Defining Treatment Response, Remission, Relapse, and Recovery in First-Episode Psychosis: A Survey among Korean Experts
Article information
Abstract
Objective
For the proper treatment of first-episode psychosis, assessment of treatment response, remission, relapse, and recovery is important. Therefore, the present study aimed to develop operational definitions of clinical outcomes in first-episode psychosis.
Methods
A questionnaire was developed by a panel of experts and underwent three revisions. The final survey was presented to 150 psychiatrists who were members of the Korean Society for Schizophrenia Research. Respondents selected factors that they believed were important to consider while defining treatment response, remission, relapse, and recovery using a 6-point Likert scale. Selected factors that constituted each definition were statistically extracted, and operational definitions were developed.
Results
A total of 91 experts responded to the survey. The extent of reduction in psychopathology, socio-occupational functioning, and duration of each state were the core factors of each definition. Outcomes obtained from discussions and consultations by experts have been summarized and proposed.
Conclusion
The criteria developed in this survey tended to be somewhat stricter than those used by other studies. The fundamental reason for this is that this survey focused on first-episode psychosis. A better understanding of each definition in first-episode psychosis is necessary to improve effective treatment outcomes.
INTRODUCTION
The goals in treating first-episode psychosis (FEP) include targeting symptoms, preventing relapse, and increasing adaptive functioning so that the patient can be integrated back into the community as a normally functioning individual [1]. It is important to accurately determine the state of the patient during treatment in order to formulate future treatment strategies [2]. Although several studies have attempted to derive definitions of the numerous treatment outcomes, objective and clear definitions of treatment response, remission, relapse, and recovery in the treatment of FEP have yet to be established [3-5]. This ambiguity hampers comparisons between study results and has a negative impact on future treatment planning.
In general, researchers use rating scales such as the Positive and Negative Syndrome Scale (PANSS) [6], Brief Psychiatric Rating Scale [7], Scale for the Assessment of Negative Symptoms (SANS) [8], and Clinical Global Impression (CGI) scale [9] to judge treatment response, and the criteria for determining the treatment response vary from 20% to 50% of reduction [10,11]. Moreover, the period after treatment to evaluate the treatment response is another issue that should be considered. It may be meaningful to only consider the period of active treatment to avoid unnecessary delay; however, the full therapeutic effect may not manifest during this time [12-16]. If the patient responds to treatment, the patient should be reminded that symptomatic improvement lasts for a certain period of time but during remission, a patient may still have symptoms, irrespective of the magnitude of improvement [17]. The definition of remission also varies [18-22]. There has been increased focus on treatment outcome for schizophrenia; the Remission in Schizophrenia Working Group (RSWG) developed a consensus definition of symptomatic remission in schizophrenia [23]. This innovative approach for standardizing the definition of outcome in schizophrenia could facilitate research and support a positive, longer- term approach of studying the outcome in patients with schizophrenia [4]. Although symptomatic improvement is maintained after treatment, worsening of psychotic symptoms could be observed in clinical practice. It is important to determine whether it constitutes a relapse to plan the next appropriate treatment step for the patient. When defined as relapse, the patient’s symptoms may be considered on the premise that they have improved over a period. Therefore, relapse should be evaluated qualitatively and quantitatively. The core characteristics of relapse are identified as follows: the reappearance of schizophrenia symptoms in patients who have been symptom-free after an initial episode (there is need to consider a minimum period of time for reappearance of schizophrenia symptoms), worsening of clinical status severity, worsening of functioning, and reappearance of positive symptoms [5]. Recovery, the ultimate goal of treatment, should include functional recovery as well as symptomatic improvement. Recovery is defined as adequate function and not impeded social and occupational function social and occupational function, but no clear consensus on the definition of recovery exists either [24].
This lack of uniformity in the definitions of clinical outcomes has had an impact on the clinical guidelines that seek to distill evidence from various studies. Not surprisingly, given the variation used in the criteria among studies, treatment guidelines use vague definitions that are open to a wide range of interpretations, potentially leading to inconsistent clinical management and treatment delays. Complicating this, inconsistent results have been reported with the application of the same definition. For example, the reported rates of remission in FEP range between 17% and 78% [4,25]. Furthermore, the rate of recovery ranges from 13.5% to 42% [4]. These inconsistencies can confuse clinicians in the field and make it impossible to comprehensively compare results among studies [26]. In view of this, the Committee of Treatment Guidelines for First-Episode Psychosis in Korea was formed to establish consensus criteria to standardize the definition of treatment response, remission, relapse, and recovery. By comparing the status of individuals with FEP on the basis of each definition, it would be possible to determine which treatment is more effective, such that it can be used for more efficient evaluation in clinical practice and new research. The aim of the study, therefore, was to develop criteria to aid in clinical trials and clinical practice.
METHODS
Literature review
An intensive approach was adopted to develop criteria for the definitions of treatment response, remission, relapse, and recovery in FEP. First, we performed a literature review of these definitions. We searched articles and abstracts using the following keywords: first-episode psychosis, treatment response, remission, relapse, recovery, and outcome in PubMed from January 1980 to January 2016. We included studies that involved patients with first-episode schizophrenia spectrum psychotic disorder, namely schizophrenia, schizophreniform disorder, nonaffective psychosis, delusional disorder, and psychotic disorder not otherwise specified. Titles and abstracts were reviewed to initially determine eligibility. The reference lists of relevant original research and review articles were also searched to further identify potential studies. We conducted a systematic review to judge which factors were appropriate for each definition. A total of 93 studies were identified, of which 66 met the selection criteria and were used to develop a questionnaire. Operationalized criteria of treatment response [3,18,19,27-44], remission [3,18-23,27,41,42,44-58], relapse [19,21,22,27,34,39,48,53,55,57,59-73], and recovery [3,30,58,74-82] were reported in 22, 29, 26, and 14 studies, respectively.
Survey
This study was approved by the Medical Research Ethics Committee and Institutional Review Board of the Inje University Haeundae Paik Hospital (2016-06-019).
First, we recorded whether the criteria from the literature review were operationalized. Next, the key factors that constituted each definition were finely extracted. Subsequently, a committee composed of 10 expert members of the treatment guideline committee for first-episode psychosis of the Korean Society for Schizophrenia Research (KSSR) was established. The committee met four times in 2016 and mapped out the key criteria for each definition and operationalized them. Following this, the committee developed a survey, which was defined and modified three times. In its final version, it was composed of four parts with a total of 48 items, including four items for demographic data. Respondents were asked how strongly they agreed or disagreed with each statement on a 6-point Likert scale (strongly agree: 5 to strongly disagree: 0). In addition, respondents were asked to rank their preferences regarding various operational criteria. A brief introduction of the meaning and methods was provided to the respondents. Subjects were instructed to respond to questions for individuals with FEP and were informed that several commonly used instruments were included as part of the survey items. Finally, respondents were instructed that each item itself was not a definition but factors constituting a definition and which specific factors have been used by the researchers.
We recruited all KSSR members to take part in the survey to identify the key areas of agreement and disagreement. The survey was conducted via mail. One hundred and fifty members were invited via telephone and asked to participate in the survey. During the 30-day collection period, 91 responses (60.7%), covering all areas of South Korea, were received. Ten members of the KSSR refused to respond. Responses were synthesized and refined during subsequent discussions among the committee to derive a consensus recommendation. Following this, the committee met to consider and revise the criteria for which there was a lack of consensus. The revised criteria were circulated to all KSSR members and presented as part of an open workshop at a special interest meeting for further discussion, input, and refinement. Finally, consensus was reached regarding this publication through review by all authors. The results of the survey were presented and discussed at the UK-Asian Symposium on Biomarkers of Psychosis (2016) and the 2016 KSSR autumn meeting.
Measurements
PANSS is an internationally validated assessment tool based on 30 items that measure positive and negative psychotic symptoms and general psychopathology symptoms. Each item is rated based on seven categories of severity, resulting in a total score that ranges from 30 to 210 [6]. The SANS measures negative symptoms on a 25 item, 6-point scale. Items are listed under the five domains of affective blunting, alogia, avolition/apathy, anhedonia/asociality, and attention [8]. The CGI scale is an overall clinician-determined summary measure that takes into account all available information and comprises two companion one-item measures evaluating the following: (a) severity of psychopathology from a scale from 1 to 7 and (b) change from the initiation of treatment on a similar seven-point scale. Subsequent to a clinical evaluation, the CGI scale can be completed in less than a minute by an experienced rater [9].
Statistical analysis
Most of the survey consisted of assessing specific items using a 6-point (0–5) Likert scale. We scored the answers to these questions as follows: if the response was >3 points (neutral), it was determined that the item was appropriate. Responses were summarized by frequency and percentage and mean±standard deviation. Differences were tested using Fisher’s exact test for categorical data and the Mann-Whitney’s U test or Kruskal-Wallis test for numeric data. For ranked preferences, the percentage of the first ranked item was calculated. In addition, a weighted-average ranking was calculated for each answer to evaluate the most preferred answer. Statistical analysis was performed using IBM SPSS Statistics version 21.0 (IBM Corp., Armonk, NY, USA). p<0.05 was considered statistically significant. This study was exploratory by nature, and therefore no adjustment for multiple testing was applied.
RESULTS
A total of 91 experts (60.7%) participated in the survey. The mean (standard deviation [71]) age of the experts and duration of practice in psychiatry were 47.3 (9.2) and 19.6 (9.3) years, respectively. The percentage of male respondents was 79.1%. The classification of experts according to their job type was as follows: 44 (48.4%) worked at a training hospital with a psychiatry residency program; 24 (26.4%) worked at psychiatric hospital, 10 (11%) at a private clinic, eight (8.8%) at a general hospital, and five (5.5%) at another facility.
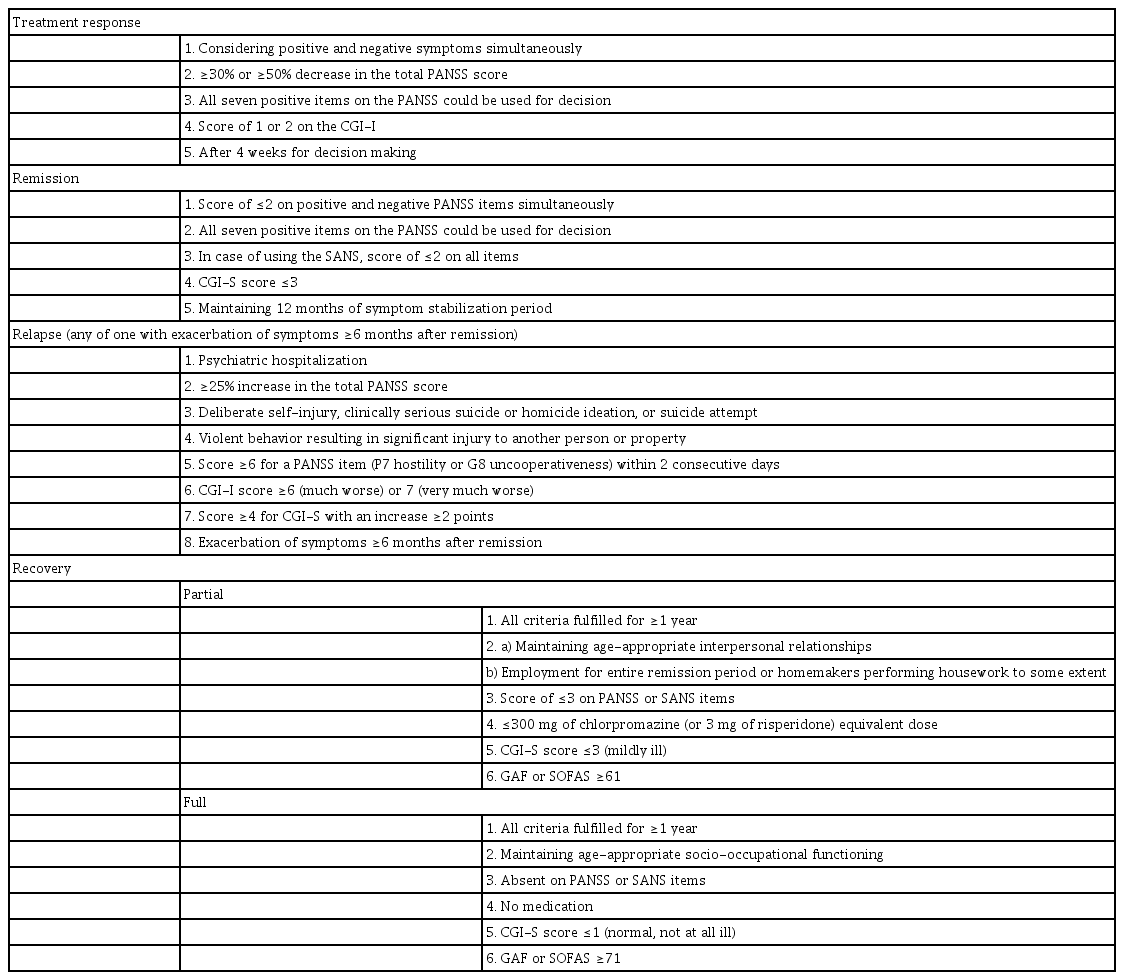
Table 1 shows the results of the consensus for defining treatment response, remission, relapse, and recovery. All results of the survey are summarized in the Supplementary Table 1–9 (in the online-only Data Supplement).
Treatment response
Instead of positive symptoms alone, simultaneously evaluating both positive and negative symptoms to judge the treatment response showed a statistically high level of consensus (p<0.001). For the PANSS total score, “30% or 50% reduction” was statistically higher than “20% reduction” (p<0.001). In the case of positive symptoms, the most appropriate criteria were surveyed, and most respondents held that all seven PANSS positive items should be evaluated. On the CGI-Improvement (CGI-I), there was no statistically significant difference between the options “improved to ≥2 points when the baseline CGI-Severity (CGI-S) score was ≥4 (moderate), and improved to ≥1 point when the baseline CGI-S score was 3” and “improved to ≥2 points” (p=0.453). When asked regarding the appropriate time to decide on a treatment response after initiation of medication, 53.3% of the respondents selected 4, followed by 6 (21.1%) and then 2 (15.6%) weeks.
Remission
The mean±SD of the consensus on the inclusion of social and occupational function to the criteria of remission was 4.08± 1.05. Most respondents answered “≤2 (minimal) than≤3 (mild)” to judge the severity of each PANSS item score for the remission criteria (p<0.001). For positive symptoms, the most appropriate criteria were surveyed and most respondents agreed that all seven PANSS positive items should be used. The use of the SANS for the evaluation of negative symptoms showed a level of agreement of approximately 3.66±1.05, and when the SANS (76) was used, the criterion of severity was “≤2 (minimal) than≤3 (mild)” to judge the severity of each SANS item score (p<0.001). The agreement level for using a CGI-S score of 3 or lower was 3.66±0.79 for symptom improvement. The most frequent response regarding the maintenance period of the remission state was 12 months (56%), followed by 6 (33.0%) and 3 (6.6%) months.
Relapse
The degree of consent on defining relapse based on the patient being admitted to the hospital due to aggravation of psychiatric symptoms was very high (4.53±0.81). The agreement on an increase of 25%≥PANSS total score showed statistically significance than the “increase of more than 20%” (p=0.001). The degree of agreement on the clinically significant suicidal attempt or suicide was 4.20±1.02 and on intentional self-injury behavior, 4.00±0.97. In the case of 2 or more consecutive days, on the Hostility or Uncooperation PANSS items, the level of consent was significantly higher for “6 points or higher” than for “5 points” (p=0.005). Moreover, the degree of consent was 4.60±0.61 when the CGI-I was 6 or 7, 4.00±0.72 when the CGI-S was 4 or higher, but 3.06±0.99 for higher levels of psychiatric treatment (increasing number of visits to the clinic) and 3.07±1.04 when there was increase of ≥25% in maintained medication dose.
In addition, when relapse was defined using the PANSS, 44.3% of the respondents selected “4 points ≥any of the four PANSS positive items (P1, P2, P3, P6) with increase ≥2 points” as their first priority. The respondents reported that the duration of the stable condition prior to relapse should be at least 6 (59.3%) or 12 (28.6%) months.
Recovery
The degree of consent on dividing recovery into partial and full was 3.94±1.22 and 3.37±0.99, respectively, for a PANSS total score ≤36 points.
For the criteria of social functioning, “having age-appropriate interpersonal relationships” (46.0%), followed by “meeting with an acquaintance more than twice a month or making phone calls” (40.2%) were selected as the definition for partial recovery. However, for full recovery, most respondents selected “having age-appropriate interpersonal relationships” (85.7%). The difference between the two definitions was statistically significant (p<0.001). For the criteria of occupational functioning, “when working or preparing for work or when the students went to school somewhat regularly and homemakers performed some housework” was highly selected at 46.5% for partial recovery and for full recovery, “having appropriate occupational or academic function and homemakers performing appropriate housework” was selected (68.5%). This difference was also statistically significant (p<0.001). The response to the question regarding the cutoff value for the general function assessment of full remission with the Global Assessment of Functioning (GAF) [83] and Social and Occupational Functioning Assessment Scale (SOFAS) [84] was (mean±SD) 76.86±7.38 and 77.23± 7.44, respectively. The cutoff value for partial recovery was 64.51±7.88 and 64.96±8.48 for the GAF and SOFAS, respectively. According to the criteria of psychiatric symptoms (using the PANSS), 77.6% of the respondents selected “3 points or lower” for partial recovery and 86.3% selected “absent” for full recovery (p<0.001). For the SANS criteria, the same pattern was revealed at 69.0% for “3 points or lower” and 72.3% for “absent” for partial and full recovery, respectively (p<0.001). For the criteria of the CGI-S, “3 points or lower” and “absent” were most preferred for partial and full recovery, respectively (p<0.001). In terms of antipsychotic dosage, “300 mg or lower of chlorpromazine equivalent” (48.8%) and “absent” (60.5%) were selected for the definition of partial and full recovery, respectively (p<0.001). Finally, 44.3% and 21.6% of the respondents answered that the period for maintenance of the recovery state should be 1 year and 2 years for partial and full recovery, respectively.
DISCUSSION
Every decision in clinical practice and clinical trials for the treatment of FEP should consider the outcomes. Because there is no clear definition of clinical outcomes in FEP, we sought to determine them and describe the subjective opinions of experts as objectively as possible.
Our results showed that besides our generally moderate rigor of development, the results of this survey might be difficult to apply simply and had a low legitimization base for clear use in clinical practice and research. The respondents’ opinions regarding factors that could be used to build definitions showed that, in practice, it may be challenging to develop operational definitions. However, the originality of our study lies in determining factors that could construct each definition based on literature review and the interpretation of responses from a nationwide survey of key representatives in Korea.
Treatment response
Treatment response denotes the extent to which a patient improves, irrespectively of the presence or absence of symptoms [17]. Most respondents reported that positive and negative symptoms should be evaluated at the same time when determining the treatment response. Although an important factor in determining treatment response is the change in positive symptoms from baseline, many researchers and clinicians use the change in the PANSS total score from baseline. Most studies on treatment response confirm the degree of change in symptoms from baseline or observe changes in relative status. In case of using percentage of reduction on rating scale, some individuals showing treatment response would still be considered markedly ill [3]. Additionally, when researchers calculate percentage reduction on the PANSS scores from baseline, they must remember to first subtract the minimum scores of 30 [2]. To overcome these problems, Leucht [3] proposed instead the use of the CGI scale. The inclusion of positive and negative symptoms for considering the treatment response does not differ from the results of previous studies because the PANSS total score also includes these two symptoms [17]. There seems to be no consensus on whether 30% or 50% reduction on the PANSS total score should be used to define treatment response [3,17] Although a widely held belief is that low response cutoffs are more sensitive for detecting differences between drugs and placebo than are higher cutoffs [2], others have contested that selecting the most sensitive cutoff is not recommended because clinically meaningful cutoffs are important for clinical trials to be informative for practice [3].
According to one meta-analysis of PANSS factor structure, P2, Conceptual Disorganization, and P4, Excitement, are not included in the positive symptoms of schizophrenia [85]. In the acute state of schizophrenia, excitement and disorganization symptoms can be seen and improved by appropriate treatment. Meanwhile, over 40% of the respondents in this study selected all seven positive symptoms as appropriate for the assessment of positive symptoms. Instead of evaluating the treatment response based on change in total score, summing the score of the items may have additional explanatory power. However, evaluating a limited number of items will be advantageous in terms of length of assessment, whereas evaluating all items requires more time and effort. Approximately half the respondents (53.3%) considered 4 weeks as the best time to determine the treatment response. Treatment guidelines for patients with schizophrenia have typically suggested a requirement for a 4–8-week antipsychotic response time [12]. The lack of response to antipsychotics in weeks 1–2 when treating acutely ill patients with schizophrenia has been shown to predict a poor response with short-term trial endpoints [12-14]. However, other studies have suggested that limited early symptom improvement is not an identifier of first-episode patients who will not show improvement in the future [15,16]. When compared with using 1–2 weeks to determine treatment response, it may be that Korean experts prefer to allow more time to pass from the initial treatment to evaluate improvement. This result was also different from those of other studies, which did not consider time for treatment response.
Remission
On remission, the results of the survey were partially different from those of the RSWG. According to the results of our survey, most respondents agreed to include the concept of social occupational function in the definition of remission. Including the concept of improvement of functioning to the criteria of remission could cause confusion with the criteria of recovery. Several studies prior to the definition of the RSWG included functional improvement in the concept of remission [4], based on the notion that if symptomatic improvement is maintained for a certain period, functional improvement could also be observed [23].
Instead of a score of 3 points, respondents defined a PANSS score of ≤2 points (minimal) as the cutoff for positive and negative symptoms for remission. This suggests that the survey respondents in this study tended to apply stricter criteria. Chung et al. [42] sought to divide the remission criteria into two different groups and use stricter cutoff and negative symptom scales, which led to a low remission rate with 20% differences between groups. In addition, using the negative symptom scale may be appropriate for studies that focus on the improvement of psychosocial function as well as symptom severity, such as longterm follow-up studies. When positive symptoms were evaluated, 53.6% of respondents considered all seven items of the PANSS positive symptoms in evaluating remission. To define remission, 56% of the respondents set 12 months as the required duration for a symptomatically stable condition. Compared with the RSWG criteria (6 months), most experts tended to report that they would use a longer duration to define remission. These rigorous criteria for determining remission might be due to differences in individuals with FEP compared with the chronic patients that were considered by the RSWG. According to a long-term study, a high percentage (approximately 80%) of patients remitted within 1 year [86]. Although long time criteria could reflect the heterogenous nature and long-term course of schizophrenia, Leucht [3] suggested 3 months for defining remission out of consideration for clinical trials that need to be sufficiently long and require frequent measurements.
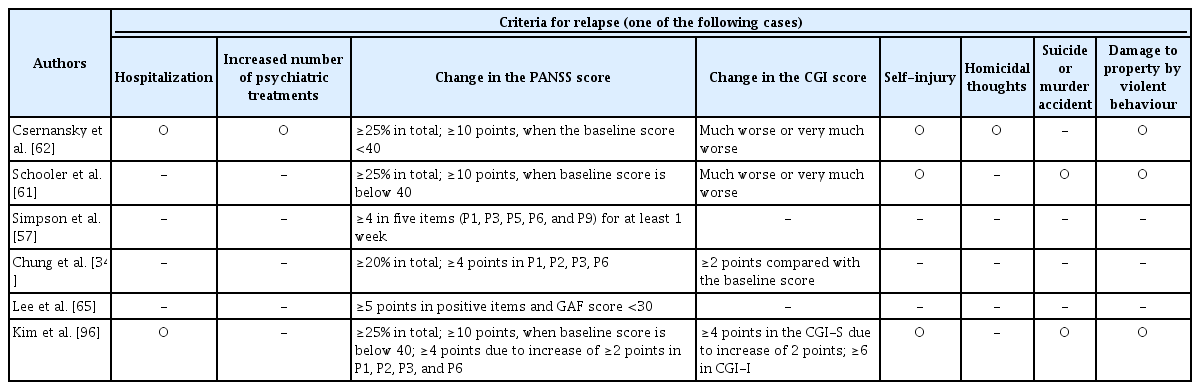
Relapse
Many relapse definitions have been used by numerous studies and are presented in Table 2. When we assessed the threshold for relapse, hospitalization due to aggravation of symptoms was considered a relapse. The aggravation of psychotic symptoms in a symptom-free patient after the initial episode being considered as a relapse is consistent with data reported in the literature [87]. In addition, the presence of positive symptoms measured by how clinical scales rate relapses agrees with data reported in the literature [19,62,87,88]. However, the definition of the minimum time necessary for the reappearance of psychiatric symptoms and worsening in disease severity and functioning was reported at 2 days in this study, whereas previous studies have reported the minimum necessary time at 2 weeks [87,89]. Conversely, we sought to define the duration of a stable condition prior to relapse, and this suggested that a period of 6 months was more favorable than a period of 12 months, which is consistent with the findings of other studies [5]. Few respondents agreed that an increase in the level (frequency) in the frequency of psychiatric consultations.
Recovery
Recovery has been operationalized as a multidimensional concept, incorporating symptomatic and functional improvement in the social, occupational, and educational domains, with a necessary duration component [4]. The numerous trials on the definitions of recovery are presented in Table 3. The results of our survey revealed that over half the respondents did not define recovery as <36 points on the PANSS. This is similar to the results of previous studies, which argued that the complete elimination of symptoms has no therapeutic purpose, and restoring social function is the ultimate goal [74,76]. We found that the GAF and SOFAS scores were consistent with data reported in the literature [75]. To identify the definitions of partial and full recovery of social function, respondents selected appropriate interpersonal relations at all age ranges, which is consistent with the findings of previous reports [74,90]. Regarding these results, it is highly likely that different interpreters will have different opinions. Although there may be the capability or desire to form interpersonal relationships, it may not be possible because of the actual environment of the patient. A total of 46.5% of the respondents agreed that the definition of partial recovery in occupational function included employment for the whole period of maintaining the remission state or homemakers performing housework to some extent. Moreover, over 25% of respondents did not specify a duration for functional recovery. Conversely, 68.5% of respondents agreed that full recovery should be defined as restored appropriate occupational or academic function or homemakers performing proper housework without a specific duration. According to generally accepted views, functional remission implies proper social functioning in the main domains of everyday life: personal care, living, working, and relating to others. However, the assessment of social functioning is quite complicated [91,92]. Many instruments have the drawback of assessing a mixture of instrumental performance of daily life tasks and psychopathology- related behavior instead of measuring the level of functioning in social roles relative to what one may expect based on social position and background [93]. Our study suggested that Korean experts agreed with a somewhat vague concept regarding socio-occupational functioning for determining recovery without specific components. This may signify that they regard the recovery state in FEP as a state of being no different than any other member of society. However, when psychopathology was considered using the PANSS, most respondents defined ≤3 points (mild) as partial recovery. Nonetheless, 86.3% of respondents defined no symptoms as full recovery.
Considering psychopathology, dosage of medication, and the CGI scale, the guidelines suggested by our Korean experts were somewhat strict compared with other definitions. This can be explained by our specificity of assessing FEP. On the duration of recovery, our results showed that it should be set at 1 year, which is consistent with the proposal by Lally et al. [4], but other study has suggested 2 years for recovery [93]. When defining recovery based on the medication dose, many Korean experts agreed that a chlorpromazine equivalent of ≤300 mg (risperidone 3 mg) and no medication indicated partial and full recovery, respectively. This medication dose was equal to those previously reported [94]. There have been suggestions that recovery should be determined not only based on symptomatic and functional remission but also based on the absence of medication [74,95]. Son et al. [94] suggested that antipsychotic treatment discontinuation in an individual who has achieved functional recovery after a single psychotic episode is associated with a high risk of symptom recurrence. Future studies should assess patients with FEP prescribed a low dosage or no medication in a medication discontinuation study.
Limitations
It is of note that a small number of experts participated in the survey. This may have excluded many opinions of experts with sufficient experience in the field of FEP. Furthermore, it is not common for the PANSS or related objective instruments to be administered in routine clinical practice in Korea. Most general and psychiatric training hospitals have a residency program for psychiatrists. Fortunately, the respondents’ working environment was biased toward general and psychiatric hospitals and were often exposed to incidents of psychosis and objective instruments for assessing the symptoms of psychosis. Although general psychometric properties cannot be examined with the CGI scale, one alternative would be to replace the PANSS with the CGI score that can be quickly and easily evaluated [3]. It should also be noted that this study identified what experts considered as intrinsic factors for each definition; however, some respondents misinterpreted the question itself as a definition. In addition, it is likely that the profile of agreed aspects of the operational definitions of treatment outcome for individuals with FEP may differ among countries; therefore, the exclusivity of the Korean-based sample is also a limitation. The decision regarding the selection of items and the formulation of questions was subjective and taken by several members of the expert panel, which may reflect the areas with highest personal experience or the clinical setting in which more studies have been performed. While experts’ opinions collected in a consensus as in this study have a low grade of evidence, we consider this study as a step in a long process to reach the level of evidence required due to the absence of other types of assessment.
In conclusion, as shown in Table 1, each criterion for the definitions of clinical outcomes was suggested using a survey. Each definition consists of the extent of the reduction in psychopathology, socio-occupational functioning, and the duration of each state.
The results of this study are outcomes obtained from various discussions and consultations after we reviewed domestic and foreign literature regarding the clinical evaluations of FEP, followed by a collection of informed opinions from Korean experts. Therefore, these results may improve the interpretation of assessment measures in FEP research. We hope that these can be widely shared among psychiatrists and play a significant role in the clinical care of patients with FEP.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2019.0240.
Acknowledgements
This research was supported by a grant of the Korean Mental Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HM14C2608) and a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI18C2383).
Notes
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Young-Chul Chung. Data curation: Kunhyung Kim, Bong Ju Lee. Formal analysis: Kunhyung Kim. Funding acquisition: Young-Chul Chung. Investigation: Young-Chul Chung, Bong Ju Lee. Methodology: Young-Chul Chung, Sung-Wan Kim, Bong Ju Lee. Project administration: Young-Chul Chung, Yang Hong Piao. Resources: Sung-Wan Kim, Jung Jin Kim, Je-Chun Yu, Kyu Young Lee, Seung-Hee Won, Seung-Hwan Lee, Seung-Hyun Kim, Shi Hyun Kang, Euitae Kim. Software: Kunhyung Kim. Supervision: Young-Chul Chung. Validation: Young-Chul Chung, Bong Ju Lee. Visualization: Kunhyung Kim, Bong Ju Lee. Writing—original draft: Bong Ju Lee. Writing—review & editing: Young-Chul Chung, Bong Ju Lee.