Diagnostic Issues of Depressive Disorders from Kraepelinian Dualism to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
Article information
Abstract
Because the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) was mainly influenced by the neo-Kraepelinian approach, its categorical approach to defining mental disorders has been criticized from the viewpoint of etiological neutrality. In the context of bridging the gap between “presumed etiologies-based symptomatology” and “identifiable pathophysiological etiologies,” the content in 5th edition, the DSM-5, has been revised to incorporate a combination of categorical and dimensional approaches. The most remarkable change of note regarding the diagnostic classification of depressive disorders in the DSM-5 is the splitting of mood disorders into bipolar disorders and depressive disorders, which is in accordance with the deconstruction of the Kraepelinian dualism for psychoses. The transdiagnostic specifiers “with mixed features,” “with psychotic features,” and “with anxious distress” are introduced to describe the relationships of depressive disorders with bipolar disorders, schizophrenia, and generalized anxiety disorder, respectively, in a dimensional manner. The lowering of the diagnostic threshold for major depressive disorder (MDD) may be caused by the addition of “hopelessness” to the subjective descriptors of depressive mood and the elimination of “bereavement exclusion” from the definition of MDD. Since the heterogeneity of MDD is equivalent to the Wittgensteinian “games” analogy, the different types of MDD are related not by a single essential feature but rather by “family resemblance.” Network analyses of MDD symptoms may therefore need further review to elucidate the connections among interrelated symptoms and other clinical elements.
INTRODUCTION
The Diagnostic and Statistical Manual of Mental Disorders (DSM) has a tendency to resist change and the revision of its content, consistent with the statement that “the Catholic Church changes its Pope more often than the American Psychiatric Association (APA) publishes a new version of the DSM.” [1] The DSM has been revised five times between 1952 and 2013. The first incarnations, the DSM-I (1952) and DSM-II (1968) were based on psychoanalytic and psychodynamic theories and had shortcomings in terms of their arbitrariness and inconsistency in defining the diagnoses for mental disorders. The “DSM-III revolution (1980),” which refers to the increasing trends that occurred in logical positivism and biological psychiatry, was subsequently proposed in order to overcome criticism based on the Rosenhan experiment findings, the antipsychiatry movement, and public debates regarding the distinctive unclearness of the DSM-I and DSM-II. Thus, in the DSM-III, mental disorders were defined from a categorical viewpoint that was based on the operational diagnostic system characterized by a descriptive approach, explicit inclusion and exclusion criteria, algorithms for diagnostic criteria, a nominalist definition, etiological neutrality, and a quantitative approach. Then, in the DSM-IV (1994), consistent with empirical trends, the tendency to define psychiatry as a part of biomedicine was further strengthened [2,3].
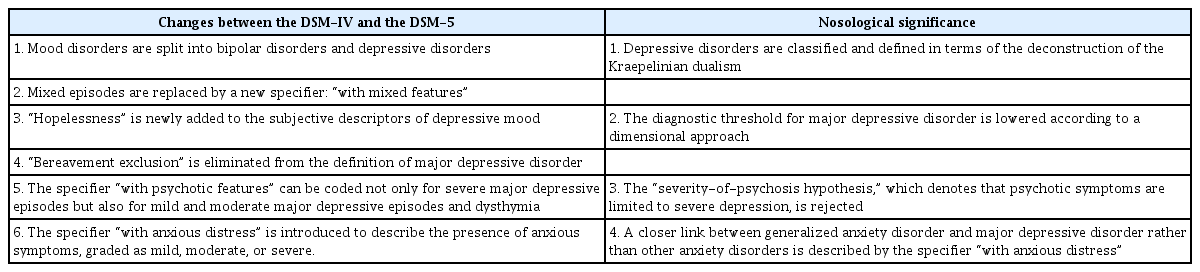
Steven Hyman [1], a former director of the National Institute of Mental Health, criticized the DSM, saying “the problem is that (the) DSM has been launched into under-researched waters, and this has been accepted in an unquestioning way.” Thus, the construction of a “paradigm shift in psychiatry” from a “symptom-based classification system” to an “etiology-based classification system” was proposed during the revision process of the DSM-5 [4-6]. Since the DSM-5 task force realized, however, that this goal was wildly premature, a dimensional approach characterized by the introduction of numerical scales was alternatively regarded as its major innovation. It was thus suggested that dimensional measurements rather than diagnostic categories contribute to a valid, biologically based, and scientifically sound classification system in psychiatry [7]. However, the dimensional scales were relegated to the appendix of the DSM-5 for further study by the APA assembly since the severity scales were not validated and an undue burden was imposed upon clinicians [8]. Moreover, an editorial article authored by Allan Frances [9], who had been the chair of the DSM-IV task force, titled “Diagnosing the DSM,” was published in the New York Times on May 11, 2012. In this article, the DSM-5 was labeled a “promise to be a disaster.” As a result, a combination of categorical and dimensional approaches was introduced for the definition of mental disorders in the DSM-5 (2013), since the aims of the DSM-5 task force shifted toward bridging the gap between “presumed etiologies-based symptomatology” and “identifiable pathophysiological etiologies.” [10] The failure of the task force to achieve a radical paradigm shift was explained as the result of “grand ambition, furious resistance, and the derailment of the DSM-5 revision process,” by Whooley and Horowitz [7]. However, the DSM-5 revision process has also been praised for “opening the door to questions about future psychiatry” in terms of categorical and dimensional approaches to mental disorders. Table 1 summarizes the changes in diagnostic classifications and criteria for depressive disorders between the DSM-IV and DSM-5 [11,12]. Herein, we sought to review and discuss the categorical and dimensional approaches to depressive disorders in the context of the changes during the move from the DSM-IV to the DSM-5 that were made to diagnostic classifications and criteria for depressive disorders.
DICHOTOMIZING MOOD DISORDERS INTO BIPOLAR DISORDERS AND DEPRESSIVE DISORDERS AND REPLACING MIXED EPISODES WITH MIXED FEATURES
The dichotomization of the chapter, “Mood Disorders,” into two chapters called “Bipolar and Related Disorders” and “Depressive Disorders” has been one of the most notable changes to the diagnostic classifications for depressive disorders made between the DSM-IV and the DSM-5 [11,12]. An odd combination of the classical views of Emil Kraepelin and Karl Leonhard (a follower of Carl Wernicke, Kraepelin’s opponent) contributed to the definitions underlying the nosology of mood disorders in the DSM-III and DSM-IV. Kraepelin’s classical distinction between dementia praecox (chronic psychosis) and manic-depressive insanity (recurrent mood illness with psychosis) was extended to include manic-depressive illness (nonpsychotic mood episodes) by later researchers. Thus, in line with Wernicke’s opposition of Kraepelin’s manic-depressive illness concept, Leonhard insisted that manic-depressive illness was composed of two distinctive subtypes including unipolar depression and bipolar disorder, based on findings from genetic research. In the DSM-III, the Kraepelinian separation of schizophrenia from mood disorders was, in an odd way, combined with the Leonhardian dichotomization of mood disorders into the two unipolar and bipolar groupings. Moreover, in the DSM-IV, following a rather pragmatic approach, the unipolar depression concept was expanded to major depressive disorder (MDD), potentially influenced by a preference to prescribe antidepressants rather than lithium and neuroleptics, due to side effects [13-16]. The finding that bipolar and depressive disorders overlap symptomatically and genetically to a degree that is similar to schizophrenia and depressive disorders led to the dichotomization of mood disorders into bipolar disorders and depressive disorders in the DSM-5 [17-19]. The dichotomization into bipolar disorders and depressive disorders is thus consistent with the deconstruction of the Kraepelinian dualism for psychoses, which denotes the reclassification of schizophrenia and bipolar disorder in terms of a dimensional rather than a categorical approach [13-16]. From the perspective of a paradigm shift from a categorical to a dimensional approach, the dichotomization of mood disorders carries nosological significance, in that MDD is now considered to be a distinctive disease entity parallel to schizophrenia and bipolar disorder.
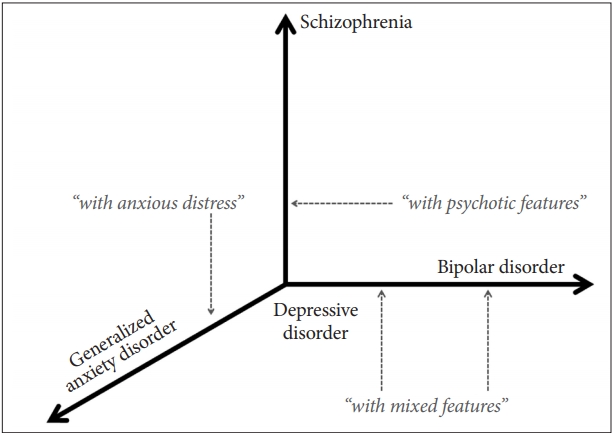
However, the dichotomization into bipolar disorders and depressive disorders is partly inconsistent with the fact that the conversion from depressive disorders to bipolar disorders is one of the most significant conversions to occur in psychiatric taxonomy [20,21]. It has been speculated that the completely distinctive definitions of predominantly manic and depressive episodes may have contributed to the removal of the “mixed episode” type in the DSM-5. Moreover, the dichotomization has been theoretically or nosologically supplemented by the replacement of the “mixed episode” with a new coding specifier, “with mixed features,” in the DSM-5 [11,12]. The “mixed episode” has been conceptualized in the DSM-IV from the perspective of a categorical approach, whereas the “with mixed features” in the DSM-5 has been defined from the perspective of a dimensional approach. The specifier “with mixed features” can be coded during all episodes-manic, hypomanic, or depressive. Further, the subthreshold bipolar features during a predominantly depressive episode are coded by the specifier “with mixed features,” denoting the presence of at least three of seven hypomanic symptoms including elevated mood, inflated self-esteem, pressure of speech, racing thoughts, goal-directed activity, involvement in risky activities, and decreased need for sleep. However, arguments have been raised that hypomanic expansive symptoms in mixed depression have rarely been reported in previous studies and that mixed depression is a separate condition in the context of mood disorders [22-24]. Moreover, recent studies have reported that major depressive episode (MDE) mixed features are characterized by a low prevalence, the predominance of anxious distress, the prevalence of cluster B personality disorders, and pharmacological treatment with antipsychotics [25-27]. Thus, as shown in Figure 1, the specifier “with mixed features” may indicate quantitative but not qualitative overlapping symptoms from one pole to the opposite pole in the dichotomization of mood disorders into bipolar and depressive disorders.
ADDITION OF “HOPELESSNESS” TO THE SUBJECTIVE DESCRIPTORS OF DEPRESSIVE MOOD AND THE ELIMINATION OF “BEREAVEMENT EXCLUSION” FROM THE DEFINITION OF MDD
The term “hopelessness,” which is consistent with the mention of a “black and pessimistic view of the future” contained in the definition of depressive mood in the International Classification of Disease, 10th revision (ICD-10), has newly been added to the subjective descriptors of depressive mood in the DSM-5 [11,12]. Since “hopelessness” is regarded as a cognitive attitude of pessimism rather than a specific emotional state and since it can be present despite the absence of depressive mood, it represents a distinctive feature. In addition, the “bereavement exclusion” has been eliminated from the definition of MDD in the DSM-5, based on the few significant differentiating clinical features between bereavement-related and bereavement-unrelated depressive disorders and the characterization of bereavement-related MDD with past personal histories and family histories of MDEs [28-30]. The addition of “hopelessness” to the subjective descriptors of depressive mood has therefore broadened the diagnosis of MDD.
Separately, the elimination of the “bereavement exclusion” from the definition of MDD has likely lowered the diagnostic threshold for MDD and contributed to the medicalization of normal grief. As the less severe forms of MDD, such as low-symptom and non-melancholic MDD, are characterized by lower recurrence rates as compared with other forms of MDD [31-33], the appropriate threshold for the differentiation of MDD from normal sadness needs to be further explored and precisely defined in the context of either a categorical or a dimensional approach.
WITTGENSTEIN’S “GAMES” ANALOGY AND THE HETEROGENEITY OF MDD
Although a simplified list of the symptom criteria for MDD, consisting of low mood, loss of interest or pleasure, guilt/worthlessness, impaired concentration/indecision, and suicidal thoughts, has been developed by Zimmerman et al. [34], the list of nine depressive symptoms as inclusion criteria for MDD has not been changed between the DSM-IV and the DSM-5. The presence of at least five symptoms from a list of nine inclusion criteria, at least one of which should be either low mood or anhedonia, is required to fulfill the DSM-IV/DSM-5 diagnostic criteria for MDD. A total of 227 different combinations of five or more symptoms can thus fulfill the diagnostic criteria for MDD [35]. Considering real clinical situations, 170 and 119 different depressive symptom combinations have been identified in 1,566 patients with MDD diagnosed with the DSM-IV in the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) project [36] and in 853 patients with MDD diagnosed with the DSM-IV in the Clinical Research Center for Depression (CRESCEND) study [37], respectively. Moreover, either multiple or alternative compounds simultaneously define one inclusion criterion among the six MDD symptom criteria, including psychomotor agitation/retardation, impaired concentration/indecisiveness, worthlessness/guilt, insomnia/hypersomnia, decreased/increased appetite, and death wish/suicidal ideation. Thus, if each component symptom of the six complex criteria is separated, a total of 14,528 different depressive symptom combinations can fulfill the diagnostic criteria for MDD [36]. Furthermore, the heterogeneity of MDD is inconsistent with the disease essentialism paradigm that the operational criteria for mental disorders enable one to discover the essential neurobiological underpinnings of observable symptoms or signs from the perspective of the categorical approach for classifying mental disorders [11,12].
Ludwig Wittgenstein (1889–1951), a representative analytical philosopher, had a profound influence on logical positivism and language philosophy. In the context of Wittgenstein’s theory, the misconceptions that a psychiatric diagnosis indicates a particular mental process in terms of a categorical approach can be mainly criticized according to the concepts of “family resemblance” and “essence.” An analogy involving the concept of “games” has been offered previously by Wittgenstein and is as follows [38]:
Consider, for example, the proceedings that we call games. I mean board-games, card-games, ball-games, Olympic games, and so on. What is common to them all?-don’t say “there must be something common, or they would not be called games”-but look and see whether there is anything common to all. For, if you look at them, you will not see something that is common to all, but similarities, relationships, and a whole series of them at that. To repeat: don’t think, but look! … the concept game is a concept with blurred edges. “But, is a blurred concept a concept at all?” Is an indistinct photograph a picture of a person at all? Is it even always an advantage to replace an indistinct picture [with] a sharp one? Isn’t the indistinct one often exactly what we need? [39].
Rosenman and Nasti [38] regarded the operational diagnostic criteria of MDD as a corresponding equivalent to Wittgenstein’s “games” analogy, based on the fact that cases of depression are related not by an “essence” but instead by extensions of meaning in terms of the heterogeneity of MDD. Namely, a single or “essential” characteristic cannot be identified from cases of MDD that are connected by a set of “family resemblances.” In addition, from the perspective of psychiatric taxonomy, the diagnostic boundaries among psychiatric categories are mainly characterized by their boundlessness.
NETWORK ANALYSIS OF MDD SYMPTOMS AND OTHER ELEMENTS
“Symptomics,” a new paradigm that describes symptombased rather than diagnosis-based analysis, has been proposed to describe more detailed clinical features (including transdiagnostic symptoms) in the field of mental disorders. Symptomics methods are used to analyze the potential causal interrelations among symptom networks and to understand psychopathology at the level of the individual, not the diagnosis [40,41]. Based on the symptomics framework, psychiatric diagnoses are considered collections of interrelated symptoms or symptom clusters; network analysis is then used to explore the map of connections and eventual dynamic influences among symptoms and other elements including risk factors, biomarkers, and treatment responses in the field of mental disorders [42-45]. Network analysis is also used to evaluate the properties of the network as a whole and to determine whether or not these properties contribute to adaptive functioning within the network [46]. Moreover, network analysis is employed to evaluate the elements that disproportionally contribute to adaptive function within the network. Because “centrality” is defined as the overall connectivity of a symptom in the network structure, central symptoms may have a greater influence on the entire network than peripheral symptoms, and these central symptoms may facilitate interrelations between symptoms within the structure [47,48].
Network analyses performed to evaluate interactions between depressive symptoms over time have reported weaker associations between depressive symptoms in subjects with depression in remission [49] and diminished connectivity among symptoms after an intervention [50]. Network analyses to evaluate interactions between depressive symptoms and other clinical elements have also revealed connections between depressive symptoms and stressful life events [51] and relationships between stress, biomarkers, and depression [52]. The most remarkable findings of such network analyses regarding concurrent symptoms in patients with MDD are as follows: first, DSM symptoms were not more central than non-DSM symptoms in a network analysis of 28 depressive symptoms in 3,463 outpatients with depression, as part of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study. In fact, the same network analysis identified energy loss (DSM vegetative symptom), sad mood (DSM emotional symptom), and sympathetic arousal (non-DSM symptom) as the most central symptoms of MDD [47]. These findings are consistent with the observation that the most central symptoms in individuals experiencing chronic pain are difficulty with concentration, loss of interest, depressed mood, and fatigue [53]. These findings are also in line with the fact that different forms of depression are related not by an essential mental process but instead by a set of “family resemblances,” which denotes extensions of meaning in terms of Wittgenstein’s “games” analogy [38]. However, they support neither the operational definition that depressive symptoms are equivalent to indicators of MDD nor the categorical approach assumption that DSM symptoms have greater clinical relevance than non-DSM symptoms in terms of defining MDD. The findings do support the notions that depressive syndrome rather than depressive disease may be the more appropriate therapeutic target, and that symptom-based rather than diagnosis-based antidepressant selection may be a more suitable pharmacological treatment strategy.
ISSUES IN THE CLASSIFICATION OF PSYCHOTIC DEPRESSION
Psychotic depression is defined as depression accompanied by psychotic symptoms such as delusions and hallucinations [11,12,54]. Beyond the mere psychotic symptoms, psychotic depression is clinically discriminated from nonpsychotic depression in terms of a greater severity of depressive episodes; greater level of psychomotor disturbance; higher rates of rumination and insomnia; greater deficits in cognitive performance; longer duration of each subsequent episode; greater vulnerability of conversion to bipolar disorder; greater risk of psychosis in recurrent episodes; and greater rates of mortality, suicide, suicidal attempts, and suicidal ideation [55-61]. Further, psychotic depression is neurobiologically differentiated from nonpsychotic depression by way of the observation of increased activity of the hypothalamic-pituitary-adrenal axis, a greater rate of cortisol nonsuppression according to the dexamethasone suppression test, smaller volumes of the higher associative regions of the frontal and insular cortices, and a lower activity rate of dopamine-β-hydoxylase [62-70]. Therapeutic benefits in patients with psychotic depression have been observed after competitively antagonizing cortisol at the glucocorticoid receptor with mifepristone [71]. It has thus been suggested that psychotic depression may be a clinically distinctive entity rather than a subtype of MDD. However, psychotic depression is still listed as a subtype of depressive disorders (dysthymia and MDD), using the specifier “with psychotic features,” in the DSM-5 [11,12,54].
Because psychotic depression has previously been conceptualized in terms of the “severity-of-psychosis hypothesis” that considers psychotic symptoms to be dependent on the severity of the depressive episode, “with psychotic features” is allowed to be coded only for severe MDEs in the DSM-IV [72-74]. In terms of deconstructing the Kraepelinian dualism, the white paper for the DSM-5 declares that psychotic symptoms can co-occur regardless of the severity of the depressive episode [75]; as Figure 1 indicates, “with psychotic features” should be more adequately defined, and unipolar and bipolar psychotic depression are clinically related and overlap. Also, the “severity-of-psychosis hypothesis” has been rejected by several studies. The specifier “with psychotic features” can thus be coded for dysthymia and mild and moderate MDEs as well as for severe MDEs in the DSM-5 [11,12,54].
To evaluate the depressive and/or psychotic symptom domains of psychotic depression, 14 non-self-rated and symptom-based scales have been used. The review by Østergaard et al. [76] classified the 14 symptom-based scales for psychotic depression into four subgroups, including the scales predominantly covering depressive symptoms [i.e., the 17-item Hamilton Depression Rating Scale (HAMD-17), 21-item Hamilton Depression Rating Scale (HAMD-21), 24-item Hamilton Depression Rating Scale (HAMD-24), Modified Hamilton Depression Rating Scale (MHRSD), Montgomery-Asberg Depression Rating Scale (MADRS), Bech-Rafaelsen Melancholia Scale (MES), and Calgary Depression Rating Scale (CDS)]; those predominantly covering psychotic symptoms [i.e., the Brief Psychiatric Rating Scale (BPRS)], Spiker Psychoticism Scale (SPS), and Positive and Negative Symptom Scale (PANSS); those predominantly covering delusions [i.e., the Delusion Severity Item of the Schedule for Affective Disorders and Schizophrenia (SADS), Dimensions of Delusion Experience Rating Scale (DDRES), and Delusion Assessment Scale (DAS)]; and those covering both depressive and psychotic symptoms [i.e., the Psychotic Depression Assessment Scale (PDAS)].
Among all of these, the PDAS is the only validated scale to evaluate the holistic aspects of psychotic depression. The PDAS consists of 11 items derived from six items of the HAMD-17 (somatic symptoms including general, work and activities, depressed mood, psychic anxiety, guilt feeling, and psychomotor retardation) and five items of the BPRS (emotional withdrawal, suspiciousness, hallucinations, unusual thought content, and blunted affect). The scores on the BPRS items must be converted using the formula (BPRS-1)×2/3 because the scores on the HAMD-17 range from zero to four points and the scores on the BPRS range from one to seven points. Using data from a 12-week randomized controlled trial of olanzapine+sertraline (n=129) and olanzapine+placebo (n=130), the relative superiority of the PDAS over both the HAMD-6 and HAMD-17 has been demonstrated in terms of the detection of differences in pharmacological treatment responses to psychotic depression. Moreover, the PDAS has been proposed as a useful tool to differentiate psychotic from nonpsychotic depression. Most of all, in an analysis of the data from the CRESCEND study, the BPRS subscale of the PDAS showed an effective screening ability to discriminate psychotic from nonpsychotic depression, with a cutoff score of one point (sensitivity=71.2%; specificity=87.2%) [76-84]. The PDAS is thus the only useful validated scale to measure the overall aspects of psychotic depression and discriminate psychotic from nonpsychotic depression, even though it does not cover cognitive symptoms, formal thought disorders, or suicidal risk. Moreover, a more detailed version with an anchoring score from zero to four points for the PDAS has been developed, with the original English-language version now translated into Korean, Danish, Dutch, Japanese, and Turkish (http://psychoticdepressionassessmentscale.com). The PDAS can thus be considered a promising scale, in terms of considering categorical versus dimensional approaches, to supplement the definition of psychotic depression in the DSM-5.
ISSUES IN THE DIAGNOSES OF DEPRESSION AND GENERALIZED ANXIETY DISORDER
Diagnosing depression and generalized anxiety disorder (GAD) has been considered one of the most important issues regarding categorical versus dimensional approaches [11,12,54] and one of the most important matters for the DSM-5 task force to handle while refining their research agenda [85]. A closer relationship between GAD with depressive disorders than with other anxiety disorders including panic disorder, agoraphobia, social phobia, and specific phobia has been reported in several studies. Because of a close link between GAD and MDD at the genetic level, it has been proposed that GAD should be classified under the umbrella of depressive disorders, within a continuum from depression to anxiety disorders, rather than on the basis of a dichotomous distinction between depression and anxiety disorders. However, while associated symptom criterion changes for GAD have been proposed, the symptom descriptors for GAD have not changed between the DSM-IV and the DSM-5 [86,87]. Transdiagnostic specifiers and dimensional assessment tools may thus represent alternative methods to overcome the restrictions of the categorical approach in the DSM-5 diagnostic classification for depression anxiety disorders. It has been proposed that the overlaps in familial/genetic factors, childhood environment, personality traits, and demographic characteristics between MDD and GAD have contributed to the introduction of the specifier “with anxious distress.” As shown in Figure 1, “with anxious distress” is used to describe the presence of at least two among five anxiety symptoms (i.e., feeling keyed up or tense, feeling unusually restless, difficulty concentrating due to worry, fear that something awful will happen, and fear of losing control of oneself) in an MDD patient. The severity of “with anxious distress” is dimensionally graded as mild, moderate, and severe, comparable with the presence of two, three, and four or more of the five anxiety symptoms, respectively. Individuals with MDD “with anxious distress” have been characterized by poorer clinical outcomes than those without anxious distress in a large cohort study [88].
Moreover, while mixed anxiety and depressive disorder, which denote the presence of subthreshold anxiety and subthreshold depression in the ICD-10, were intended for inclusion in the DSM-5, they were ultimately not included, leading to claims that the dimensional characteristics of the relationship between anxiety disorder and depression have been insufficiently conceptualized in the DSM-5.
CONCLUSION
It has been suggested that the changes made in diagnostic classifications and criteria for depressive disorders between the DSM-IV and the DSM-5 can be nosologically conceptualized by a combination of categorical and dimensional approaches. Most of all, the dichotomization of mood disorders into bipolar disorders and depressive disorders and the replacement of “mixed episode” with “mixed features” has mainly been influenced by the deconstruction of the Kraepelinian dualism. Also, the addition of “hopelessness” to the subjective descriptors of depressive mood and the removal of “bereavement exclusion” from the diagnosis of MDD in the DSM-5 can contribute to a lowering of the diagnostic threshold for MDD, from the perspective of a dimensional approach. The complexity of the diagnostic criteria for MDD in the DSM-5 inevitably results an increase in the heterogeneity of MDD, corresponding to the Wittgensteinian “games” analogy, which suggested that the different forms of MDD are not related by a single essential characteristic but instead by “family resemblance,” thereby denoting an extension of meanings. Network analyses of MDD symptoms and other clinical elements are needed to further investigate psychopathologies in the context of computational psychiatry. Network analysis findings so far suggest that depressive symptoms are not equivalent to indicators of MDD and that DSM symptoms do not have a greater level of clinical relevance than non-DSM symptoms for the definition of MDD, respectively. In terms of diagnostic issues in psychotic and anxious depression, the transdiagnostic specifiers “with psychotic features” and “with anxious distress” may be alternative or supplementary dimensional methods for overcoming the “boundlessness” caused by the rough categorical classifications for depressive disorders including MDD. Moreover, transdiagnostic dimensional scales including the PDAS may improve measurements of the holistic features of psychotic depression listed in the current nosological definition of the DSM-5.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (2019R1A2C1090146).
Notes
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Yong-Ku Kim. Funding acquisition: Seon-Cheol Park. Investigation: Seon-Cheol Park, Yong-Ku Kim. Projected administration: Yong-Ku Kim. Writing—original draf: Seon-Cheol Park, Yong-Ku Kim. Writing—review & editing: Seon-Cheol Park, Yong-Ku Kim.