Smartphone Usage and Sleep Quality in Korean Middle School Students During the COVID-19 Pandemic
Article information
Abstract
Objective
This study evaluated the quality of sleep and smartphone addiction in Korean adolescents during the coronavirus disease 19 pandemic and analyzed their effects on perceived quality of life.
Methods
An online survey system provided by the Gwangmyeong City Health Center located in Gyeonggi-do, Korea, was completed by 1,678 local middle school students from April 1 to June 30, 2021. We measured quality of life using the KIDSCREEN-27 health-related quality of life questionnaire, quality of sleep using the Korean version of the Pittsburgh Sleep Quality Index, and smartphone addiction using the Smartphone Addiction Self-Diagnosis Scale. Bed times, wake times, and total sleep hours were also recorded.
Results
Sleep quality and quantity were directly associated with smartphone addiction. The results indicated that lower quality of life was associated with lower sleep quality, delayed onset of sleep, shorter total sleep time, and higher smartphone addiction. Female students reported lower quality of life, lower sleep quality, delayed sleep phases, shorter total sleep hours, and higher smartphone addiction scores than did male students.
Conclusion
Our results suggest that adolescents’ quality of life is threatened by poor sleep, which in turn could be due to unhealthy smartphone usage. Girls were more heavily affected by this trend than were boys. Preparations to intervene for further mental health issues that might follow are necessary.
INTRODUCTION
Coronavirus disease (COVID-19) pandemic started to spread worldwide in late 2019 and still continues to infect and affect our lives today. The COVID-19 disease has high infectivity and may lead to fatal respiratory failure, especially in vulnerable populations. Effective cure for the disease is still in development, and governments of most countries have concluded that suppression of disease transmission through social distancing is the best viable option. Schools have also been affected by social distancing. Students were asked to stay at home and avoid meeting their peers. School schedules were interrupted at first and then were switched to remote learning through online applications. The South Korean government started these policies in March 2020, and presently, students switch between remote learning periods and actual school attendance (November 2021).
COVID-19 has now been around for more than one and a half years. Concerns about the impact of the pandemic on adolescents’ sleep and everyday life have already been seen in the early stages [1]. Studies have noted that the ‘lockdown’ measures have affected the sleep patterns of youths. Italian researchers found that sleep cycles were significantly delayed in all children and adolescents aged 1–18 years. The most significant delay was observed in school-aged children [2]. Studies in the US have also shown that adolescents have shorter sleep durations, delayed sleep/wake patterns, and more daytime sleepiness as compared to pre-pandemic periods [3], Another subject of concern during the pandemic is increased screen time. Lockdowns and quarantines are now a part of life and nobody can fully avoid them. Universally, more time is spent in front of screens, be it computers, televisions, or smartphones [4], A study in China revealed that screentime increased from 610 min to 2,340 min per week after the outbreak of the pandemic [5]. Smartphones have been around for more than 10 years and have greatly affected our lives. Although smart devices are great tools for coping with stress and boredom, and even help maintain social contacts, they have potentially harmful effects, and caution must be taken while using them [6].
They impact sleep in many ways: the bright light suppresses melatonin secretion, associated emotional or cognitive effects result in sleep problems, and messages or alarms may directly wake an individual during sleep [7]. Screentime has increased greatly during the pandemic, and smartphones play a significant role in this trend. Digital devices are not all bad. In times of mandatory social distancing, they helped continue education, provide psychological support, and served as a source of entertainment [8,9].
The effect of poor sleep on quality of life (QoL) is not novel. Decreased sleep quality has been found to induce daytime sleepiness, poor academic performance, obesity, and even cardio-metabolic problems, and such changes contribute to a lower QoL [10]. Poor sleep also directly affects the QoL of adolescents alongside fewer physical activities and more sedentary behavior, as has been shown in a South Australian study on high school students [11].
It is clear that the COVID-19 era has had an impact on the lives of children and adolescents worldwide, but the actual specific changes in life and their secondary influences have not yet been concretely discussed. It is important to investigate the type and depth of such impacts to prepare ourselves, since “living together with COVID-19” is no longer a distant mirage. We hypothesized that the increase in screen time, which is caused by excessive smartphone addiction in children and adolescents, would affect the quality of sleep, and at the same time, decreased the quality of sleep would affect their QoL. To provide practical evidence, we collected and analyzed data regarding the current state of sleep, smartphone use, and QoL of Korean adolescents.
METHODS
Participants and procedure
Data was collected from April 1, 2021, to June 30, 2021, using an online web-based survey system provided by the Gwangmyeong City Health Center. The survey targeted circa 9,000 students from all 12 local middle schools in the Gwangmyeong area, from which 1,678 students responded. The questionnaire collected demographic data, including age, sex, and clinical data, using various rating scales. QoL was measured using the KIDSCREEN-27 health-related quality of life questionnaire (KIDSCREEN-27), quality of sleep using the Korean version of the Pittsburgh Sleep Quality Index (PSQI-K), and smartphone addiction using the Smartphone Addiction Self-Diagnosis Scale (S-Scale). For additional sleep data, participants were asked to provide their typical bed-time and wake-time. The total sleep hours were calculated using this information.
All participants and parents provided written informed consents. The study was approved by the Institutional Review Board of the Korea Medical University (IRB No. 2021GR0455).
Measures
Quality of life
The KIDSCREEN-27 health-related quality of life questionnaire is a shorter version of the KIDSCREEN-52 questionnaire, an instrument for measuring subjective QoL in children and adolescents. This is the first questionnaire to be developed simultaneously in different countries and tested on large samples of various cultural backgrounds [12]. Compared to its 52-item version, the KIDSCREEN-27 saves administrative costs and burdens to ensure wider use in clinical studies, and studies have verified its construct validity [13]. The questionnaire has five dimensions: physical well-being, psychological well-being, parent relationship and autonomy, social support and peers, and school environment. Scores range from 1 to 5, where higher numbers generally represent better QoL, but some questions are calculated in reverse. Scores were finally computed and transformed into values with a mean of 50 and a standard deviation of 10 (T-score) for analysis [14].
Quality of sleep
The PSQI is typically used, worldwide, to measure sleep quality in the previous months in a self-reporting manner [15]. PSQI-K was standardized and evaluated for reliability and validity [16]. The questionnaire consists of 18 items and considers both qualitative and quantitative aspects of sleep. Each item is scored from 0 to 3, resulting in a total score of 0 to 21. Greater scores are associated with poorer sleep quality, and scores higher than or equal to 5 indicate significantly disturbed sleep quality, and scores higher or equal to 9 indicate clinical levels of sleep disturbance.
Smartphone addiction
The S-Scale is a derivative of the Korean scale for Internet addiction (K-scale) [17]. The K-scale was developed by the Korea National Information Society Agency to assess Internet addiction behaviors [18], The S-Scale is very similar to the K-scale but concentrates on the use of smartphones rather than generalized Internet use. The scale consists of 15 questions in four categories: disturbance of adaptive functions, virtual life orientation, withdrawal, and tolerance. Each question was scored from 1 to 4, resulting in a total score of 15 to 60. Users are divided into three groups: normal users (<42), tentatively risky users (42–44), and high-risk users (>44).
Statistical analyses
All statistical analyses were performed using the SPSS software version 25 (IBM Corp., Armonk, NY, USA). Pearson’s correlation analysis was performed to investigate the correlations between the demographic and clinical variables and their impact on the QoL of the participants. Student’s t-tests were then performed to compare the means of clinical variables between male and female students. The significance level was set at p<0.05.
RESULTS
Demographic and clinical data
A total of 1,678 participants were initially included in the study. Fourteen participants failed to complete all questions on the online questionnaire, and 17 participants did not provide adequate demographic information; thus, 31 participants were excluded. A total of 1,647 participants with a mean age of 13.83±0.95 years were included in the final analysis; of them, 784 (47.60%) were male and 863 (52.40%) were female.
The mean total KIDSCREEN scores for all participants were 96.17±14.92. Scores for component dimensions were as follows: physical well-being, 15.10±1.61; psychological well-being, 25.80±4.87; parent relationship & autonomy, 26.01±5.50; social support & peer, 14.66±3.55; and school environment, 14.60±3.18.
The mean PSQI-K scores were 6.09±3.01. A total of 486 (29.51%) participants had PSQI scores of 4 or lower, indicating no sleep disturbance. A total of 852 (51.73%) participants had scores between 5 and 8, showing significantly disturbed sleep quality, and 309 (18.76%) participants had scores of 9 or higher, indicating clinical levels of sleep disturbances.
The mean S-Scale scores were 30.33±6.97. A total of 1,574 (95.57%) participants had scores of 41 or lower, indicating normal smartphone usage, 45 (2.73%) participants had scores between 42 and 44, showing tentatively risky smartphone usage, and 28 (1.70%) participants had scores of 45 or higher, indicating high-risk smartphone usage.
The average bed-time for participants was 00:13 (h:min), and the average wake-time was 07:42 (h:min), resulting in an average total sleep of 7.49±1.44 hours. Further details are presented in Table 1.
Pearson’s correlation analysis
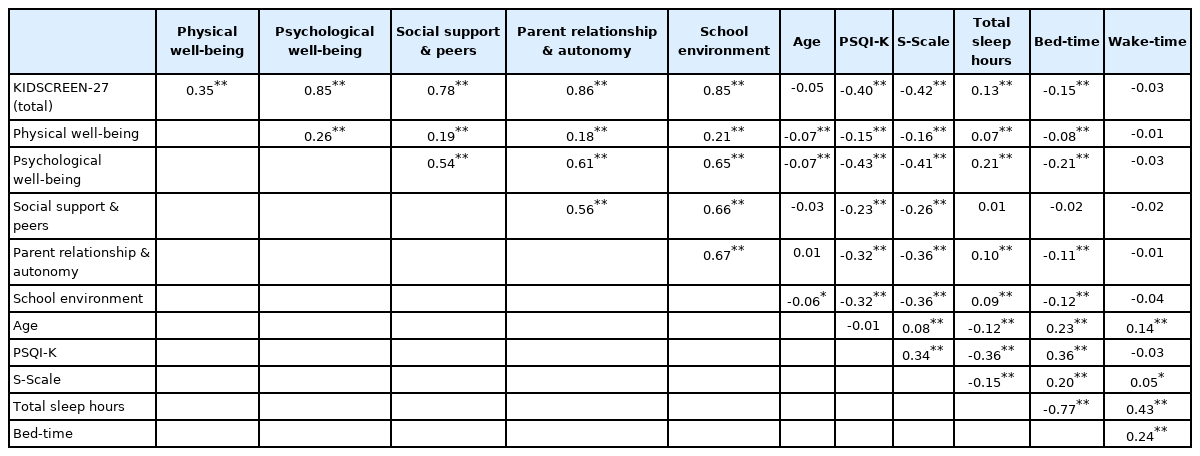
Total KIDSCREEN-27 scores were negatively correlated with PSQI-K scores (r=-0.40**), S-Scale scores (r=-0.42**), and bedtime (r=-0.15**), and positively correlated with total sleep hours (r=0.13**) (r, correlation coefficient; *p<0.05, **p<0.01). The five subdimensions also showed similar results. Physical well-being scores were negatively correlated with PSQI-K scores (r=-0.15**), S-Scale scores (r=-0.16**), age (r=-0.07**), and bedtime (r=-0.08**), and positively correlated with total sleep hours (r=0.07**). Psychological well-being scores were negatively correlated with PSQI-K scores (r=-0.43**), S-Scale scores (r=-0.41**), age (r=-0.07**), and bedtime (r=-0.21**), and positively correlated with total sleep hours (r=0.21**). Parent relationship and autonomy scores were negatively correlated with PSQI-K (r=-0.32**), S-Scale (r=-0.36**), and bedtime (r=-0.11**), and positively correlated with total sleep hours (r=0.10**). Social support and peer scores were negatively correlated with the PSQI-K (r=-0.23**) and S-Scale scores (r=-0.26**). School environment scores were negatively correlated with PSQI-K scores (r=-0.32**), S-Scale scores (r=-0.36**), age (r=-0.06*), and bedtime (r=-0.12**), and positively correlated with total sleep hours (r=0.09**). The PSQI-K scores were negatively correlated with total sleep hours (r=-0.36**) and positively correlated with S-Scale scores (r=0.34**) and bedtime (r=0.36**). The S-Scale scores were negatively correlated with total sleep hours (r=-0.15**) and positively correlated with age (r=0.08**), bedtime (r=0.20**), and wake time (r=0.05*). Further details of the correlation analysis are presented in Table 2.
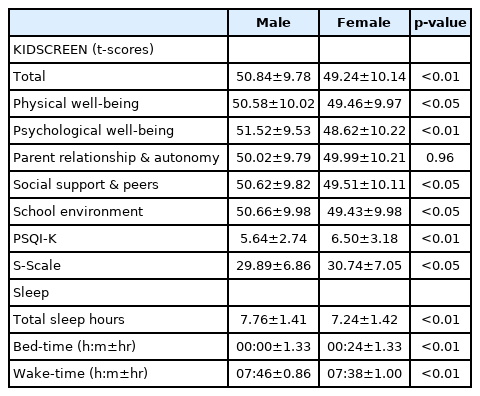
t-test analysis
Female students showed significantly lower total KIDSCREEN-27 scores than male students. All component scores were also lower for female students, but parent relationship and autonomy scores did not show statistically significant differences between male and female students. Female students also showed significantly higher PSQI-K and S-Scale scores than male students. They also reported significantly later bedtime, earlier wake-times, and shorter total sleep hours. The details are listed in Table 3.
DISCUSSION
The COVID-19 era involves social distancing, lockdowns, and quarantines. Students were stripped off of their right to go to school, and remote learning became the new standard, worldwide. Staying at home led to changes in everyday lifestyle. As previous studies have already suggested, adolescents had delayed sleep patterns and greatly increased screentime as compared to pre-pandemic times. Although children and adolescents were largely unaffected in terms of mortality in COVID-19, such changes heavily affected their subjective QoL. Notably, this change was not one-sided. Many families were forced to reinvent their ways of spending time, staying at home together, or doing activities in the open outdoors, since indoor facilities were mostly closed. Online schooling led parents to play the role of a home teacher. These changes led to positive experiences for certain children and families [19]. In fact, a Canadian study revealed that many children and adolescents showed deteriorations in various mental health domains, but large groups experienced improvements in at least one domain [20]. Our current knowledge indicates that strict quarantine measures and vulnerabilities such as pre-existing psychiatric disorders result in a more negative QoL [21,22]. It is therefore important to identify groups that are at a higher risk of mental health deterioration to prepare for later interventions. Various nationwide studies have shown that children and adolescents reported lower QoL during the pandemic, indicating that they are candidates for such vulnerabilities [23-25]. Our study targeted Korean middle school students and indicated that lower KIDSCREEN-27 scores, and lower QoL were associated with lower quality of sleep, more smartphone use, less total sleep hours, and later bedtime. Heavy smartphone use was also directly associated with poor sleep quality and delayed sleep patterns.
QoL was most heavily impacted by quality of sleep and smartphone use (r=-0.40, -0.42, respectively), and less by sleep hours and bedtime (r=0.13, -0.15, respectively). Although all subdimensions of KIDSCREEN-27 were affected, the greatest impact of sleep and smartphone use was on psychological well-being, and the least impact was on physical well-being. This confirms again that COVID-19 pandemic does not only threaten the physical health but also overtly affects the mental health of children and adolescents. It is also concerning that school environment, parent relationship, and social support are also impacted much heavier than physical well-being. It is an egg and chicken paradox, but the cut-down social life quality of adolescents (including school and family) could be either due to or the reason for poorer sleep and more smartphone use.
Our results indicated that students with lower sleep quality also reported lower QoL. It is a worldwide phenomenon that youths have shown deteriorated sleep patterns after the pandemic, but our concern is that many participants reported high levels of sleep disturbance. In fact, 70.45% of participants had scores of 5 or higher, indicating a significant disturbance of sleep, and 18.75% had scores of 9 or higher, being recommended to seek a sleep professional as soon as possible. Previous studies have already confirmed that adolescent sleep patterns worsened during the pandemic [26-28], and one of the possible contributing factors might be increased screentime.
Our results showed that higher S-Scale scores were associated with lower sleep quality and delayed sleep phases. High S-Scale scores mean that the individual has a hard time being abstinent from a smartphone, resulting in a longer screentime and problematic daily life due to such behavior. As a matter of fact, media use was identified as a major tool to cope with stress and mood problems [29]. Our results also showed that more smartphone use was associated with slightly higher psychological well-being scores of KIDSCREEN-27, possibly due to such stress-relieving roles. Nevertheless, we must not avoid the problems that smartphones accompany. Increased screentime and smartphone use are not only associated with health hazards such as obesity, hypertension, myopia, and diabetes, but also with psychological problems such as depression or sleep problems [30]. The increased use of digital devices during the pandemic led to corresponding growths of such problems worldwide, and experts are addressing that this trend is still ongoing [31-33]. Problems associated with excessive smartphone use were not an unknown menace, but the pandemic hit the world hard and quick, countermeasures had to be deployed on par, and now it seems like we are facing the consequences of such rapid and unprepared changes.
This study also revealed that girls reported poorer QoL, sleep quality, and riskier smartphone use habits than boys. The general literature states that girls have higher levels and prevalence of depression, anxiety, and sleep problems [34,35]; possibly, girls were more heavily impacted by social distancing measures than boys. Recent studies on the influence of the pandemic on mental health report that women are at an especially high risk for developing mental health issues, although it has to be mentioned that the paper only concerned women of fertile age spectrums [36]. A systematic review on the impact of COVID-19 on mental health indicated that female gender is indeed a risk factor for higher psychiatric symptoms and lower psychological well-being in the general population [37]. Canadian researchers also reported that girls had more pronounced effects on academy and social life than boys. They also suggested that females use social media more frequently as a coping mechanism for stress than males [38]. These results are in line with ours, proposing social media use as a possible variable that hides behind the link between smartphone use and QoL.
An additional factor that may mediate the effects of the pandemic on smartphone use is socioeconomic status (SES). Although related data were not gathered in this study, high SES has been known to be generally protective of the burdens imbued by the pandemic on children and adolescents [39]. Populations with low SES are considered high-risk groups for several reasons. First, economic pressure hits the family budget harder, leading to less healthy family interactions. Second, there are disparities regarding the availability of appropriate gear and internet connections for home schooling or diverse leisure activities [40]. The latter leads to a greater gap in education levels, and technological access turning education from the right to a privilege is becoming a major problem [41]. Even before the pandemic, low SES was associated with more problematic smartphone use in Korea [42]. Possibly, parents with lower SES spend more time at work, leaving their children in a less supervised environment for using smartphones, a tendency that might have worsened during the pandemic. Considering our results, adolescents with lower SES might have suffered harder drops in sleep quality and QoL due to the increase in smartphone usage.
There are several limitations to our study. First, due to its cross-sectional design, data before the onset of the pandemic were not available. Baseline data on QoL or sleep quality could have led to a more detailed analysis of the effect of social distancing on clinical variables. Second, difficult and time-consuming questions were not used for this online survey. Although, social distancing guidelines made it near impossible, offline questionnaires with supervisors would have allowed for more diverse information to be collected, and less participants would have been excluded due to wrongly answered questions. Third, all participants were middle school students from a particular area. Although the participant numbers were large, the whole group had similar ages and lived in the same region, which may limit the generalization of the study results. Fourth, only 1,678 students out of circa 9,000 responded to the original questionnaire. Since its design was an online questionnaire, respondents might have been closer to smartphones than non-respondents, resulting in biased S-Scale scores. Fifth, our original questionnaire did not include clinical rating scales on depression or anxiety. It is possible that psychiatric disorders might have contributed to altered sleep patterns or smartphone using patterns which could have affected our results. Nevertheless, our study on a large homogeneous group during this pandemic is important for understanding the risks for the mental health of adolescents.
In conclusion, the COVID-19 era is not yet a part of history; it is an ongoing event that seems to have no proper finale. The current increase in smartphone usage and the associated drop in sleep quality and QoL will continue, if not worsen. Sitting still and hoping for a natural reversal is no longer an option. Our results showed that adolescents, especially girls, are at increased risk for various mental health issues that are associated with poor sleep and smartphone addiction. We advise that proper administrative preparations should be taken for appropriate interventions on mental health problems that might emerge in the future.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Suhyuk Chi, Moon-Soo Lee. Data curation: Suhyuk Chi, Jong-ha Lee. Formal analysis: Suhyuk Chi, Min-soo Ko. Funding acquisition: Hyun-suk Yi. Methodology: Suhyuk Chi, Moon-Soo Lee. Writing—original draft: Suhyuk Chi, Moon-Soo Lee. Writing—review & editing: Moon-Soo Lee.
Funding Statement
This research was supported by the COVID-19 Disaster Psychological Support Program through the Gwangmyeong Mental Health Welfare Center funded by the Gwangmyeong City Health Center.
Acknowledgements
The authors would like to thank all the participants in our study.