The Positive Aspects of Attention-Deficit/Hyperactivity Disorder among Famous People
Article information
Abstract
Objective
The shortage of clinical data regarding adult patients with often results in adults with ADHD being stigmatized and being inadequately treated. In this paper, famous people who potentially have ADHD were analyzed to understand better, the life-long progression of ADHD.
Methods
131 people were analyzed as potential candidates for ADHD. A grading system for the candidates was developed: class 1, compatible with ADHD; class 2, likely; class 3, less likely; class 4, uncertain with a shortage of data; and class 5, not compatible. Initially, 39 subjects in class 4 and 12 in class 5 were excluded from the analysis. Finally, 80 subjects (30 in class 1, 33 in class 2, and 17 in class 3) were analyzed for sociodemographic data and psychiatric comorbidities.
Results
88.8% were men and 47.5% of the subjects were married once. In terms of occupation, 45.0% of the subjects were cultural professionals and 25.0% were chief executives. Narcissistic personality disorder was the most frequently noted comorbidity, followed by substance-related and addictive disorder.
Conclusion
Famous people with ADHD in this study revealed high skill levels in occupation, offering positive aspects of ADHD in adults.
INTRODUCTION
Interest in adult ADHD has recently increased [1], and cases of late-onset ADHD in adulthood in individuals without a history of childhood ADHD have recently been reported [2]. Furthermore, there has been recent controversy surrounding the diagnosis of ADHD in children and adults [3]. The primary symptoms of ADHD differ according to ADHD subtypes, and its progress varies, which have resulted in disagreements over the diagnosis of ADHD [4]. Although ADHD is a chronic disease that requires follow-up when pediatric patients’ transition into adulthood, there is a high rate of suspension in the management of this disorder during this transition [5]. In addition, studies involving middle- and older-aged patients with ADHD are rare [6,7].
Adult patients with ADHD who were not properly treated in childhood suffered social-economic losses, such as higher rates of traffic accidents, divorce, and higher medical expenses, and also experienced personal problems such as lower educational levels, higher rates of non-professional occupations, and higher substance use disorders compared to the general population [8,9]. Contrary to these negative viewpoints of ADHD, a few scholars have argued that people with ADHD are ‘hyper-focused’ on their interests and may produce remarkable achievements or display outstanding creativity [10]. Furthermore, it has been reported that adults with ADHD may have difficulty in adapting to military life, which is representative of an organizational culture with the greatest control and restrictions [11]. However, the highly structured training in the military may provide a positive environment that promotes organizational skills among those with ADHD [12], and such findings suggest that the quality of life of adults with ADHD may differ according to the individuals’ social adaptation skills and capability [13].
A review of biographical analyses of patients with ADHD can be performed to resolve the controversy over the diagnosis and progression of ADHD. This approach is advantageous because it allows for observations of a person over the course of their life span from birth to death. Teive et al. [14] reviewed the biographies of Che Guevara, and stated that Che Guevara’s achievements were found to be in accord with ADHD. Aanonsen [15] reported that Henrik Wergeland, who worked to provide people with general education in Norway in the 19th century, had characteristics of ADHD. Fitzgerald [16] suggested the possibility that various famous figures might have ADHD based on their biographies. In addition, he identified positive aspects and strengths of ADHD through the character analyses of these individuals. The advantages of research analyses of historical figures in ADHD-related studies are as follows [17]. First, historical figure-related information are accessible through the media or from autobiographies, instead of medical records or other private personal information. Secondly, given their influence on the public, the review of whether a famous person had ADHD can have positive effects on changing the public perception of ADHD. In other words, since famous people in general had extraordinary achievements or achieved successes, they can contribute to overcoming social prejudice against ADHD.
In this study, historical figures and celebrities from the viewpoint of their potential diagnosis of ADHD were analyzed. This was an effort to communicate more effectively with the general population regarding ADHD and discover diagnostic and prognostic clues through the investigation of life-long histories.
METHODS
Subjects
The candidates for ADHD were selected from individuals who publicly claimed to have ADHD in ADHD-related websites and in the media, or individuals who self-proclaimed to have ADHD in his or her biography. The following keywords were selected for the search on Google: attention deficit hyperactivity disorder, ADHD, attention deficit disorder, ADD, historical person, celebrity, famous person, and adult ADHD. People of interest to the author were also included in this study. An analysis was then performed on the data accumulated from March 2011 through February 2017. In total, 131 initial subjects were selected for this study.
Methods
Two groups of medical students (third-year medical school students, 4 students per group) participated in a clerkship program conducted every four weeks at the Department of Psychiatry at Kyung Hee University Hospital. As a component of the clerkship program, the students selected and reviewed one candidate with potential ADHD per group. The students were educated to investigate the anecdotes compatible with ADHD and comorbid psychopathology from the autobiographies and related materials of each candidate with possible ADHD. Students presented their results during their 4th week in the clerkship program. Only data published in English or with English abstract were used. This process was supervised by two board-certified psychiatrists (Bahn GH and child fellows).
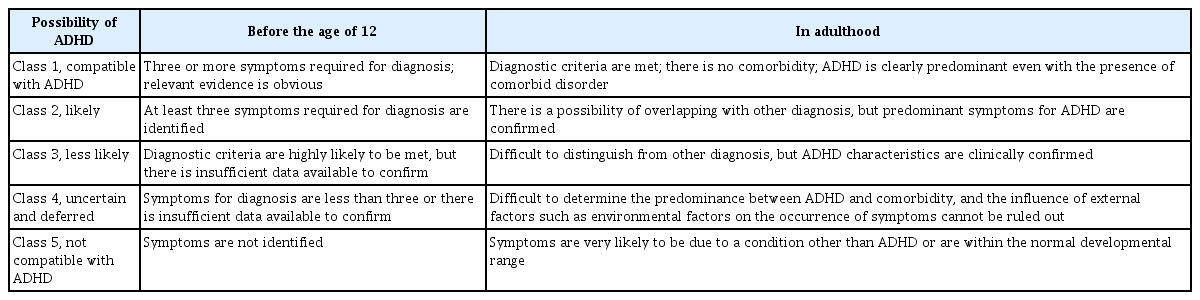
In order to evaluate the possibility that candidates may be diagnosed with ADHD, the authors developed a standard (Table 1) based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [18]. The candidates were classified according to the following assessment criteria: (A) evidence and degree of symptoms (3 or more symptoms per symptom category) prior to the age of 12, and (B) evidence and degree of symptoms in adulthood (5 or more symptoms per symptom category) as stated in the DSM-5 Diagnostic Criteria for ADHD [18]. There were five classes: Class 1, compatible with ADHD; Class 2, likely compatible with ADHD; Class 3, less likely compatible with ADHD; Class 4, uncertain and deferred; Class 5, not compatible with ADHD.
After assessing the possibility that each candidate might be diagnosed with ADHD, cases in Classes 4 and 5 were excluded from the final analysis of this study due to an uncertainty of whether they could be diagnosed with ADHD. Finally, sociodemographic data (sex, marital status, and occupation) and comorbid psychiatric disorders were analyzed for the cases in Classes 1, 2, and 3. Lifespan was presented as a century instead of life years considering privacy.
Marital status and the number of marriages were included only if they were legally recognized, even though the subjects’ cohabiting partner or extramarital affair partner was indicated in the relevant documents.
Occupations were named and classified according to the International Standard Classification of Occupations (ISCO-08) by the International Labour Organization [19]. A representative occupation of each subject was determined after discussion among the researchers. For example, one person has been described as an architect, painter, sculptor, and philosopher, but he was finally classified as a visual artist (ISCO-08 code 2651) in this study. Another people among subjects was known as an art collector, but that occupation code is not available in the ISCO-08; therefore, the subject was classified as a ‘managing director and chief executive’ (code 1120). While two subjects were great inventors, there was no occupation code for an inventor in the ISCO-08; therefore, we coded them as ‘2151, electrotechnology engineers.’ There was a professional internet gamer; however, an appropriate job code was not available in the ISCO-08, and thus the subject was classified as ‘3421, athletes and sports players.’
After each subject’s information about their comorbid psychopathology was reviewed by students and two psychiatrists, his/her comorbid psychiatric disorders were determined in accordance with the DSM-5 diagnostic criteria [18]. Each subject was allowed more than one psychiatric diagnosis.
Ethics statement
This study was approved by the Institutional Review Board of Kyung Hee University Hospital (KHUH 2019-10-058). Not all subjects have public records of being identified as ADHD or identifying themselves as ADHD. Informed consent was not obtained from these individuals. As “it is unethical for a psychiatrist to offer a professional opinion unless she/he was conducted an examination and has been granted proper authorization for such a statement [20],” the authors decided not to publish most sociodemographic information of subjects, including the lists of each subject’s biography, and also the list of subjects in the paper.
Statistical analyses
Due to the wide range of life history of the subjects, accurate statistical comparisons between classes or between individuals were not feasible. Therefore, only simple aggregates were implemented.
RESULTS
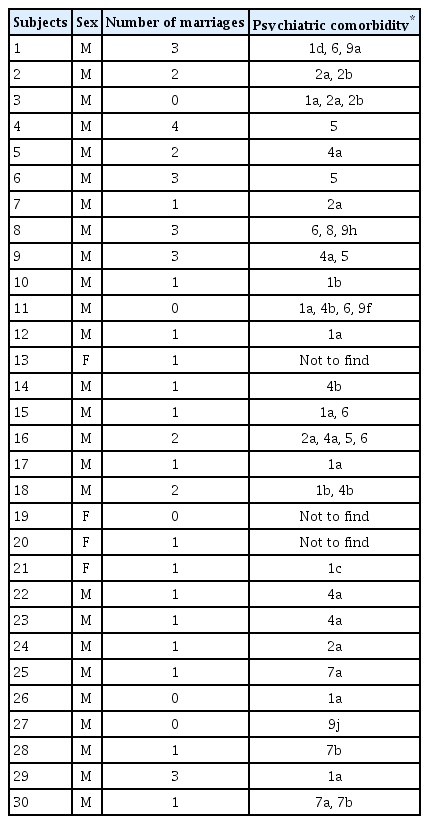
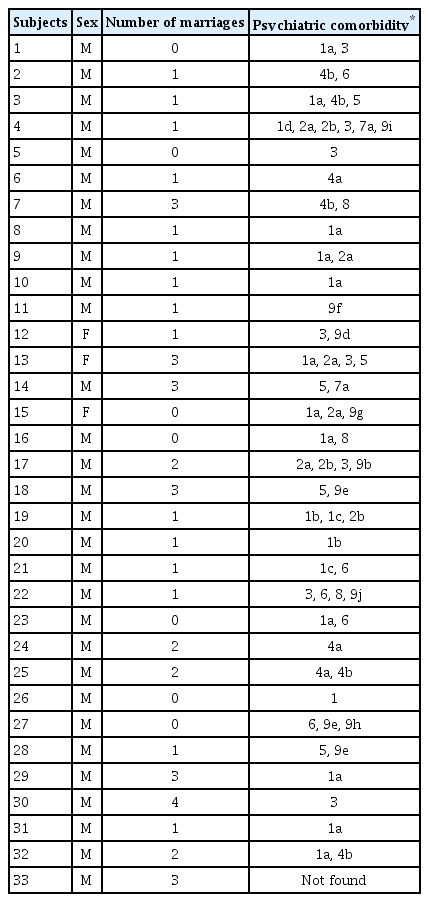
Of the 131 subjects initially reviewed, there were 39 and 12 cases in Classes 4 and 5, respectively, who were excluded from the final analysis. Ultimately, 80 subjects were analyzed in this study: 30 (37.5%) Class 1 cases (Table 2), 33 (41.2%) Class 2 cases (Table 3), and 17 (21.3%) Class 3 cases (Table 4).

Demographics, clinical characteristics and resources for the candidates categorized as Class 3 (N=17)
Of the 80 subjects, 71 (88.8%) were male. In terms of marital status, 14 (17.5%) were unmarried. In terms of the number of marriages among married subjects, 38 (47.5%) married once, 10 (12.5%) remarried, 15 (18.7%) married three times, and 3 (3.8%) married four times.
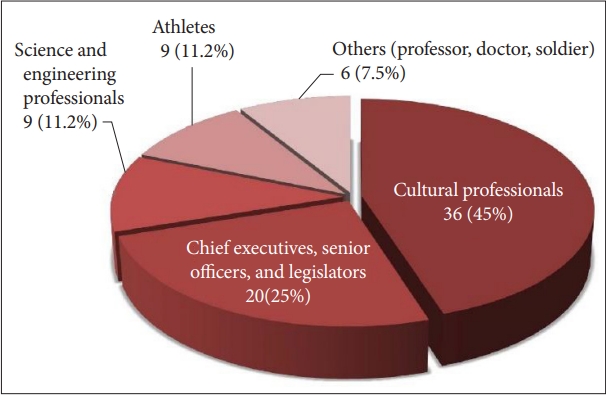
In terms of occupational classification (Table 5), the number of those in the occupational group of legal, social and cultural professionals represented the largest proportion of the subjects at 36 (45.0%) (Figure 1). The number of those in the group of chief executives, senior officials, and legislators was 20 (25.0%). The number of those in the group of science and engineering professionals was 9 (11.2%). The legal, social, cultural and related associate professionals were 9 (11.2%). There were two health professionals, three teaching professionals, and one armed forces-other ranks.
There were 133 diagnoses of comorbid psychiatric disorders with 1.66 per subject (Figure 2). Of 80 subjects, 4 were assessed as having no comorbidity. The number of those with personality disorder (PD) was the highest with 34 (25.5%). The subtypes of PD included narcissistic (25, 18.8%), obsessive-compulsive (5, 3.8%), histrionic (2, 1.5%), and antisocial (2, 1.5%). Narcissistic PD was the most frequent diagnosis even among all psychiatric comorbidities. PDs were followed by substance-related and addictive disorder (21, 15.8%), bipolar disorder (13, 9.7%), specific learning disorder (13, 9.7%), depressive disorder (12, 9.0%), obsessive compulsive disorder (12, 9.0%), disruptive disorder (7, 5.2%), and autism spectrum disorder (7, 5.2%). Since the data used in this study were not in medical records, learning disorders or dyslexia as described in autobiographies or related data were included in specific learning disorder categories. Disruptive disorders included conduct disorders and oppositional defiant disorders. When classifying the results of this study, Asperger syndrome, pervasive developmental disorder, and infant autism as described in related data were included in autism spectrum disorder if they were considered appropriate. In addition, ‘others’ included tic disorder, posttraumatic stress disorder, pedophilia, specific phobia, body dysmorphic disorder, generalized anxiety disorder, somatic symptom disorder, and nocturnal enuresis in childhood.
DISCUSSION
In this study, the diversity and whether the candidates had ADHD in adulthood were identified through a lifelong trajectory analysis of various famous people. While the subjects show evidence of ADHD, the majority of the subjects were engaged in highly skilled professional occupations.
While sex differences in ADHD become less prominent in adults as compared to children [21], 88.8% of the subjects in this study were male. This was due to more men being identifiable in records, especially in the past centuries, rather than famous men with ADHD being more common among famous people with ADHD. Therefore, it was presumed that this result might be influenced by a selection bias.
In the USA, the divorce rate among the general population continued to rise between 1960 and 1980 [22], with 50% of marriages expected to end in divorce. Adults with ADHD are known to be more likely than the general population to have difficulties in marital relationships resulting in higher rates of divorce [9]. Of the candidates with ADHD in this study, 47.5% married once, and approximately 1/3 married twice or more times. These results suggested that the subjects of this study had more stable relationships in marriages than couples with ADHD in previous studies. However, because the subjects of this study were very different with respect to social, cultural, and historical backgrounds, it was difficult to conclude whether their marriage and remarriage characteristics represent the married life of adults with ADHD.
Of the 80 subjects in this study, the occupations of all subjects correspond to ISCO-08 Skill Levels 3 and 4. Occupations at Skill Level 3 typically involve the performance of complex technical and practical tasks that require an extensive body of factual, technical, and procedural knowledge in a specialized field [19]. Skill Level 4 typically involves the performance of tasks that require complex problem-solving, decisions-making, and creativity based on an extensive body of theoretical and factual knowledge in a specialized field [19]. None of the subjects in this study had final occupations at Skill Level 1 or 2. These results were different from those of previous studies that emphasized the impairments in major life activities, especially unemployment and problems in work performance in adults with ADHD [9]. These differences support the hypothesis that adults with ADHD might have jobs with higher skills according to personal characteristics, such as a higher level of intelligence and less psychiatric comorbidities [13]. It is interesting to note that 45% of the subjects of this study were people in the cultural professionals who required creativity, such as writers, painters, musicians, actors, and film directors. Davis [23] described the following attributes of creative people: risk taking, energetic, attracted by complexity, artistic, open-minded, and emotional. Many of these factors match the characteristics of patients with ADHD [10]. The results of this study can present positive evidence of whether patients with ADHD may be more creative than the general public [24]. Fitzgerald [16] claimed through the trajectory analysis of many artists that they may have ADHD. However, it is difficult to say whether there are more artists among people with ADHD. While children with ADHD may be more creative in some evaluated areas compared to typical developing children [25], there have been no follow-up reports of creative children with ADHD through adulthood. For parents, in addition, the effects of stimulants on creativity can affect the decision of medication for children with ADHD. Recent studies have reported better creative potential in children with ADHD with un-medicated condition than medicated [26,27]. Therefore, the results of this study could provide guidance for a more effective assessment of giftedness in youths with ADHD.
ADHD is often associated with a higher rate of psychiatric comorbidity in both children and adults than in the general population [28]. Between 65 and 89% of all adults with ADHD suffer from one or more psychiatric disorders during their lifespan [29]. The subjects of this study also had 1.66 comorbid psychiatric disorders per person. The most common psychiatric disorders in adulthood ADHD are anxiety disorders, mood disorders, substance use disorders and personality disorders [30]. The distribution of comorbid disorders varies according to sex. In other words, it has been reported that the prevalence of mood disorders, anxiety disorders, and eating disorders as comorbid disorders was higher in female patients with ADHD than in male adults with ADHD [31]. The prevalence of substance-related and addictive disorders as comorbid disorders was higher in male patients with ADHD than in female patients with ADHD [30]. The results of this study also found that substance-related disorders were the second most common comorbid mental disorder, probably due to the greater number of males than female subjects. Previous studies have shown that antisocial personality and borderline personality disorder were the most common comorbid disorders in adult ADHD [32]. In the results of this study, the distribution of personality disorder subtypes was found to be different from the results of previous studies. Particularly, it was noticeable that narcissistic personality disorder was found to be the most common, whereas borderline personality disorder was not found. The materials related to the subjects of this study primarily focused on personal accomplishments and social achievements, which suggest that more cases of narcissistic personality traits could be identified. The reasons for the absence of borderline personality disorder in this study are as follows: first, the number of female subjects of this study was small, with 9 subjects among 80; secondly, these female subjects were extraordinary people with remarkable personal achievements. Differences in the distribution of comorbid disorders between this study and previous studies suggest that the prognosis of adult ADHD may vary depending on individual abilities.
This study has some obvious limitations. First, since the research materials were not medical records and were described by the subjects themselves or by people around them, it was difficult to guarantee the accuracy of the assessment of comorbid psychiatric disorders or the diagnosis of ADHD in the subjects. Because most descriptions regarding the subjects of this study focused on their activities in adulthood, there was a lack of related materials on their childhood that were essential for the diagnosis of ADHD. Secondly, there was a variable for screening the subjects of this study; adults with ADHD were not randomly extracted from the general population, but rather they were selected from socially or historically famous people. Regional and cultural limitations should also be considered. Therefore, it is quite difficult to generalize the results of this study as the characteristics of ADHD in adults. Thirdly, most people in this study have remarkable achievements in certain areas. To establish incredible achievements in specific domains, they would require selective immersion with creativity unlike that observed in the normal population as well as relatively less focus on certain parts of life. Fourth, while the talents or intelligence could be matter to the subjects’ achievement, the parents (or guardian) with goodness-of-fit, friends and spouse might have an important role to their success. In later studies, exploring the effects of environmental factors, including peoples, will help establish a diagnosis and treatment strategy. In this paper, these life trajectories were classified as ADHD according to the clinical diagnostic criteria; however, new evaluation criteria to differentiate those who are particularly outstanding from ordinary people are needed in the future.
Despite these limitations, the data from this study could be useful in clinical practice when diagnosing adults with ADHD, given that the data were analyzed based on the whole life history of the candidates. If the characteristics of each ADHD subject were analyzed by life cycle and in further detail, the results may be helpful for the diagnosis and management of ADHD, as well as for identifying prognostic factors for ADHD in adults. To the best of our knowledge, this is the first report that analyzed the potential diagnosis of ADHD across the lifetime trajectory with a large sample.
Acknowledgements
The theme of this article was presented as a poster at the 6th World Congress on ADHD on 21 April, 2017, Vancouver, Canada. The author thanks Donggi Hwang for help in the data analysis. Also special thanks to the fellowship trainees in the division of child and adolescent psychiatry, Su-Jin Moon, Jung-Won Min, Yeon Jung Lee, Minha Hong, Juhee Han, Ram Hwangbo, Sung-Woo Cho, Seung Yup Lee, Kyung Hoon Seo for the discussion to diagnose cases with psychiatric disorders including ADHD from 2011. Also, I would like to thank the medical students who contributed to the accumulation of this research data during their clerkship.
Finally, I would like to thank Editage (www.editage.co.kr) for English language editing.
Notes
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Geon Ho Bahn. Data curation: Jong Won Lee. Formal analysis: Geon Ho Bahn. Investigation: Geon Ho Bahn. Methodology: Kyunghoon Seo. Project administration: Geon Ho Bahn. Resources: Jong Won Lee. Software: Geon Ho Bahn. Supervision: Geon Ho Bahn. Validation: Kyunghoon Seo. Visualization: Jong Won Lee. Writing—original draft: Jong Won Lee, Kyunghoon Seo. Writing—review & editing: Geon Ho Bahn.