively [11,12].
Relationship Scales Questionnaire
The 30-item Relationship Scales Questionnaire was developed by Griffin and Bartholomew [13] in 1994 as a 7-point (between 1 pt.=does not describe me at all and 7 pts.=completely describes me) rating self-report scale in order to assess the four attachment styles. The Turkish validity and reliability studies of the scale were carried out by Sümer and Güngör [14] in 1999. In this scale, the participants scored the situation addressed in the respective items and the general attitudes they exhibit in close relationships in the context of the situation specified in the item. Secure and anxious-preoccupied attachment styles are assessed in five items, whereas dismissive-avoidant and fearful-avoidant attachment styles are measured in four items. The scores reflecting the four attachment styles are calculated by adding up the points given to the respective items available in each subscale specific to the attachment style and then by dividing this sum by the number of items available in the respective subscale. Accordingly, the scores that can be obtained from a subscale vary between 1 and 7 and are used for grouping the participants into attachment styles. In the grouping process, each participant is included in the respective attachment style group for which he/she has the highest score. Internal consistency coefficients of the subscales range between 0.27 and 0.61 [13,14].
Childhood Trauma Questionnaire-28 Item Short Form
The Childhood Trauma Questionnaire was developed by Bernstein et al. [15] in 1994. The Turkish validity and reliability studies of the scale, a five-point Likert type self-report scale, were carried out by Şar et al. [16] in 2012. The short form of the scale consists of 28 questions that assess the emotional, physical and sexual abuse and physical and emotional neglect in childhood. The Cronbach’s alpha value of the scale was calculated as 0.93 [15,16].
Statistical analyses
Statistical Package for the Social Sciences (SPSS) version 22 (IBM Corp., Armonk, NY, USA) software package was used to analyze the research data. Kolmogorow Smirnow test was used to analyze the data that conform to the normal distribution. Parametric analyses were conducted in respect of the normally distributed data and non-parametric analyses were conducted in respect of the non-distributed data. The data were presented in the form of arithmetic means, standard deviations, numbers and percentages. The t-test, one-way and two-way analysis of variance tests, Pearson’s correlation test, and Pearson’s chi-squared test were used in the statistical analyses of the data. Probability (p) values of <0.05 were considered to indicate significance.
RESULTS
A total of 62 participants were included in the study. Thirty-one of these participants were female patients who were diagnosed with BPD in accordance with the DSM-5 diagnostic criteria, whereas the remaining 31 participants were healthy control subjects without any psychiatric disorder. Sociodemographic and clinical data of the participants are shown in Table 1.
Oxytocin levels were found to be statistically significantly lower in the patient group compared to the control group. It was determined that the mean CTQ-28 total score and the subscale scores as well as the mean Rejection Sensitivity Questionnaire scores were statistically significantly higher in the patient group than in the control group (Table 2).

Comparison of the mean CTQ-28 and Rejection Sensitivity Questionnaire scores with the oxytocin levels in the patient and control groups
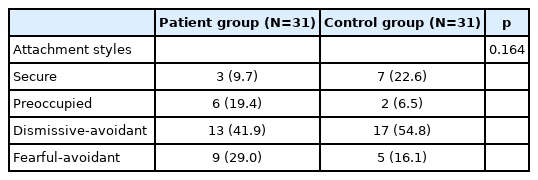
The distribution of attachment styles in the patient and control groups is shown in Table 3. The data on the oxytocin levels in the patient and control groups by the attachment styles are given in Figure 1. Comparison of the oxytocin values with attachment styles revealed a significant difference between the oxytocin levels of the BPD patients values with different attachment styles. Accordingly, it was found that oxytocin levels of the patients with fearful-avoidant and dismissive-avoidant attachment styles were significantly higher than the oxytocin levels of the patients with secure and anxious-preoccupied attachment styles (Table 4).
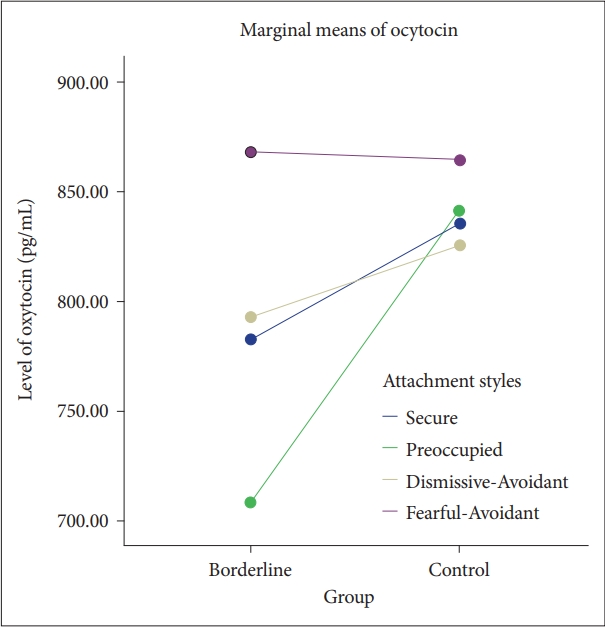
Distribution of the oxytocin levels of the patient and control groups by attachment styles. Two-way ANOVA test.
Data on the correlation between the oxytocin levels and the mean CTQ-28 total and subscale scores and Rejection Sensitivity Questionnaire scores in patient and control groups are given in Table 5. No significant correlation was found between the oxytocin levels and the CTQ-28 subscale scores and the Rejection Sensitivity Questionnaire scores in both the patient and control groups.
DISCUSSION
One of the important findings of this study is that the serum oxytocin levels were found to be significantly lower in the patient group compared to the control group. Similarly, in another study, it was shown that there was a decrease in the plasma oxytocin levels in women diagnosed with BPD, and it was concluded that the dysregulation in the oxytocin system may be an important underlying factor for BPD. 9 Along these lines, in another study, it was shown that there was a decrease in the oxytocin levels as well as in oxytocin receptor protein expression in patients with BPD compared to the control group [17,18]. It has been reported that the low oxytocin levels may be a factor in the abnormal response given to stress and the bottom-up and top-down dysregulation of emotional systems, which is characteristic of BPD [19]. The effect of the low oxytocin levels on the limbic system would cause an unusually high activation of the amygdala, resulting in interpersonal hypersensitivity, emotional dysregulation, and impulsive behavior that are not adequately modulated by the prefrontal cortex [20]. Despite the fact that the finding obtained as a result of this study is compatible with the findings reported in the literature, there are also other studies available in the literature, in which it was demonstrated that not all the samples taken from BPD patients had low blood oxytocin levels [21]. This finding suggests that there are other psychopathological, social and biological mediating factors in the etiology of BPD.
It has been suggested that the abnormalities in oxytocin levels in BPD patients are clinically manifested as misreading of social cues, difficulties in building trust and attachment capacity [20]. In comparison, although the distribution of attachment styles in this study did not reveal any statistically significant difference between the patient and control groups, it was determined that the number of subjects with a secure attachment style were less in the patient group than in the control group. Additionally, in this study, a statistically significant difference was found between the oxytocin levels of those with the anxious-preoccupied and fearful-avoidant attachment styles in the patient group.
Previous studies have shown that female patients with BPD, and the ones with insecure attachment styles in particular, had significantly lower oxytocin levels compared to the control group [22]. In comparison, in this study, it was found that the oxytocin levels were higher among the BPD patients in those with fearful-avoidant attachment style than those with anxious-preoccupied attachment style.
There are also studies in which it was reported that the oxytocin levels in BPD patients may lead to varying results, and thus that the findings in respect of oxytocin levels should be evaluated together with childhood experiences and attachment styles [23]. In comparison, in this study, the fact that a significant relationship was found between the degree of attachment and the oxytocin levels in the patient group, while no such relationship was found between the degree of attachment and the oxytocin levels in the control group, supports the hypothesis that oxytocin plays a role in the etiology of BPD, which is a finding suggesting that further studies are needed to investigate the underlying factors.
It has reported that childhood traumas play an important role in BPD as well as in the development of many personality disorders [24]. In comparison, in this study, it was determined that the total CTQ-28 scores and the scores of all CTQ-28 subscales obtained by the BPD patients were statistically significantly higher compared to the healthy control subjects. Many of the studies, in which the relationship between traumatic childhood experiences and borderline personality organization was investigated, reported a positive significant relationship between the traumatic childhood experiences and borderline personality organization [25-27]. The findings of this study were comparable to such results reported in the literature. However, no statistically significant difference was found between the patient and control groups in terms of the relationship between the CTQ-28 scores and the serum oxytocin levels. It has been reported that the plasma oxytocin levels were found to be low in women diagnosed with BPD, and that these low levels might have stemmed from the traumatic childhood experiences and attachment, as well as serotonin and dopamine (DA) dysregulations, and be associated with decreased social cognition and impaired reward system [28]. Another study, in which the role of the oxytocin receptor gene in the development of BPD symptoms that seem to be associated with gender and traumatic childhood experiences has been investigated on more than 1,000 low-income children, revealed that girls with a history of childhood maltreatment are more susceptible to developing BPD symptoms in the event that they have at least 1 A-allele of single-nucleotide polymorphism rs53576, whereas that boys with a history of childhood maltreatment are more susceptible to developing BPD symptoms in the event that they are homozygous for G/G [29]. In comparison, in this study, childhood traumas were determined to be more common in patients with BPD; however, this finding was not found to be associated with the oxytocin levels. This result, taken together with the fact that the respective results reported in the literature are contradictory, suggests that the etiopathogenesis of BPD should be evaluated from a biopsychosocial perspective and it should not be forgotten that there may be many underlying factors.
Another important finding of this study is that while rejection sensitivity in the patient group was found to be statistically significantly higher than in the control group, no statistically significant relationship was found between the rejection sensitivity and both the oxytocin levels and traumatic childhood experiences. Similarly, it was demonstrated in another study available in the literature that patients diagnosed with BPD had higher rejection sensitivity compared to healthy control subjects [30]. This study was initially based on the hypothesis that there may be an inverse relationship between the oxytocin levels and rejection sensitivity; however, no relationship was found as a result of the study between rejection sensitivity and oxytocin levels, yet the fact that the BPD patients, who had fearful-avoidant attachment style and perceive others as unreliable and rejecting, were found to have significantly higher oxytocin levels can be deemed to indicate the internal consistency of the study.
In another study, the importance of validation of the assumption that high rejection sensitivity stems from the experiences of rejection during the early childhood period, was emphasized to better understand the relationship between BPD and rejection sensitivity [6]. It has been reported that the basis of rejection sensitivity is laid in childhood, that the child, who was raised under disturbing and difficult conditions and who was oppressed, seeks ways to cope with this hostile world, and that these coping methods essentially are fighting strategies involving unconsciously fighting with the original forces that surrounds him/her notwithstanding his/her own weakness and fears [31,32]. In one study, it was reported that the rejection sensitivity caused by emotional neglect and emotional abuse experienced in childhood may have a mediating effect on the development of BPD in the later period. Nevertheless, the results reported in the literature regarding the effects of rejection in childhood and rejection sensitivity on BPD are inconsistent and raise questions about the hypothesized linear relationship related thereto. From among the studies, in which the role of childhood traumas on the relationship between rejection sensitivity and BPD was investigated, there are studies [33-39] which reported that emotional neglect and emotional abuse may play a moderate role on the relationship between rejection sensitivity and BPD, whereas there are also other studies [33,40] which reported that physical neglect and physical abuse may play a low-moderate role on the relationship between rejection sensitivity and BPD in addition to emotional neglect and emotional abuse. However, most of these studies are studies, which were conducted on students with high functionality on the basis of borderline personality traits and not on clinical sample groups. Furthermore, it was also reported that the relationship that was determined between rejection sensitivity and traumatic childhood experiences in these studies is not always valid [6]. Accordingly, it can be speculated that childhood traumas are insufficient to explain the high rejection sensitivity in BPD patients, and that further studies are needed to investigate other factors in relation to the effect of rejection sensitivity on BPD.
Strengths of the study
There are many studies available in the literature in which the relationships between serum oxytocin levels, childhood traumas and attachment styles were examined in BPD patients; however, a thorough review of the literature did not reveal any study other than this one conducted on the relationship between rejection sensitivity and oxytocin levels in BPD patients, indicating, as an important strength of this study, that this is the first study, in which the relationship between rejection sensitivity and oxytocin levels was investigated in BPD patients. In addition, the fact that this study consisted of women in the 18–30 age group encompassing the early adulthood period, is another strength of this study. Another strength of this study is that almost three-quarters of the participants in the study consisted of patients who were diagnosed with BPD for the first time and did not receive any medical treatment.
Limitations of the study
One of the limitations of this study is that neuropeptides such as vasopressin, which are commonly assessed together with oxytocin, were not examined. Thus, follow-up studies in patients with BPD are needed to support the findings of this study.
In conclusion, in this study, it was found that the oxytocin levels were significantly lower and rejection sensitivity and childhood traumas were significantly higher in patients with BPD compared to the healthy control subjects. No significant difference was found in terms of attachment styles, nonetheless it was determined that there may be differences between the oxytocin levels of BPD patients depending on the attachment styles the patients have. Lastly, the fact that rejection sensitivity was not found to be associated with oxytocin levels and childhood traumas in BPD patients as a result of this study, indicates the need to assess the BPD patients in terms of other biopsychosocial factors related to the etiopathogenesis of BPD.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Fatma Kartal, Kerim Uğur. Data curation: Fatma Kartal, Kerim Uğur. Formal analysis: Burak Mete. Funding acquisition: Fatma Kartal, Kerim Uğur, Burak Mete, Mehmet Emin Demirkol. Investigation: Fatma Kartal. Methodology: Fatma Kartal, Kerim Uğur. Project administration: all authors. Resources: Fatma Kartal. Software: Fatma Kartal, Kerim Uğur, Burak Mete. Supervision: Mehmet Emin Demirkol, Lut Tamam. Validation: Burak Mete, Mehmet Emin Demirkol, Lut Tamam. Visualization: Fatma Kartal, Burak Mete. Writing—original draft: Fatma Kartal. Writing—review & editing: all authors.
Funding Statement
None