Neuronal Signatures of Negative and Positive Schemas towards the Self and Others in Patients with Early Stage Schizophrenia
Article information
Abstract
Objective
The present study investigated the functional neuroanatomy underlying negative and positive schemas towards the self and others in patients with early stage schizophrenia spectrum disorders (SSDs) using a task-based fMRI procedure.
Methods
This study included 50 patients with SSDs and 52 controls. The schema-evoking task consisted of four active conditions and neutral condition. Differences in brain activation were compared between the two groups. Correlation analysis was performed between task-related activation and psychopathology.
Results
The SSD patients exhibited higher activity of the left middle and inferior frontal gyri under the negative-others minus neutral contrast as well as greater activation of the left superior and middle frontal gyri and right medial superior frontal gyrus under the positive-self minus neutral and positive-others minus neutral contrasts. Under the positive-others minus neutral contrast, negative correlation was observed between activity of the right inferior parietal gyrus and right angular and total score of the Positive and Negative Syndrome Scale (PANSS), whereas positive correlation between activity of the left middle cingulate gyrus and left/right precuneus and positive-others score of the Brief Core Schema Scales (BCSS).
Conclusion
The present findings suggest that the frontal brain regions of SSD patients are more sensitive to negative and positive schemas towards the self and/or others compared to those of controls.
INTRODUCTION
Schizophrenia is the most representative severe mental illness. It is a very complex and heterogeneous disorder that involves synergistic interactions among various biological, psychological, and social factors to manifest its symptoms. Recently, there has been emerging interest towards the self-disorder of schizophrenia [1]. Using various designs of task-based fMRI, neural correlates underlying the psychopathology related to self or others in schizophrenia can be investigated.
People with chronic psychosis report extreme negative evaluations of the self and others [2], and these negative schemas are thought to be formed early in life and then remain stable throughout adulthood [3]. It has been suggested that sexual and physical abuse experienced during childhood contribute to the development of schemas related to the “hazard” theme, whereas childhood neglect may lead to the development of schemas related to themes of “loss” and “insignificance” [4]. Moreover, negative schemas or thoughts can induce depression [5] or suicidal behavior [6] in young persons, and negative evaluations about the self and others or negative self-concepts may be associated with the formation of delusions and hallucinations [7,8]. Negative schemas are also associated with suicidal ideation in patients with psychosis [9] and play a vital mediating role in the link between cyclothymic-hypersensitive temperament and suicidality in patients with first-episode psychosis [10].
The use of neuroimaging studies to identify the neural correlates of negative schemas in patients with schizophrenia is critically important for furthering the current understanding of its pathophysiology and informing the development of future therapeutic agents. Comparisons of functional magnetic resonance imaging (fMRI) scans during self-referential versus non-self-referential tasks in healthy volunteers revealed that several cortical midline structures, including the medial prefrontal cortex (mPFC), anterior cingulate cortex (ACC), and posteromedial cortices, are key regions involved in the processing of self-referential stimuli [11]. A meta-analysis of neuroimaging studies investigating neural correlates of self-reflection in schizophrenia reported that the ventral mPFC is responsible for tagging information relevant for ‘self’, whereas the dorsal mPFC is responsible for evaluation and decision-making processes in self- and other-referential processing [12]. Other recent fMRI studies employed self-referential stimuli also demonstrated deficits in the activation of the mPFC and ACC in patients with schizophrenia [13,14]. However, these studies did not address the neural correlates underlying more specific aspects of self, such as a positive or negative sense of self.
On the other hand, two previous studies may provide hints about the brain regions implicated in the perception of positive- or negative-self in patients with schizophrenia [15]. presented trait adjectives that were categorized as positive, negative, mental illness-related, or physical illness-related and asked participants to judge whether these words applied to themselves, another person, or whether they contained the letter “a”. They observed hypoactivation of left superior frontal gyrus during negative self traits evaluation in patients vs. controls [16]. asked people with schizophrenia and healthy controls to respond to word stimuli with a prespecified emotional valence (positive, negative, or neutral) while inhibiting responses to a stimulus with a different valence. Patients with schizophrenia were found to have failed activation of prefrontalparietal network during response inhibition to negative words. In terms of methodological aspects, the first one used adjectives, not sentences and its sample size was very small. The second one measured neural activity during response inhibition, not the activity induced by stimuli. Therefore, these two study designs appear to be insufficient to address the question at hand, and thus, further exploration of the neural substrates related to negative or positive schemas of the self and others are required.
We hypothesized that neural activation to the stimuli of negative and positive schema would be different in early stage patients with schizophrenia spectrum disorders (SSDs) compared to healthy controls. The present study aimed to identify the neural correlates associated with negative and positive schemas of the self and others between the two groups. Considering reported associations between negative evaluation and positive symptoms [7,8], the relationship between task-related activation and psychopathology was also explored. We had a special focus on studying early stage patients because of less concern with cognitive impairment, accumulative effects of antipsychotics and disease process.
METHODS
Participants
For this study, 56 individuals with patients with early stage SSD (32 with schizophrenia and 24 with schizophreniform disorder) were recruited from Jeonbuk National University Hospital, Jeonju, Republic of Korea. Early stage was defined as having a duration of illness (DI) of ≤5 years. Of these 56 individuals, all were stable outpatients with no change in medication during last 3 months, and all diagnoses were made using the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Axis I Disorders (SCID-I) [17]. Patients with alcohol or drug use disorders within the past 6 months, an intellectual disability (IQ ≤70), current or historical neurological disorders, a serious medical illness, pregnancy, and/or claustrophobia were excluded from the study.
Additionally, healthy participants were recruited for the control group via advertisements. These participants were age- and sex-matched to the patient group, interviewed using the axis I diagnoses with the SCID-I Non-Patient Edition (SCID-NP) [18], and required to have no previous or current psychiatric disorders, neurological disorders, or significant medical conditions and no family history of psychotic disorders. All healthy controls were between 19 and 50 years of age and were assessed as right-handed using the Edinburgh Handedness Inventory [19]. All participants joined this study voluntarily and provided written informed consent. The study was approved by the Ethics Committee of Jeonbuk National University Hospital (approval number: CUH 2012-08-001).
Clinical assessments
The severity of symptoms within the week prior to the fMRI experiment was evaluated in each SSD patient using the Positive and Negative Syndrome Scale [20], which was administered by trained psychiatrists. Additionally, beliefs about the self and others were evaluated with the Brief Core Schema Scales (BCSS) [2], which yield subscale scores for negative-self, positive-self, negative-others, and positive-others schemas.
Schema task
The first 50 candidate sentences in the schema task described four schemas (negative-self, negative-others, positive-self, and positive-others) that were developed based on a classic list of personality trait words [21], the Automatic Thought Questionnaire [22], and the Affective Norms for English Words wordlist [23]. The healthy controls evaluated the sentences in terms of appropriateness for schema evocation, ease of understanding, and valence using a visual analogue scale (VAS) ranging from 0 to 10. Sentences that were rated ≥7 for all items were selected, and the lengths were adjusted to be balanced over the four schemas. Finally, a psychiatrist and clinical psychologist selected 30 sentences for each schema to be used in the task.
For the neutral stimuli, 50 candidate sentences that described simple facts or knowledge were prepared. The healthy controls evaluated the sentences in terms of ease of understanding and valence. Sentences rated ≥7 for ease of understanding with the VAS and those that were rated close to “0” for valence using an 11-point Likert scale (-5 to +5) were selected and then finalized by the psychiatrist and clinical psychologist. Any sentences that were not selected were used for preliminary training prior to fMRI.
The fMRI procedure comprised a block design with five task conditions and one rest condition (Figure 1). An example of each condition was “I am ugly,” “I am honest,” “Other people are cruel,” “Other people are kind,” and “Rabbits are faster than turtles” for negative-self, positive-self, negative-others, positive-others and neutral condition respectively. There were five runs, with each run containing five blocks for each condition, and each block containing six trials in which a sentence was displayed for 3 s. Participants were instructed to press the button anytime during three seconds of stimulus display. If they agreed with contents of negative- and positive-sentences or thought that contents of neutral sentences were correct, right button was pressed (vice versa). To control for order effects, the blocks in each run were presented in random order with no consecutive blocks from the same condition. During the rest condition that was inserted between the task conditions, a fixation cross was shown for 18 s. Prior to the functional run, the participants completed practice trials to become familiarized with the tasks. The total scan time for one session (25 blocks for the task condition and 25 rest conditions) was 15 min.
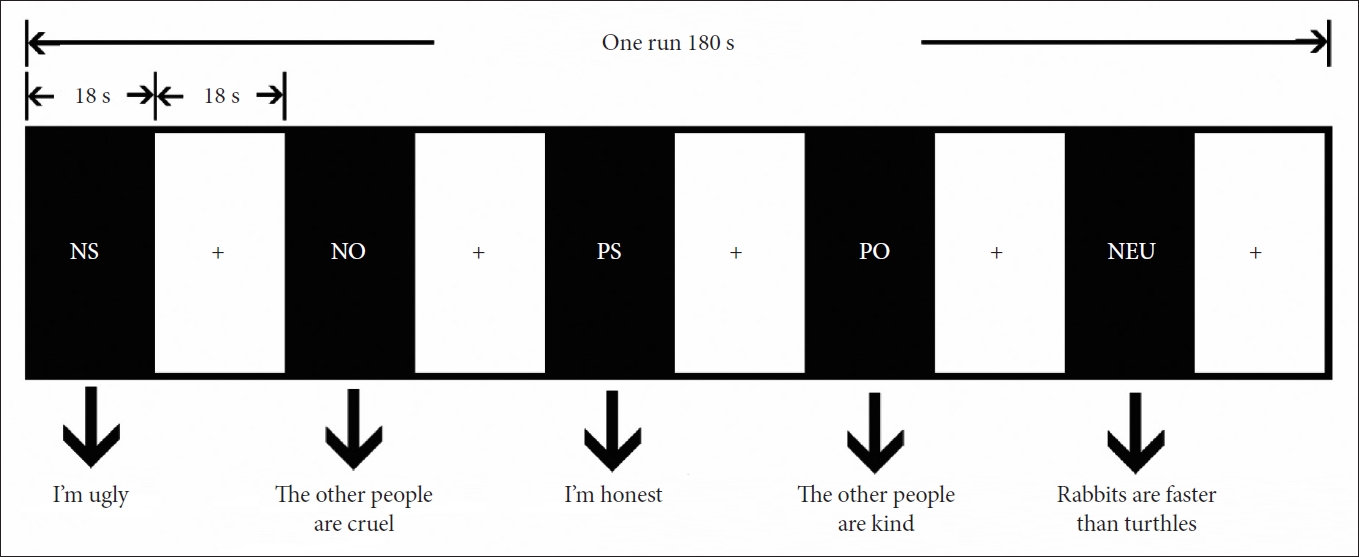
Task design. Every block contains six sentences each of which was presented for 3 s. Fixation cross was shown 18 s between every block. The session contains five runs. The session contains five runs. NS: negative-self block, NO: negative-others block, PS: positive-self block, PO: positive-others block, NEU: neutral block, Fixation cross: rest block.
Image acquisition and preprocessing
All fMRI data were acquired at Jeonbuk National University Hospital using a 3T Siemens Verio scanner (Siemens Medical Solutions, Erlangen, Germany) with 45 mT/m gradients and a 12-channel standard quadrature head coil. Transaxial functional scans were acquired using a single-shot T2*-weighted gradient-echo-planar imaging sequence that depicted the blood oxygenation level-dependent (BOLD) signal with the following parameters: repeat time (TR)=3 s, echo time (TE)=30 ms, field of view (FOV)=240 mm, acquisition matrix=64×64, flip angle=90°, gap=0.8 mm, 302 volumes (36 contiguous axial 3-mm-thick slices), and even-first interleaved acquisition. Prior to BOLD imaging, axial 1.0-mm-thick T1-weighted spin-echo images (TR=1,900 ms, TE=2.5 ms, flip angle=9°, FOV=240 mm, and image matrix=256×246 mm) were acquired as an anatomical reference. The first three volumes were discarded to account for T1 saturation.
All processing of the fMRI data was conducted using SPM12 software (https://www.fil.ion.ucl.ac.uk/spm/software/spm12). Functional images were corrected for slice acquisition time within each volume, motion-corrected by realigning to the first volume, and co-registered with the anatomical data of each participant. Then, the functional data were transformed into a standard anatomical space based on the parameters obtained by spatially normalizing each T1 image to the Montreal Neurological Institute (MNI) template. The normalized images were smoothed with an 8-mm full-width-at-half-maximum Gaussian filter, and then a high-pass filter with a cut-off period of 128 s was implemented to remove low-frequency drifts from the time series. The processed data were examined for excessive motion artifacts using the Artifact Detection Tool software package (http://web.mit.edu/swg/art/art.pdf; http://www.nitrc.org/projects/artifact_detect). In total, six patients were excluded due to excessive head movements [24] based on the following criteria: a maximum absolute head motion displacement of >2 mm along the x/y/z axes and yaw/pitch/role rotation >2°.
Analyses of the imaging and clinical data
First-level analyses were performed for each participant and each contrast (negative-self minus neutral, negative-others minus neutral, positive-self minus neutral, and positive-others minus neutral). Then, in the second-step analyses, one-sample t-tests were performed to generate within-group activation maps, and between-group two-sample t-tests were performed for each corresponding contrast; all group comparisons included education as a covariate. As we did not have prior hypothesis, whole brain analysis was performed. Activations were considered to be significant at p-values with a family-wise error <0.05 (pFWE) and a cluster size threshold of >20 voxels. Between-group analysis was performed again with drug-naïve or drug-free patients (n=23) and age and sex-matched controls (n=23). Finally, in the patient group, multiple regression analyses were conducted to assess the relationships between the PANSS or BCSS score and mean activation values of the areas showing a difference under each contrasted condition using age, sex, and duration of illness as covariates. Results were considered to be significant at pFWE <0.05 and cluster size threshold >20 voxels.
To plot the correlation graphs, β-values (mean values of the areas) were extracted using MarsBaR (http://marsbar.sourceforge.net/) for significantly correlated regions. For the behavioral data, either a two-way analysis of variance (ANOVA) or t-tests were performed. When comparing two groups, either independent t-tests or chi-square tests were conducted depending on the variable type.
RESULTS
Participant characteristics
Comparison of the demographic information of SSD patients and healthy controls revealed that there was a significant difference in education level. All subscale scores on the BCSS, except for that of positive-others, differed significantly between the patients and controls (Table 1). Of the 50 SSD patients, 14 were antipsychotic-naïve, 9 were antipsychotic-free, and 27 were medicated. The mean chlorpromazine-equivalent dose for the patients was 250.74±133.77 mg/day [25-27].
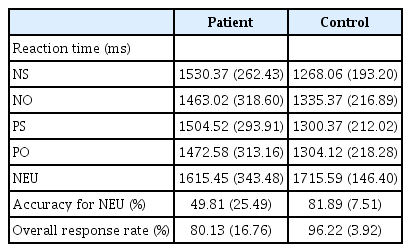
Behavioral data
A two-way ANOVA of the reaction time (RT) data that included group and condition type as factors revealed that the main effects of group (F1,55=20.48, p<0.001) and condition (F4,55=13.44, p<0.001) were significant, as well as the group×condition interaction (F4,55=4.51, p=0.001). Post-hoc t-tests revealed that the SSD patients exhibited significantly longer RTs under negative-self (t=4.63, p<0.001), positive-self (t=3.25, p=0.002), and positive-others (t=2.54, p=0.014) conditions compared to the healthy control group. The patients also exhibited significantly lower levels of accuracy under the neutral condition (p<0.001) and lower overall response rates (p<0.001) compared to the healthy controls (Table 2).
fMRI data
One-sample analysis
Under all contrasted conditions, activation differences were most commonly observed in the frontal gyrus and precuneus and less frequently in the temporal gyrus, cingulate gyrus, insula, or thalamus in both the patient and control groups (Figure 2); a more detailed description is provided in the Supplementary Material, Supplementary Table 1 and 2 (in the online-only Data Supplement).
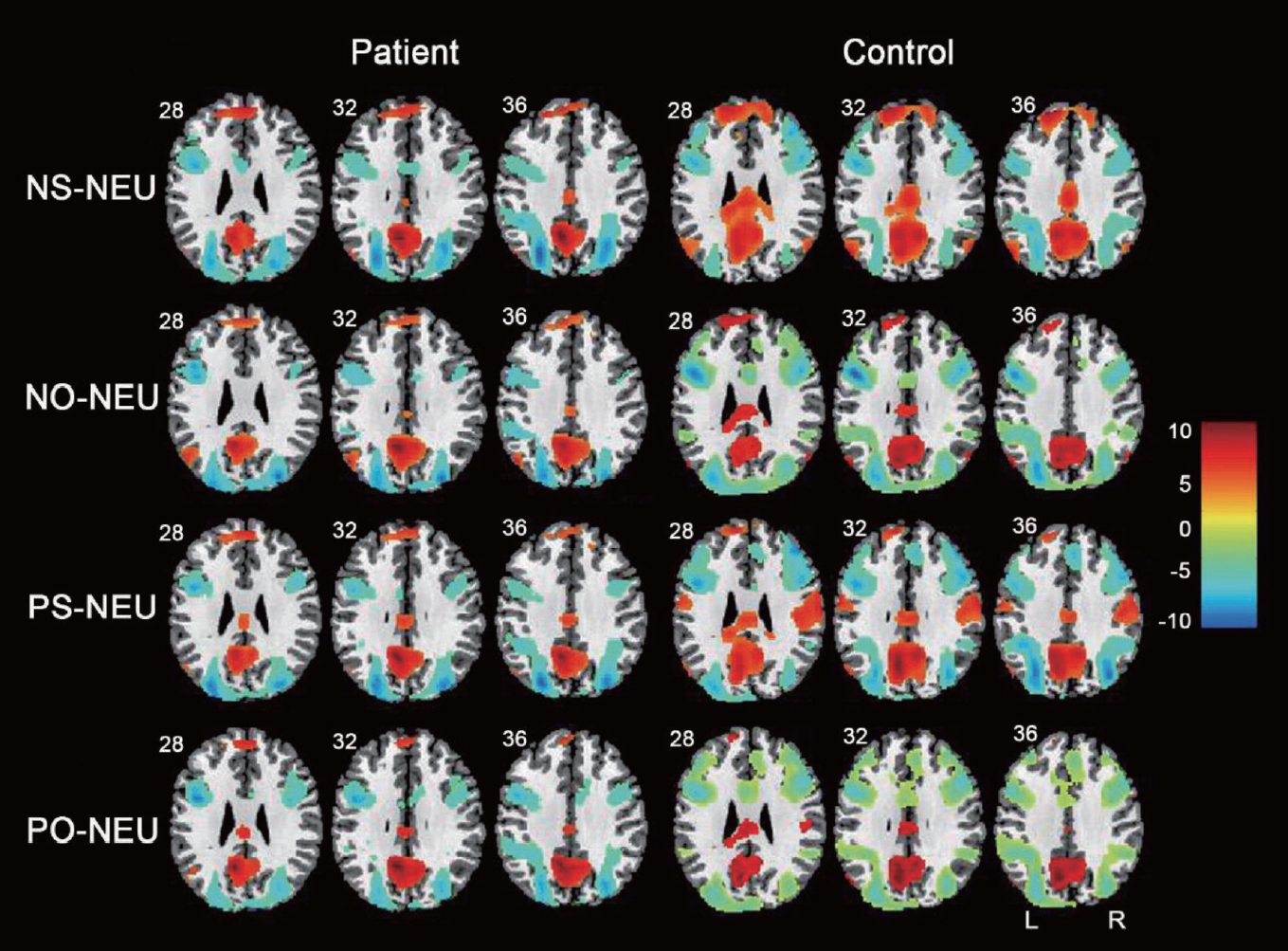
Brain activation during the NS-NEU, NO-NEU, PS-NEU and PO-NEU contrasts in patients and healthy controls. Left is patient group, right is healthy control group. Warm colors indicate increased activation, cool colors represent decreased activation. The number below each slice indicates slice location (mm) of MNI z coordinate. NS-NEU: negative-self minus Neutral contrast, NO-NEU: negative-others minus neutral contrast, PS-NEU: positive-self minus peutral contrast, PO-NEU: positive-others minus peutral, MNI: Montreal Neurological Institute.
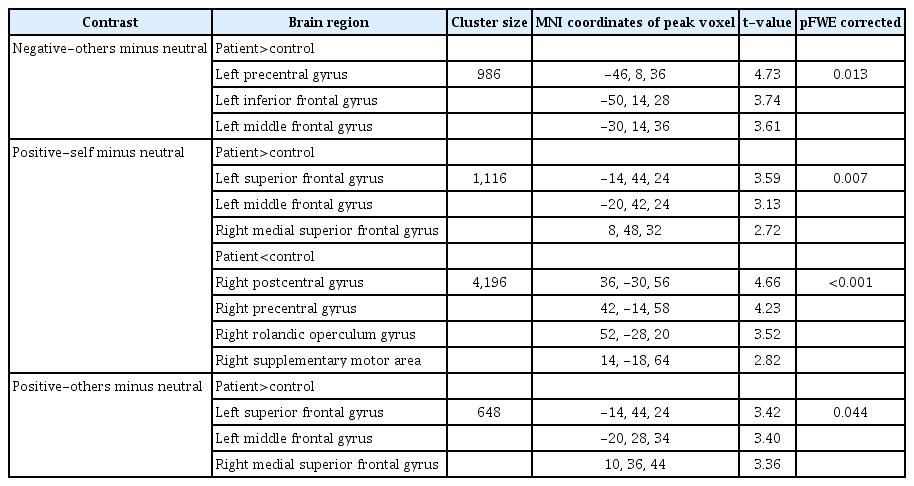
Group comparisons
Negative-self minus neutral. There was no significant difference between the two groups. However, in subgroup analysis, patients with drug-naïve or drug-free state showed hyperactivation in the left superior frontal and inferior frontal gyri and hypoactivation in the right insula, and right postcentral and parahippocampal gyri (Supplementary Table 3 in the online-only Data Supplement).
Negative-others minus neutral
The SSD patients exhibited relatively higher activity in the left precentral gyrus (t=4.73, MNI coordinates: -46, 8, 36), left inferior frontal gyrus (t=3.74, MNI coordinates: -50, 14, 28), and left middle frontal gyrus (t=3.61, MNI coordinates: -30, 14, 36) compared to the healthy controls. In subgroup analysis, patients showed hyperactivation in the right anterior cingulate gyrus and cerebellum crus 2 (Supplementary Table 3 in the online-only Data Supplement).
Positive-self minus neutral
The SSD patients exhibited significantly higher activity in the left superior frontal gyrus (t=3.59, MNI coordinates: -14, 44, 24), left middle frontal gyrus (t=3.13, MNI coordinates: -20, 42, 24), and right medial superior frontal gyrus (t=2.72, MNI coordinates: 8, 48, 32) compared to the healthy controls. Additionally, the SSD patients exhibited significantly lower activity in the right postcentral gyrus (t=4.66, MNI coordinates: 36, -30, 56), right precentral gyrus (t=4.23, MNI coordinates: 42, -14, 58), right Rolandic operculum gyrus (t=3.52, MNI coordinates: 52, -28, 20), and right supplementary motor area (t=2.82, MNI coordinates: 14, -18, 64) compared to the healthy controls. In subgroup analysis, patients showed hyperactivation in the right superior frontal, inferior frontal operculum, middle temporal gyri and left precuneus (Supplementary Table 3 in the online-only Data Supplement).
Positive-others minus neutral
The SSD patients exhibited significantly (pFWE <0.05, cluster size >20) higher activity in the left superior frontal gyrus (t=3.42, MNI coordinates: -14, 44, 24), left middle frontal gyrus (t=3.40, MNI coordinates: -20, 28, 34), and right medial superior frontal gyrus (t=3.36, MNI coordinates: 10, 36, 44) compared to the healthy controls (Table 3, Figure 3). In subgroup analysis, patients showed hyperactivation in the cerebellum 6 and crus 1 (Supplementary Table 3 in the online-only Data Supplement).

Comparison between patients and healthy controls in the NO-NEU, PS-NEU and PO-NEU contrasts. Warm colors indicate greater activation in patients than controls whereas cool colors represent decreased activation in patients. The number below each slice indicates slice location (mm) of MNI z coordinate. NO-NEU: negative-others minus neutral contrast, PS-NEU: positive-self minus neutral contrast, PO-NEU: positive-others minus neutral contrast, MNI: Montreal Neurological Institute.
Correlations
Under the positive-others minus neutral contrast, there were significant negative correlations (r=-0.567, p<0.05) between the PANSS total score and activation at the regional cluster including right angular gyrus (AG; MNI coordinates: 38, -64, 50) and right inferior parietal gyrus (MNI coordinates: 40, -54, 52). For the BCSS, the positive-others score was significantly and positively correlated (r=0.497, p<0.05) with activation at the regional cluster including left middle cingulate gyrus (MNI coordinates: -8, -44, 54), right cuneus (MNI coordinates: 16, -70, 36), left precuneus (MNI coordinates: 10, -50, 52) and right precuneus (MNI coordinates: 6, -42, 54) under the same contrast (Figure 4).

Correlation between the PANSS total score or BCSS score and brain activation during the positiveothers minus neutral contrast in patients with SSD. A: Negative correlation of the PANSS total score with the activity in the right angular gyrus and right inferior parietal gyrus. B: Positive correlation of positive-others score of the BCSS with the activity in the left middle cingulate gyrus, right cuneus and left/right precuneus. PANSS: Positive and Negative Syndrome Scale, BCSS: Brief Core Schema Scale, SSD: schizophrenia spectrum disorders.
DISCUSSION
Patients with schizophrenia often have deep-rooted negative-self or -others schemas that are closely associated with the formation of positive symptoms and suicidality during psychosis. Thus, the present study was based on the assumption that there would be differences in brain activation in response to self- or others-related negative and positive sentences between SSD patients and healthy controls.
In the present study, the SSD patients showed relatively higher activity in the left middle and inferior frontal gyri and left precentral gyrus compared to the healthy controls under the negative-others minus neutral contrast. It should be noted that percent signal changes of contrast images in both patients and controls were minus values and its value was greater in controls (data not shown). Therefore, it seems that higher activity in patients can be interpreted as less deactivation under this contrast compared to controls. As both patients and controls showed negative percent signal changes under negative-others condition, this suggests that task of negative-others condition may be associated with neuronal inhibition which may in turn decrease BOLD signal. This speculation may be supported by the finding that negative contrast values were observed in the right middle and superior frontal gyri of patients with schizophrenia during response inhibition to negative compared with neutral words [16]. However, in that same study [16], healthy controls showed positive contrast values which is opposite to our result. It has been reported that in healthy controls, negative self-related sentences induce hyperactivation of the dorsomedial prefrontal cortex (dmPFC), ACC, and insula [28] and forgetting negative self-referential information is associated with more widespread activation that includes the middle frontal gyrus and inferior frontal gyrus [29]. Direct comparison of these results should be cautious given that details of the tasks and participant’s characteristics were different. In order to deepen understanding and implication of related findings, percent signal change of each condition needs to be verified which most of studies seldom provide. Nevertheless, relatively higher activity in the middle/inferior frontal gyrus and precentral gyrus of schizophrenia patients during negative-other minus neutral contrast resonates with the findings of two previous studies: relatively higher activity in the right superior and middle frontal gyri of patients under the refusal minus acceptance condition [30] and relative overactivity in the left superior frontal gyrus of patients during self-evaluation in response to negative trait adjectives [15]. Interpretation of less deactivation to negative stimuli in patients compared to controls may be that neural plasticity in patients is so rigid that inefficient response to negative stimuli may occur in patients. It should be noted that we did not observe significant difference of brain activation between the two groups under the negative-self minus neutral contrast despite of significantly higher score of negative-self in patients compared to controls. One explanation for this discrepant finding may be that mental states of patients could have been different between the time points of scan and assessment of the BCSS performed. Alternatively, actual environmental conditions for scanning and scale assessment are quite different that the results from the two conditions do not necessarily have to be the same. Last but interesting possibility could be related to the results of subgroup analysis. As drug-naïve/free patients showed significantly different activations under negative-self minus neutral contrast, antipsychotics may have exerted dampening effect on brain activation but not on the scale performance.
In the present study, the SSD patients exhibited greater activation in the left superior and middle frontal gyri and right medial superior frontal gyrus than the healthy controls in the positive-self and -others minus neutral contrasts. These findings are in contrast with those of Bedford et al. [15], who observed no significant findings in patients with schizophrenia compared to controls during self-evaluation in response to positive trait adjectives. Other studies have reported that control participants exhibit increased activity in the right dmPFC and left ventromedial PFC in response to positive self-related sentences or words [28,31]. Therefore, the present results appear to be counterintuitive. It is possible that repulsion towards positive descriptions of the self or others may have played a role in the induction of greater activation of the frontal regions of SSD patients compared to controls. Alternatively, it may suggest that patients need more blood perfusion to process positive stimuli because of inefficient neural mechanisms. Previous findings showing that people with schizophrenia do not deactivate the cingulate areas during response inhibition to positive words [16] partially support this notion. Moreover, the precentral gyrus and postcentral gyrus are primary sensory and motor cortices, respectively [32], and are typically active during any task that involves movement [33]. Likewise, the Rolandic operculum gyrus is activated during visual stimulation [34]. The present findings showing lower levels of activity in the pre- and postcentral gyri, the Rolandic operculum gyrus, and supplementary motor areas in SSD patients may have been due to their slow sensorimotor responses, which was reflected in the longer RTs for pressing the button.
In the present study, correlation analyses revealed negative relationships between the PANSS total score and activity in the right angular and inferior parietal gyri. The AG is involved in semantic processing, word reading and comprehension, number processing, the default mode network, memory retrieval, attention, spatial cognition, reasoning, and social cognition [35]. The role of the inferior parietal lobe (IPL) is to maintain attentive control during current task goals as well as to respond to salient novel information or alerting stimuli in the environment [36]. The percent signal changes in the angular and parietal gyri under the positive-others condition were negative values suggesting presence of deactivation. Based on the functional roles of the AG and IPL and their negative signal changes, it is possible that more severe abnormalities in these regions may result in a greater degree of dysregulation in terms of neurocognition and social cognition, which, in turn, could manifest as a more severe psychopathology.
Interestingly, in the present study, the positive-others score on the BCSS was positively correlated with activity in the left middle cingulate gyrus and left or right precuneus/cuneus. The cingulate cortex processes cognitive, emotional, and social information [37]. The middle cingulate cortex (MCC) is the dorsal portion of the ACC and has the highest level of connectivity with areas related to cognitive (dorsal PFC) and motor (premotor and motor cortices) functions [38]. The precuneus is involved in a wide variety of highly integrated tasks such as visuospatial imagery, episodic memory retrieval, and self-processing operations, including taking a first-person perspective and the experience of agency [39]. The cuneus (Brodmann area 17) receives visual information from the same-sided superior quadrantic retina and is primarily involved in basic visual processing. Taken together, these findings indicate that higher activities in the MCC and precuneus are associated with a greater degree of taking a positive perspective towards others, even though the positive-others score was low for the SSD patients in this study. Its implication may be that any interventions, drugs or transmagnetic brain stimulation, targeting to enhance blood perfusion or neural activity in the MCC and precuneus would be helpful in treating patients. On the other hand, it was unexpected results not observing significant correlation with other contrasts given that the scores of negative-self and negative-others in patients were significantly higher than controls. Considering that total score of the PANSS in patients was relatively low, it may be that performing the task of positive-others rather than negative related task might have been more strenuous which may be related to the severity of psychopathology.
The present study has several limitations that should be considered. First, the participants were stable and exhibited mild levels of symptomatology and thus, the PANSS may not be sufficiently sensitive to detect correlations between its subscale scores and activation signals. The use of more detailed and comprehensive scales, such as the Psychotic Symptom Rating Scales [40], may produce different results. Second, although education was included as a covariate in the analyses, this does not rule out the possible contribution of education to the group differences in regional activation. Thus, a more careful recruitment process for healthy control participants will be necessary in the future. Third, most patients in the present study were medicated and this fact should be considered when interpreting the results. Despite these caveats, the present study is the first to provide evidence of the neural signatures related to negative and positive schemas towards the self and others in SSD patients.
In conclusion, the present negative and positive schema task revealed that SSD patients exhibited significantly different activations under the negative-others minus neutral contrast and positive-self and -others minus neutral contrasts compared to healthy controls. These findings suggest that the frontal regions are more sensitive and showing inefficient response to negative and positive schemas of the self and/or others in SSD patients compared to healthy subjects.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2020.0335.
Acknowledgements
The corresponding author would like to thank all participants in the study and the Father in Heaven. The authors report no biomedical financial interests or potential conflicts of interest.
This study was supported by a grant from the Korean Mental Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HL19C0015) and a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, which is funded by the Ministry of Health & Welfare, Republic of Korea (HI18C2383).
Notes
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Young-Chul Chung. Data curation: Young-Chul Chung, Jie Shen. Formal analysis: Jie Shen, Guangfan Shen. Funding acquisition: Young-Chul Chung. Investigation: Guangfan Shen. Methodology: Woo-Sung Kim, Jie Shen. Project administration: Woo-Sung Kim, Congcong Liu, Guangfan Shen, Uyanga Tsogt. Resources: Woo-Sung Kim. Software: Woo-Sung Kim. Supervision: Young-Chul Chung. Validation: Young-Chul Chung. Visualization: Guangfan Shen. Writing—original draft: Guangfan Shen, Jie Shen. Writing—review & editing: Young-Chul Chung.