 |
 |
- Search
| Psychiatry Investig > Volume 20(11); 2023 > Article |
|
Abstract
Objective
Methods
Results
Notes
Availability of Data and Material
Hyung-Jun Yoon had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Eun Hyun Seo, Hyung-Jun Yoon. Data curation: Eun Hyun Seo, Hyung-Jun Yoon. Formal analysis: Seung-Gon Kim, Jae-Hon Lee, Hyung-Jun Yoon. Funding acquisition: Hyung-Jun Yoon. Investigation: Eun Hyun Seo, Seung-Gon Kim, Jae-Hon Lee, Chandlee C. Dickey, Hyung-Jun Yoon. Methodology: Mella Y. Kim, Ravneet Kaur Ghumman. Project administration: Hyung-Jun Yoon. WritingŌĆöoriginal draft: Eun Hyun Seo, Hyung-Jun Yoon. WritingŌĆöreview & editing: Jae-Hon Lee, Chandlee C. Dickey, Mella Y. Kim, Ravneet Kaur Ghumman.
Funding Statement
This study was supported by research fund from Chosun University(2022).
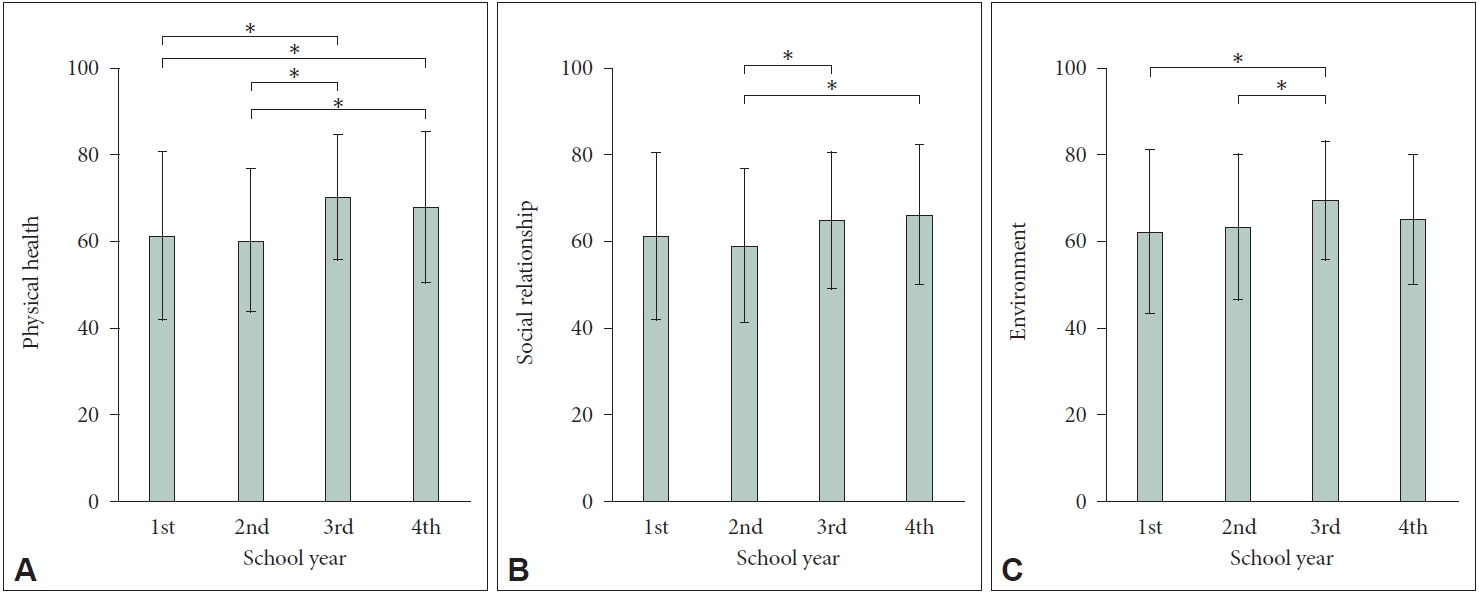
Figure┬Ā1.
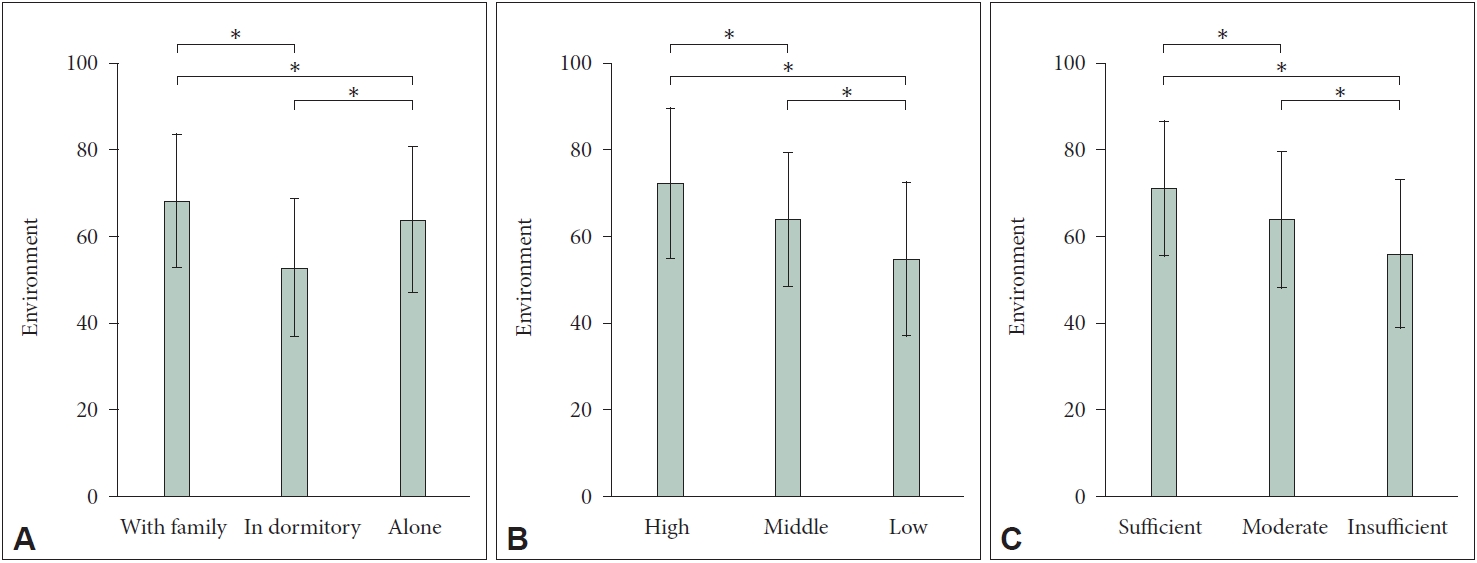
Figure┬Ā2.
Table┬Ā1.
Table┬Ā2.
| Variables |
WHOQOL-BREF |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Physical health | p | Psychological health | p | Social relationships | p | Environment | p | ||
| Sex | 0.041* | 0.020* | 0.658 | 0.022* | |||||
| Male | 66.2┬▒17.4 | 62.9┬▒19.6 | 62.4┬▒18.9 | 66.3┬▒17.0 | |||||
| Female | 62.3┬▒17.7 | 58.2┬▒18.7 | 63.5┬▒14.9 | 62.6┬▒15.8 | |||||
| School year | <0.001*** | 0.399 | 0.013* | 0.002** | |||||
| First-year | 61.3┬▒19.4 | 58.5┬▒22.6 | 61.3┬▒19.2 | 62.2┬▒19.0 | |||||
| Second-year | 60.2┬▒16.5 | 59.2┬▒20.0 | 59.0┬▒17.7 | 63.3┬▒16.9 | |||||
| Third-year | 70.2┬▒14.5 | 63.1┬▒16.3 | 64.8┬▒15.8 | 69.5┬▒13.8 | |||||
| Fourth-year | 67.9┬▒17.5 | 64.4┬▒16.8 | 66.2┬▒16.2 | 65.1┬▒15.0 | |||||
| Residence | 0.509 | 0.475 | 0.285 | 0.001** | |||||
| With family | 66.3┬▒18.2 | 62.4┬▒19.2 | 64.6┬▒16.6 | 68.3┬▒15.4 | |||||
| Dormitory | 62.3┬▒17.3 | 57.1┬▒17.7 | 58.2┬▒15.0 | 52.9┬▒15.9 | |||||
| Alone | 64.2┬▒17.4 | 60.9┬▒19.6 | 62.2┬▒18.1 | 64.0┬▒16.9 | |||||
| Self-perceived SES | 0.602 | 0.471 | 0.869 | <0.001*** | |||||
| High | 66.7┬▒17.6 | 63.1┬▒20.8 | 63.1┬▒20.8 | 72.4┬▒17.4 | |||||
| Middle | 64.3┬▒17.1 | 60.9┬▒18.9 | 62.9┬▒16.4 | 64.0┬▒15.5 | |||||
| Low | 63.7┬▒22.2 | 58.9┬▒20.3 | 60.6┬▒18.9 | 54.9┬▒17.8 | |||||
| Self-perceived pocket money | 0.540 | 0.199 | 0.187 | <0.001*** | |||||
| Sufficient | 66.7┬▒16.7 | 63.7┬▒18.5 | 65.0┬▒17.3 | 71.2┬▒15.6 | |||||
| Moderate | 63.9┬▒18.0 | 60.4┬▒20.0 | 62.3┬▒17.6 | 64.0┬▒15.8 | |||||
| Insufficient | 64.1┬▒17.7 | 59.1┬▒18.3 | 60.3┬▒17.3 | 56.1┬▒17.2 | |||||
Table┬Ā3.
| Variables |
WHOQOL-BREF |
|||
|---|---|---|---|---|
| Physical health | Psychological health | Social relationships | Environment | |
| BDI | -0.628*** | -0.649*** | -0.512*** | -0.470*** |
| IAT | -0.330*** | -0.361*** | -0.292*** | -0.266*** |
| RSES | 0.600*** | 0.771*** | 0.582*** | 0.535*** |
| Duke-UNC FSSQ | 0.457*** | 0.465*** | 0.473*** | 0.383*** |
Table┬Ā4.
| Variables | Standardized ╬▓ | t | p |
|---|---|---|---|
| Physical health | |||
| ŌĆāSchool year (reference group: first-year) | |||
| ŌĆāŌĆāThird-year | 0.075 | 2.272 | 0.024* |
| ŌĆāBDI | -0.364 | -7.729 | <0.001** |
| ŌĆāIAT | -0.118 | -3.357 | 0.001** |
| ŌĆāRSES | 0.321 | 7.040 | <0.001*** |
| ŌĆāDuke-UNC FSSQ | 0.109 | 2.787 | 0.006** |
| ŌĆāR2=0.577, Adjusted R2=0.572, F=109.843, p<0.001 | |||
| Psychological health | |||
| ŌĆāBDI | -0.253 | -6.750 | <0.001*** |
| ŌĆāIAT | -0.077 | -2.728 | 0.007** |
| ŌĆāRSES | 0.569 | 15.512 | <0.001*** |
| ŌĆāDuke-UNC FSSQ | 0.096 | 3.035 | 0.003** |
| ŌĆāR2=0.724, Adjusted R2=0.721, F=264.225, p<0.001 | |||
| Social relationships | |||
| ŌĆāBDI | -0.119 | -2.297 | 0.022* |
| ŌĆāIAT | -0.106 | -2.722 | 0.007** |
| ŌĆāRSES | 0.370 | 7.319 | <0.001*** |
| ŌĆāDuke-UNC FSSQ | 0.272 | 6.271 | <0.001*** |
| ŌĆāR2=0.476, Adjusted R2=0.471, F=91.666, p<0.001 | |||
| Environment | |||
| ŌĆāSchool year (reference group: first-year) | |||
| ŌĆāŌĆāThird-year | 0.081 | 2.200 | 0.028* |
| ŌĆāResidence (reference group: with family) | |||
| ŌĆāŌĆāDormitory | -0.145 | -3.897 | <0.001*** |
| ŌĆāŌĆāAlone | -0.129 | -3.373 | 0.001** |
| ŌĆāSelf-perceived SES (reference group: high) | |||
| ŌĆāŌĆāMiddle | -0.174 | -3.964 | <0.001*** |
| ŌĆāŌĆāLow | -0.187 | -4.320 | <0.001*** |
| ŌĆāSelf-perceived pocket money (reference group: sufficient) | |||
| ŌĆāŌĆāModerate | -0.087 | -2.019 | 0.044* |
| ŌĆāŌĆāInsufficient | -0.225 | -5.213 | <0.001*** |
| ŌĆāBDI | -0.161 | -3.106 | 0.002** |
| ŌĆāIAT | -0.103 | -2.633 | 0.009** |
| ŌĆāRSES | 0.336 | 6.671 | <0.001*** |
| ŌĆāDuke-UNC FSSQ | 0.126 | 2.915 | 0.004** |
| ŌĆāR2=0.505, Adjusted R2=0.492, F=36.679, p<0.001 |
REFERENCES
-
METRICS

-
- 0 Crossref
- Scopus
- 966 View
- 34 Download
-
Longitudinal Impact of Depression on Quality of Life in Stroke Patients2018 February;15(2)
Associated Factors of Quality of Life in First-Episode Schizophrenia Patients2011 September;8(3)






