Network Analysis of the Symptoms of Depressive Disorders Over the Course of Therapy: Changes in Centrality Measures
Article information
Abstract
Objective
Network analysis can be used in terms of a novel psychopathological approach for depressive syndrome. We aimed to estimate the successive network structures of depressive symptoms in patients with depressive disorder using data from the Clinical Research Center for Depression study.
Methods
We enrolled 1,152 South Korean adult patients with depressive disorders who were beginning treatment for first-onset or recurrent depressive episodes. We examined the network structure of the severities of the items on the Hamilton Depression Rating Scale (HAMD) at baseline and at weeks 2, 12, 25, and 52. The node strength centrality of all the HAMD items at baseline and at week 2, 12, 25, and 52 in terms of network analysis.
Results
In the severity networks, the anxiety (psychic) item was the most centrally situated in the initial period (baseline and week 2), while loss of weight was the most centrally situated item in the later period (weeks 25 and 52). In addition, the number of strong edges (i.e., edges representing strong correlations) increased in the late period compared to the initial period.
Conclusion
Our findings support a period-specific and symptom-focused therapeutic approach that can provide complementary information to the unidimensional total HAMD score.
INTRODUCTION
Heterogeneity is a key challenge in defining a depressive syndrome, which is defined in a polythetic and operational manner [1-4]. According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [5], the diagnostic criteria for major depressive disorder (MDD) include nine symptoms. MDD is diagnosed when patients present with five or more of these symptoms, one of which should be depressed mood or diminished interest lasting for more than two weeks. However, calculating the binomial coefficient of the combinations of symptoms meeting this criterion yields almost 227 possibilities [1,6]. Indeed, depressive sub-syndromes have been identified based on the differing numeric values of possible combinations. In the Rhode Island Methods to Improve the Diagnostic Assessment and Service (MIDAS) project, 170 different symptom combinations were identified among 1,566 patients with MDD [6]. Furthermore, in the Clinical Research Center for Depression (CRESCEND) study involving 853 patients, 119 different symptom combinations were found to meet the diagnostic criteria for MDD [7]. It is asserted that certain symptom combinations are more prevalent than others in a depressive syndrome. However, current evidence-based medicine may be insufficient to fully describe the heterogeneous complexity of depressive disorders, leading to a recommendation that the application of the DSM-5 definition is limited to a general clinical setting [8]. Moreover, according to Insel [9], clinical targets should be personalized in terms of the “nextgeneration treatments for mental disorders” based on a diagnosis to a symptom or to an endophenotype. In contrast to earlier opinions that depression is the result of a chemical imbalance, it is now proposed that depression is conceptualized as a dysfunction of the neural circuit as a whole. McNally et al. [10] proposed a new pragmatic perspective on psychopathology based on symptoms rather than categories, as follows: “Symptoms are not an outcome of an underlying disease; symptoms and the associations between them are the disease itself.” Thus, network analysis is a natural method of analyzing psychopathology, working from the bottom up, without applying any top-down construct consistent with the standard biomedical and reductionist model [11]. A network analysis attributes a given psychiatric condition to a network structure of symptom components, whereas a traditional structural equation model explains any covariance of constituent symptoms in terms of the common influence of a latent variable [12-14]. The heterogeneity of the interrelated symptoms within a network of depressive disorders can be explained better with a network-analytic approach that is consistent with nominalism and not with essentialism [15,16]. A network analysis can computationally evaluate a given property of the network structure and determine component variables that contribute proportionately or disproportionately to the network cohesiveness. In an estimated network structure, a centrality measure denotes the overall connectivity of a particular symptom. Central symptoms, or symptoms with a high value of this measure, contribute the most to the interrelatedness of symptoms within the estimated network structure [17-21]. It is suggested that central symptoms have a stronger involvement in disease than peripheral symptoms, translating into a greater impact on the cohesiveness of the symptom network. A network analysis can provide a novel perspective for evaluating the diagnostic construct “depressive disorder.” For instance, a network analysis of 3,463 outpatients with depression performed by the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study demonstrated no significant differences between the centralities of DSM symptoms (e.g., depressed mood) and those of non-DSM symptoms (e.g., anxiety) [22]. These previous findings are further supported by a network analysis considering the centralities of DSM symptoms and non-DSM symptoms in 5,952 Han Chinese women with MDD [23]. In addition, depressive symptoms were not more central than anxiety symptoms in a network analysis of symptomatology in 223 patients with major depression [24]. Guilt, in fact, was the most central domain within a network structure of depressive symptoms in 643 East Asian patients with depressive disorders. This result is not entirely consistent with the typical symptoms of depressive episodes as defined by the tenth edition of the International Statistical Classification of Diseases and Related Health Problems, namely depressed mood, loss of interest, and reduced energy [25]. Thus, using data from the CRESCEND study [7], this study aimed to estimate the serial changes in the centralities and network structures of the items of the 17-item Hamilton Depression Rating Scale (HAMD) [26,27] in a large sample of South Korean patients with DSM-defined depressive disorders.
METHODS
Study overview
The CRESCEND study in South Korea comprises a large nationwide sample of patients with depressive disorders. It is a prospective, observational, and naturalistic study, and is the first to use such a large sample of national data [7]. A total of 1,183 participants with depressive disorders, including firstonset patients beginning psychiatric treatment and those diagnosed with a recurrent depressive episode, were recruited at 18 study centers, including 16 university-affiliated hospitals and 2 general hospitals, across South Korea from January 2006 to August 2008. The inclusion criteria were as follows: 1) age >18 years; 2) a current diagnosis of MDD, dysthymic disorder, or depressive disorder not otherwise specified, as defined by the DSM-IV (American Psychiatric Association 1994) and confirmed by the Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version (SCID-I) [28]; and 3) completion of all HAMD items [26,27] at baseline and at weeks 2, 12, 25, and 52. The exclusion criteria were as follows: 1) a current or lifetime comorbid diagnosis of cognitive disorders, schizophrenia, other psychotic disorders, or bipolar disorders as defined by the DSM-IV [29]; 2) current or past history of any significant medical or neurological disease; and 3) pregnant or breastfeeding women, or women who intend to become pregnant within 9 months of enrollment. Finally, 1,152 patients with depressive disorders were included in our study. The research protocol and consent form were approved by the institutional review boards of all the study centers, including the Catholic Medical Center, Catholic University of Korea (receipt number: CUMC07U001). All eligible study subjects provided written informed consent prior to study participation.
Study design
The study participants underwent diagnostic evaluation at baseline, and histories of medical diseases and psychiatric disorders were taken. In addition, at each of the regional centers, the sociodemographic and clinical data of all participants were collected and evaluated by trained and certified research coordinators under the supervision of clinical psychiatrists. After the exclusion of patients according to the stated criteria, eligible study subjects were psychometrically assessed by a clinician at baseline and at weeks 2, 12, 25, and 52 using the HAMD.
The 17-item HAMD, a clinician-administered assessment scale, fully covered the melancholic and physical features of depression. The patients described the severity of their psychiatric symptoms using a 5-point Likert scale: 0 (symptoms absent), 1 (mild symptoms), 2 (moderate symptoms), 3 (severe symptoms), and 4 (very severe symptoms) [26]. The internal consistency (Cronbach’s α=0.76) and inter-rater reliability (r=0.94, p<0.0001) of the Korean version of the HAMD were considered favorable and excellent, respectively [27].
Statistical analysis
The network structures were estimated using the R package “graphics.” [30] Using mixed models of repeated-measures analysis of the HAMD items, we constructed network structures consisting of nodes (symptoms) and edges (associations among symptoms). False-positive edges were controlled using the least absolute shrinkage and selection operator (LASSO) [31], and very short edges were set to exactly 0 in length. The edges indicate partial correlation coefficients in the graphical LASSO procedure. Thus, the edge length inversely represents the relationship strength between two symptoms with all other relationships within the network controlled. In addition, the shrinkage parameter was minimized by the extended Bayesian information criterion, and the underlying network structures were accurately recovered [32,33]. The shorter the distance between two nodes, the stronger the associations between the two corresponding symptoms, as calculated using the Fruchterman-Reingold algorithm. This convention provides a visual demonstration of the network. Several centrality indices were examined, including node-strength centrality, a common, stable, central metric, and the sum of the associations of a given node with all others; closeness centrality, a measure of how closely one symptom is related to others; and betweenness centrality, the number of shortest paths connecting two other nodes that pass through the node under consideration. In this study, the conclusions are based on node-strength centrality, but this measure was substantially correlated with the other centralities.
The correlation stability coefficient (CS coefficient), which we calculated with 1,000 node-drop bootstrap replicates, denotes the maximum proportion of cases that can be eliminated and still retain a 95% probability of a correct node ranking. Thus, in a node-ranking correlation between the original and the case-subset networks, a CS coefficient of 0.700 would amount to a very large effect [34]. The stability of the centrality measure was operationally defined using the CS coefficient, and we only considered centrality indices with a CS coefficient above 0.250—and preferably above 0.500—as recommended by Epskamp et al. [30].
RESULTS
Baseline characteristics
Of the 1,152 patients with depressive disorders, the mean age and age at onset of the first depressive episode were 48.3 [standard deviation (SD)=2.0] years and 45.2 (SD=17.4) years, respectively. The participants were predominantly female (74.4%), married (65.9%), and not working outside the home (64.2%). In addition, many of the participants were enrolled as outpatients (78.4%) and diagnosed with recurrent depressive episodes (67.0%). Other baseline characteristics as well as psychometric assessments, including the HAMD scores at baseline and at weeks 2, 12, 25, and 52, are presented in Table 1. In the selection of an initial antidepressant, the prescription rates for SSRIs, dual-action antidepressants, and other antidepressants were 48.9%, 45.8%, and 5.3%, respectively. Among SSRIs, escitalopram (22.4%) was the most prescribed initial antidepressant, followed by paroxetine (18.7%), fluoxetine (4.1%), and sertraline (3.7%). Furthermore, 20.6% of the patients who underwent antidepressant therapy were prescribed concomitant medications.
Estimated networks of HAMD items
Baseline (n=1,152)
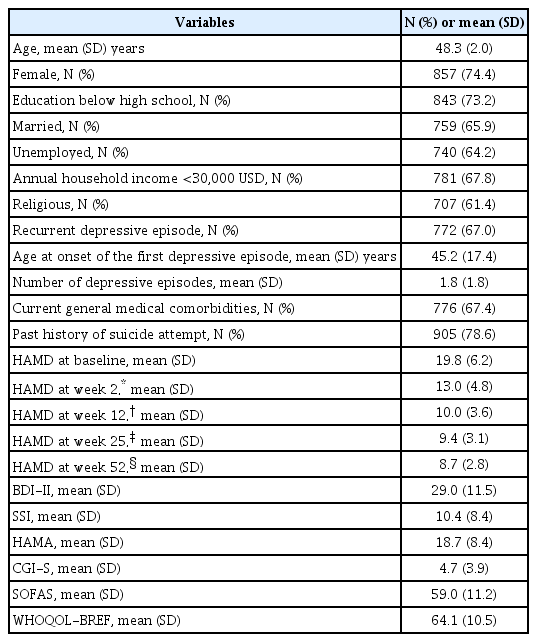
Construction of a severity network on the 17 HAMD items at baseline revealed that 85 (63.2%) of a possible 136 edges were estimated to exceed 0 (Figure 1A). In addition, several strong, positive edges with partial correlations of more than 3.000 were revealed, including connections between insomnia (middle of the night) and insomnia (early hours of the morning), insomnia (early in the night) and insomnia (middle of the night), somatic symptoms (gastrointestinal) and loss of weight, insomnia (early hours of the morning) and insomnia (early in the night), and between anxiety (psychic) and agitation. Inspecting the node strength centrality of the HAMD items revealed that anxiety (psychic) was the most central symptom domain, followed by work-and-activities, depressed mood, and others, while agitation was the most poorly interconnected within the network. At baseline, the mean total score on the HAMD was 19.8 (SD=6.2) (Table 1). The centrality indices for the node strength, closeness, and betweenness of the severity network of the 17 HAMD items at baseline are shown in Figure 1B.

Network structure and node statistics of the Hamilton Depression Rating Scale items at baseline (N=1,152). A: Network structure of the symptoms of depressive disorders at baseline (CS coefficient=0.400). Green lines represent positive associations. Red lines represent negative associations. The line thicknesses represent the edge strengths. Nodes are depressive symptoms evaluated with the Hamilton Depression Rating Scale. B: Node statistics of the symptoms of depressive disorders at baseline. AGI: agitation, ANP: anxiety psychic, ANS: anxiety somatic, DEP: depressed mood, GAS: somatic symptoms gastro-intestinal, GEN: general somatic symptoms, GUI: feelings of guilt, HYP: hypochondriasis, IEA: insomnia: early in the night, IMI: insomnia: middle of the night, IMO: insomnia: early hours of the morning, INS: insight, RET: retardation, SEX: genital (sexual) symptoms, SUI: suicide, WOR: work and activities.
Week 2 (n=801)
As shown in Figure 2A, the severity network of the HAMD items assessed at week 2 revealed that 85 (63.2%) of all possible edges were estimated to exceed 0. In addition, several strong positive edges were found between insomnia (middle of the night) and insomnia (early hours of the morning), insomnia (early in the night) and insomnia (middle of the night), somatic symptoms (gastrointestinal) and loss of weight, feelings of guilt and suicide, and between anxiety (psychic) and agitation. Thus, the strong edges at week 2 were similar to those at baseline. Inspecting the node-strength centrality of the HAMD items revealed that anxiety (psychic) was again the most centrally located within the estimated network, whereas genital symptoms was the most poorly interconnected within the network. The mean total score on the HAMD at week 2 was 13.0 (SD=4.8) (Table 1). The centrality indices at week 2 are shown in Figure 2B.
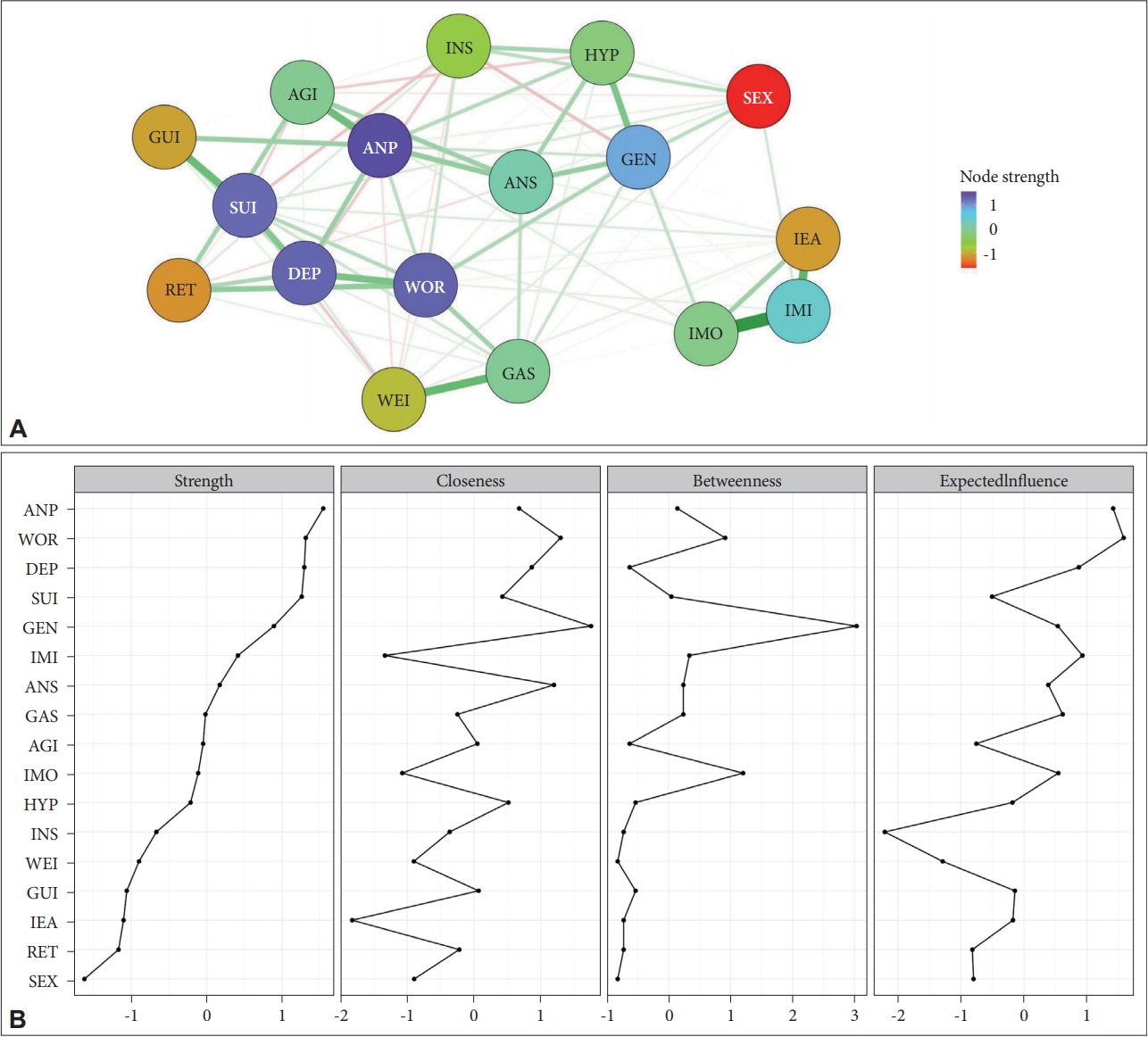
Network structure and node statistics of the Hamilton Depression Rating Scale items at week 2 (N=801). A: Network structure of the symptoms of depressive disorders at week 2 (CS coefficient=0.400). Green lines represent positive associations. Red lines represent negative associations. The line thicknesses represent the edge strengths. Nodes are depressive symptoms evaluated with the Hamilton Depression Rating Scale. B: Node statistics of the symptoms of depressive disorders at week 2. AGI: agitation, ANP: anxiety psychic, ANS: anxiety somatic, DEP: depressed mood, GAS: somatic symptoms gastro-intestinal, GEN: general somatic symptoms, GUI: feelings of guilt, HYP: hypochondriasis, IEA: insomnia: early in the night, IMI: insomnia: middle of the night, IMO: insomnia: early hours of the morning, INS: insight, RET: retardation, SEX: genital (sexual) symptoms, SUI: suicide, WOR: work and activities.
Week 12 (n=522)
As shown in Figure 3A, the severity network of the HAMD items assessed at week 12 revealed that 89 (65.4%) of all possible edges were estimated to exceed 0. In addition, several strong positive edges were revealed between insomnia (middle of the night) and insomnia (early hours of the morning), anxiety (psychic) and agitation, depressed mood and work-and-activities, and feelings of guilt and suicide. Inspection of the nodestrength centrality of the HAMD items revealed work-andactivities to be the most centrally located within the estimated network, whereas retardation was the most poorly interconnected within the network. Moreover, at week 12, the mean total HAMD score was 10.0 (SD=3.6) (Table 1). The centrality indices at week 12 are shown in Figure 3B.
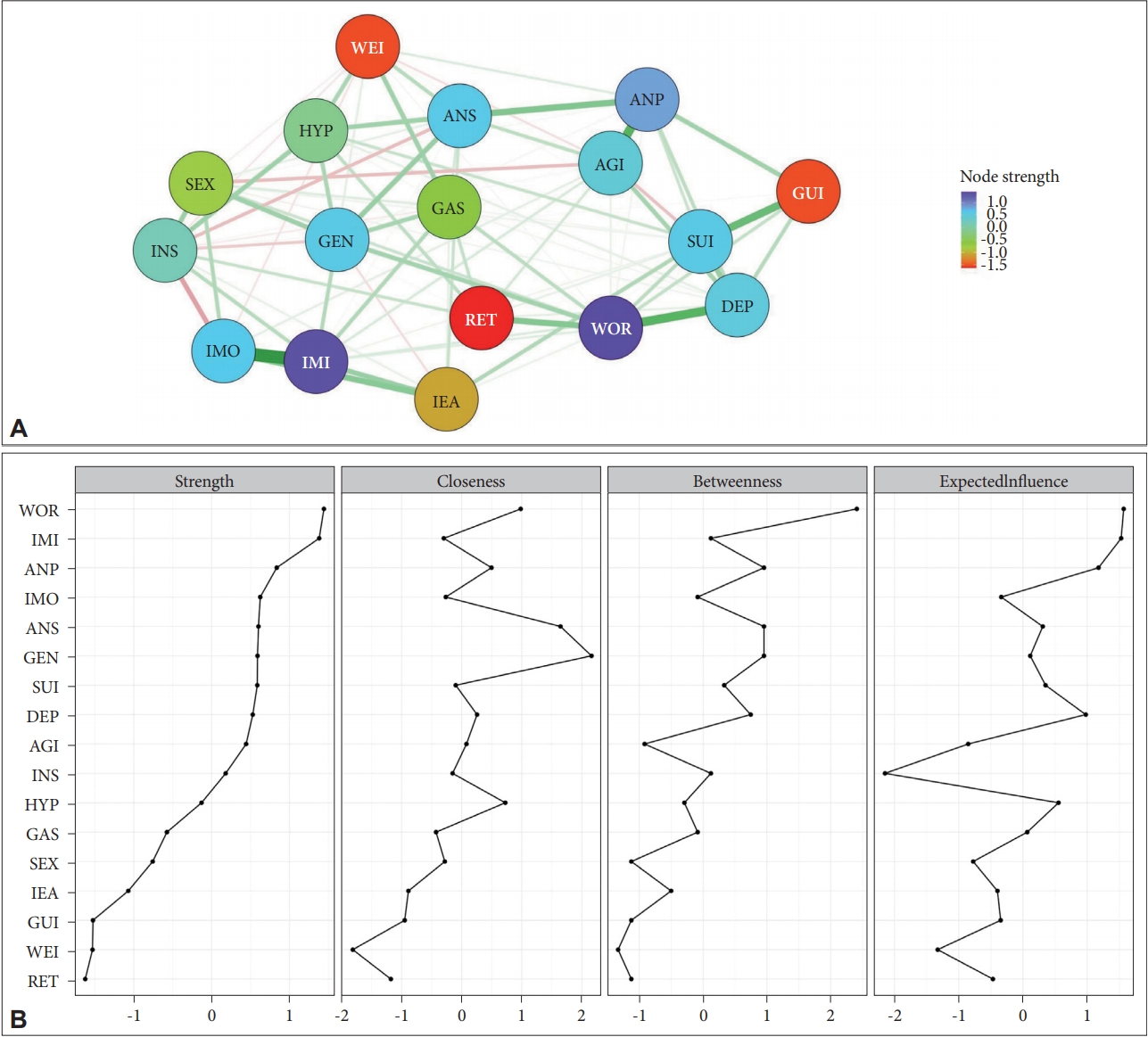
Network structure and node statistics of the Hamilton Depression Rating Scale items at week 12 (N=522). A: Network structure of the symptoms of depressive disorders at week 12 (CS coefficient=0.323). Green lines represent positive associations. Red lines represent negative associations. The line thicknesses represent the edge strengths. Nodes are depressive symptoms evaluated with the Hamilton Depression Rating Scale. B: Node statistics of the symptoms of depressive disorders at week 12. AGI: agitation, ANP: anxiety psychic, ANS: anxiety somatic, DEP: depressed mood, GAS: somatic symptoms gastro-intestinal, GEN: general somatic symptoms, GUI: feelings of guilt, HYP: hypochondriasis, IEA: insomnia: early in the night, IMI: insomnia: middle of the night, IMO: insomnia: early hours of the morning, INS: insight, RET: retardation, SEX: genital (sexual) symptoms, SUI: suicide, WOR: work and activities.
Week 25 (n=409)
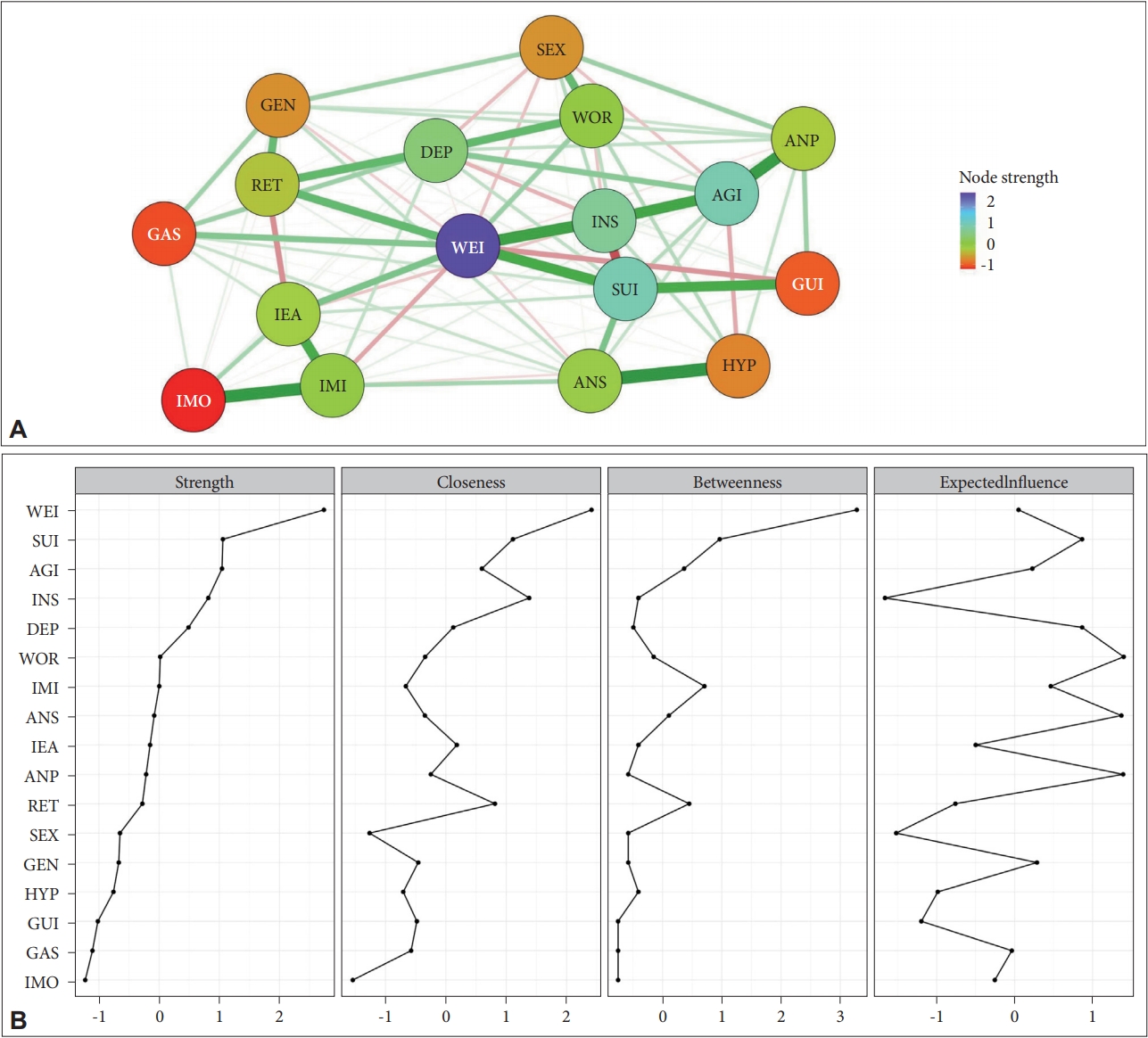
As shown in Figure 4A, the severity network of the HAMD items assessed at week 25 revealed that 120 (88.2%) of all possible edges were estimated to exceed 0. In addition, several strong edges were revealed, including those between insomnia (middle of the night) and insomnia (early hours of the morning), somatic symptoms (gastrointestinal) and loss of weight, feelings of guilt and loss of weight, anxiety (psychic) and anxiety (somatic), depressed mood and suicide, feelings of guilt and insomnia (early in the night), retardation and insight, anxiety (somatic) and loss of weight, general somatic symptoms and somatic symptoms (gastrointestinal), insomnia (early in the night) and insomnia (early hours of the morning), insomnia (early in the night) and somatic symptoms (gastrointestinal), work-and-activities and general somatic symptoms, and between agitation and somatic symptoms (gastrointestinal). Conversely, several strong negative edges with partial correlations of less than -3.000 were found between insomnia (early hours of the morning) and loss of weight, feelings of guilt and somatic symptoms (gastrointestinal), agitation and loss of weight, and feelings of guilt and anxiety (somatic). Inspecting the node-strength centrality of the HAMD items revealed loss of weight to be the most centrally located within the estimated network, while retardation was the most poorly interconnected within the network. Moreover, at week 25, the mean total score on the HAMD was 9.4 (SD=3.1) (Table 1). The centrality indices at week 25 are shown in Figure 4B.

Network structure and node statistics of the Hamilton Depression Rating Scale items at week 25 (N=409). A: Network structure of the symptoms of depressive disorders at week 25 (CS coefficient=0.399). Green lines represent positive associations. Red lines represent negative associations. The line thicknesses represent the edge strengths. Nodes are depressive symptoms evaluated with the Hamilton Depression Rating Scale. B: Node statistics of the symptoms of depressive disorders at week 25. AGI: agitation, ANP: anxiety psychic, ANS: anxiety somatic, DEP: depressed mood, GAS: somatic symptoms gastro-intestinal, GEN: general somatic symptoms, GUI: feelings of guilt, HYP: hypochondriasis, IEA: insomnia: early in the night, IMI: insomnia: middle of the night, IMO: insomnia: early hours of the morning, INS: insight, RET: retardation, SEX: genital (sexual) symptoms, SUI: suicide, WOR: work and activities.
Week 52 (n=281)
As shown in Figure 5A, the severity network of the HAMD items assessed at week 52 revealed that 90 (66.2%) of all possible edges were estimated to exceed 0. Several strong positive edges were found, including those between anxiety (somatic) and hypochondriasis, insomnia (middle of the night) and insomnia (early hours of the morning), anxiety (psychic) and agitation, loss of weight and insight, agitation and insight, suicide and loss of weight, insomnia (early hours of the morning) and insomnia (middle of the night), feelings of guilt and suicide, depressed mood and retardation, and between depressed mood and work-and-activities. Conversely, a strong negative edge was revealed between suicide and insight. Inspecting the node-strength centrality of the HAMD items again revealed loss of weight to be the most centrally located within the estimated network, whereas insomnia (early hours of the morning) was the most poorly interconnected within the network. The mean total HAMD score at week 52 was 8.7 (SD= 2.8) (Table 1). The centrality indices at week 52 are shown in Figure 5B.
Network structure and node statistics of the Hamilton Depression Rating Scale items at week 52 (N=281). A: Network structure of the symptoms of depressive disorders at week 52 (CS coefficient=0.205). Green lines represent positive associations. Red lines represent negative associations. The line thicknesses represent the edge strengths. Nodes are depressive symptoms evaluated with the Hamilton Depression Rating Scale. B: Node statistics of the symptoms of depressive disorders at week 52. AGI: agitation, ANP: anxiety psychic, ANS: anxiety somatic, DEP: depressed mood, GAS: somatic symptoms gastro-intestinal, GEN: general somatic symptoms, GUI: feelings of guilt, HYP: hypochondriasis, IEA: insomnia: early in the night, IMI: insomnia: middle of the night, IMO: insomnia: early hours of the morning, INS: insight, RET: retardation, SEX: genital (sexual) symptoms, SUI: suicide, WOR: work and activities.
DISCUSSION
The present study found successive changes in the identities of the most central domains within the networks of depressive symptoms across the course of treatment. Reflecting the progressive decrease in the HAMD total score from baseline to week 52, the estimated network structures were continually reorganizing. Whereas anxiety (psychic) was the most centrally situated within the estimated network structures in the early period (baseline and week 2), loss of weight was the most centrally situated in the late period (weeks 25 and 52). It is well known that anxiety (psychic) is included in the non-DSM symptoms of depressive disorders, although loss of weight is included in the DSM symptoms. These findings are consistent with the fact that in patients with major depression, DSM symptoms have been observed to be no more central than non-DSM symptoms within the symptom networks [22,23]. In addition, we found that the edges were stronger in the later period than in the initial period. The clinical significance of the increased number of strong edges is not certain, but we speculate that this increase is associated with the reduction of depressive symptom severity over the course of treatment and the concomitant boundary blurring of individual depressive symptoms. Furthermore, the edges among insomnia symptoms, between anxiety (psychic) and agitation, and between feelings of guilt and suicide remained consistent from baseline to week 52. In light of factor analysis and the results of using the change in the aggregate total depression score in clinical trial research [35,36], we conclude that, remarkably, the successive changes that we observed in the most central symptom domains are partly inconsistent with the unidimensional concept of depression. Thus, we speculate the following: 1) network analysis of depressive symptoms may overcome the limitations of the use of changes in the total scores of depression scales in clinical trials, 2) a period-differentiated and symptom-focused approach across the clinical course of depressive disorders is needed, and 3), the reorganization of network structures and the changes in the HAMD total score in the course of antidepressant treatment offer complementary information.
Hilland et al. [37] estimated the links between specific depressive symptoms and specific brain structures using network analysis. The study established positive associations, including crying-cingulate, crying-fusiform gyrus, irritability-fusiform gyrus, irritability-hippocampus, loss of interest-hippocampus, self-criticism-fusiform gyrus, and worthlessness-cingulate. Negative associations were also established, including changes in appetite-hippocampus, loss of interest in sex-insula, sadness-cingulate, sadness-hippocampus, and sadness-insula. We therefore speculate that the successive changes we observed in the most central domains are related to successive changes in the activities and functions of specific brain structures across the clinical course of depressive disorders. Herein, it is assumed that the observed sequence of the most central symptom, i.e., anxiety (psychic) → anxiety (psychic) → work and activities → loss of weight → loss of weight is closely associated with activity changes in the hippocampus, fusiform gyrus, and cingulate gyrus over the course of recovery.
Our study has several limitations. First, the restricted range of the Likert scale (0–4) may contribute to an estimation bias in the centrality measures because symptoms with smaller means and variances may have a limited probability of manifesting pronounced associations with other symptoms [26,27]. Our study found that depressed mood, which has been reported to have a higher mean value and a lower standard deviation than psychic anxiety and other symptoms, showed more frequent representation than psychic anxiety or other symptoms. However, we found that the Pearson correlation coefficient (r) between the standard deviation and the node-strength centrality of the HAMD items was negligible; no consistent relationship was found that had the potential to bias the results. Second, all study participants were South Korean patients with depressive disorders. Therefore, we cannot exclude the possibility that the estimated network structures of the HAMD items may be affected by some symptom presentation unique to our study population; thus, the generalizability of our findings to other populations may be limited. Third, the estimated network structures may be affected by our policy of excluding participants whose data containing missing values. Fourth, the estimated network structures may have been influenced by the characteristics of the study participants, particularly with respect to medication. Following the CRESCEND study design, we included participants medicated with any class of antidepressant and switched to any other class of antidepressant over the course of the study. Therefore, the CRESCEND study design may have been a moderator of the observed network structure of depressive symptoms. Thus, similar to previous network analyses of symptom changes [35,38], our findings have been moderated by the heterogeneity of the study subjects.
Despite these limitations, we have revealed successive changes in the network structures of depressive symptoms in a large sample of patients with depressive disorders. In addition, the network structures of depressive symptoms could be affected by the relatively high proportions of middle-aged women among the participants. In further studies, such analyses should be performed in a less heterogeneous sample of patients with depressive disorders. These limitations may be offset by our strategy of examining the successive changes in the most central symptom domains within the severity networks. It is speculated that the clinically significant symptom domains such as anxiety (psychic), suicide, work-and-activities, and weight loss may be differentiated based on the treatment time course specific to a given depressive disorder.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) (grant no. 2019R1A2C1090146). We would like to thank Dr. Jinseob Kim for his valuable help with the network analysis.
Notes
The authors have no potential conflicts of interest to disclose.
Authors’ contribution
Conceptualization: Seon-Cheol Park, Yaeseul Kim, Kiwon Kim, Eun Young Jang. Data curation: Young Sup Woo, Jung-Bum Kim, Eun Young Jang, Hwa-Yong Lee, Hyeon-Woo Yim, Byung-Joo Ham, Jae-Min Kim, Yong Chon Park. Methodology: Seon-Cheol Park, Yaeseul Kim, Kiwon Kim, Eun Young Jang. Supervision: Young Sup Woo, Jung-Bum Kim, Eun Young Jang, Hwa-Yong Lee, Hyeon-Woo Yim, Byung-Joo Ham, Jae-Min Kim, Yong Chon Park. Writing—original draft: Seon-Cheol Park.