Effects of Organic Light-Emitting Diodes on Circadian Rhythm and Sleep
Article information
Abstract
Objective
Organic light-emitting diodes (OLEDs) emit less blue light than traditional light-emitting diodes (LEDs), and we previously found that early-night OLED light exposure (LE) delays the melatonin phase by less than LED at a color temperature of 4,000 K. As a follow-up study, we investigated the effects of OLED and LED at a different color temperature (3,000 K) on melatonin profile, sleep, and vigilance.
Methods
24 healthy subjects (27.5±5.1 years) were exposed to three light conditions [OLED, LED, and dim light (DL)] from 17:30 to 24:00, in a random order and with a 1-week interval. Saliva samples for melatonin were taken every hour from 18:00 to 24:00. Polysomnography (PSG) and a psychomotor vigilance test (PVT) were performed.
Results
Melatonin onset time was significantly delayed under OLED and LED compared with DL, with no significant difference between OLED and LED. The mean melatonin level at 24:00 under LED was lower than that under DL, but there was no significant difference between OLED LE and DL. The percentage of slow wave sleep (N3) in LED was significantly lower than in OLED.
Conclusion
Exposure to light in the evening can suppress melatonin secretion late at night and disturb deep sleep, and those effects are slightly worse under LED than OLED.
INTRODUCTION
The harmful effects of light at night on humans are now well recognized by the general public. As previously reported, people exposed to light at night can have increased incidence of a wide range of illnesses, including sleep and psychiatric disorders, obesity, diabetes, and several kinds of cancers. In modern society, people are routinely exposed to electrical lighting during evening hours, after the onset of melatonin production, to partake in work, recreational, and social activities. Gooley et al. [1] reported that this indoor room light profoundly alters the timing, duration, and amount of melatonin synthesis, the health consequences of which are unknown. Blue light, which is particularly beneficial during the daytime, seems to be more disruptive at night, and induces the strongest melatonin inhibition [2]. Sensitivity of human nocturnal melatonin suppression [3,4] peaks in the blue portion of the light spectrum around 460 nm, most effective in the range between 446 and 477 nm [5]. Because photoresponse such as adaptation of the circadian clock is mediated by retinal ganglion cells expressing the photopigment melanopsin which is most sensitive to blue light, blue wavelengths can potentially exert more powerful effects on human circadian rhythm than green and yellow wavelengths [5,6].
Nocturnal blue light exposure is currently increasing, due to the proliferation of energy-efficient lighting [light-emitting-diodes (LEDs)] and electronic devices. Thus, the development of lighting systems that preserve the melatonin rhythm could reduce the health risks induced by chronodisruption [2]. Organic light-emitting diodes (OLEDs), which emit less blue light than traditional LEDs, are an energy-efficient and physiologically friendly form of lighting [7,8]. OLED light exposure (LE) could decrease the adverse health outcomes of artificial light at night, but no studies have investigated its effects on sleep quality and the circadian system. Our team previously conducted the first direct comparative study of how OLED and LED affect melatonin profile, sleep, and vigilance. We reported that early-night OLED LE exerts weaker effects on the melatonin phase delay than LED LE at a color temperature of 4,000 K [9].
This is a follow-up to that study. We here investigate the effects of OLED LE and LED LE on melatonin profile, sleep, and vigilance at a different color temperature (3,000 K) that is more commercialized for indoor lighting. Currently, there are two types of OLEDs that are commercially available in the market with color temperatures of 4,000 K and 3,000 K. The 4,000 K color temperautre is used in the office, shopping mall or daily residential outdoor lighting because it provides a normal bright light, while the 3,000 K color temperautre creates a warm atmosphere that makes us feel relaxed, so it is often used for home decoration lighting. Since we have already found that 4,000 K OLED LE affects melatonin secretion, we aimed to see if similar results were obtained with a 3,000 K OLED, which is more commonly used as indoor lighting. In this study, we also hypothesized that evening OLED LE would result in less melatonin suppression, smaller circadian phase delays, and better sleep quality and daytime vigilance compared to LED LE.
METHODS
This study is a follow-up to our team’s previous study [9], and we applied the same laboratory settings and study protocol.
Subjects and study screening
We recruited 24 healthy new patients independently from our previous studies.
Those with chronic medical problems or psychiatric problems, and sleep disorders were excluded through detailed medical history and questionnaires about sleep and mood: the Pittsburgh Sleep Quality Index (PSQI) [10], Beck Depressive Inventory (BDI) [11], and Insomnia Severity Scale (ISI) [12].
We selected only those with intermediate chronotype through a morningness-eveningness questionnaire [13], and monitored their habitual sleep patterns for a week by wrist actigraphy (ActiwatchSpectrum Pro, Philips/Respironics, Bend, OR, USA). Based on the actigraphy data, only adults with intermediate chronotype were selected, and they had a sleep time between 23:00 and 08:00.
Participants were required to avoid unusual LE during the evening and nighttime (e.g., going out during their habitual sleep time) for a minimum of 1 week prior to testing and were instructed to maintain a regular sleep schedule for 1 week prior to participating in this study. Sleep and LE were monitored by wrist actigraphy for all subjects beginning 2 days before each visit.
Study protocol
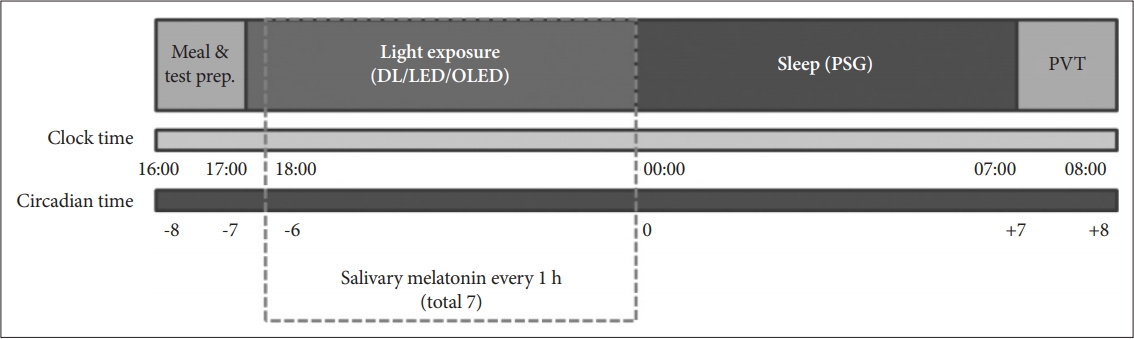
Each subject visited the light control unit a total of 3 times at a time interval of 1 week, and the type of lighting exposed at each visit was different (OLED, LED, or DL). The order of LE was randomized. The study protocol is summarized in Figure 1. Participants were admitted to the unit around 16:00. They consumed the provided meal and then we applied PSG electrodes. Then the experimental LE started at 17:30, for a total of 6.5-h until 24:00. Saliva samples were collected hourly from 18:00 to 24:00. Participants were instructed to sit on a chair and remain awake during the LE. Watching television or using electronic devices was prohibited to prevent any additional LE. During their stay, they avoided consuming alcohol- and caffeine-containing foodstuffs and were allowed to drink only water. The participants went to bed to sleep with the lights off at 24:00 and woke up between 06:00 and 07:00 ad libitum. A psychomotor vigilance test (PVT) was performed for 5–10 min upon awakening. A research assistant kept watch on the wakefulness and procedures of the participants using video and EEG monitoring in the control room of the light-control unit throughout the study.
Light conditions
We changed only the color temperature to 3,000 K, and other light conditions remained the same as in our previous study.9 Three light conditions were tested: 3,000 K OLED LE, 3,000 K LED LE, and dim light (DL; <10 lux). We used ceiling-mounted light panels (LL167RS1-74P1, 300×300 mm, 24 W, LG OLED SQUARE TYPE, Korea; LED Edge panel, 315×315 mm, 20 W, SIGMA LED, Korea). The spectral power distributions of the light produced by the OLED and LED are shown in Supplementary Figure 1 (in the online-only Data Supplement).
The illuminance level of both the OLED light and the LED light at eye level in a sitting position was maintained at 150 lux. A uniform illumination environment was produced in the room. The light illuminance was measured using a lux meter (Testo 540, Testo, Germany). Subjects were in darkness (<0.02 lux, <0.00006 W/m2) during the scheduled sleep time.
Outcome measures of melatonin onset time and suppression
Salivary melatonin was collected using polyester swab Salivettes (Sarstedt, Germany). Samples were stored in the freezer until delivery to the laboratory to measure melatonin concentration, which was performed using liquid chromatography–tandem mass spectrometry. The minimum detectable dose of melatonin (analytical sensitivity) was 0.5 pg/mL. The melatonin onset time was defined as the time that the melatonin level reached or exceeded the threshold of 3 pg/mL [14].
Melatonin suppression was assessed using the area under the time-melatonin concentration curve (AUC) from 18:00 to 24:00 (immediately before lights off) under LED LE or OLED LE compared with the AUC under DL during the same period. Melatonin suppression was calculated as a percentage using the formula 100-[(AUCLE/AUCDL)×100].
Outcome measures of sleep and vigilance
Subjects underwent PSG (Embla N7000 & RemLogic, Denver, CO, USA) each night following LE. Sleep staging and arousals were scored according to the 2017 updated guidelines of the American Academy of Sleep Medicine [15].
PVT was conducted using automated psychometric measures that are commercially available from Joggle Research (https://admin.joggleresearch.com). The following PVT metrics were obtained: mean reaction time, errors (pressing the wrong button or failing to release the button for 3 s or longer), and lapses (reaction time ≥355 ms) [16].
Subjective degree of sleepiness was evaluated through the Stanford Sleepiness Scale (SSS) questionnaire [17].
Statistical analysis
All statistical analyses were performed using SPSS (version 18.0 for Windows, SPSS, Chicago, IL, USA). Data were tested for normality using the Shapiro-Wilk test.
The Friedman test was used to test non-parametric variables. If significant differences among the three light conditions were detected by the Friedman test, we performed post hoc analysis with Wilcoxon signed-rank tests to compare parameters between pairs of light conditions (i.e., DL vs. OLED, DL vs. LED, and OLED vs. LED). Bonferroni correction was applied in multiple comparisons, with significance defined as p<0.017, while p<0.05 was considered indicative of statistical significance in other tests. The Repeated-measures ANOVA (RM ANOVA) was used to compare parametric variables among the three light conditions. If significant differences among the three light conditions were detected by the RM ANOVA, we confirmed post hoc test using Bonferroni correction.
Ethical approval
Our screening and study procedures were approved and monitored by the Institutional Review Board of Samsung Medical Center (IRB No. 2018-10-037) and were conducted in compliance with the Declaration of Helsinki and Good Clinical Practice guidelines. Informed written consent was obtained from all study participants prior to enrollment, and they were financially compensated for their participation.
RESULTS
Subject characteristics
The 24 subjects in this study were aged 27.5±5.1 years (mean±standard deviation), and 17 of them were female. They did not have any definite poor sleep quality (PSQI score=4.9±2.2 and ISI score=4.0±2.2) or depressive mood (BDI score=6.1±5.1). Their sleep logs indicated that their habitual sleep time was between 23:47±01:52 and 07:23±00:57.
Melatonin onset time and suppression
A repeated measures ANOVA with a Greenhouse-Geisser correction determined that melatonin onset time differed significantly among light conditions: 21:24±01:02, 21:49±01:04, and 21:45±01:00 in the DL, OLED, and LED conditions, respectively (p=0.011). Post hoc tests using the Bonferroni correction revealed that OLED and LED LE elicited a delay in melatonin onset time compared to DL (p=0.002 and p=0.015, respectively), whereas there was no significant difference between OLED LE and LED LE (p=0.643).
The mean AUC differed significantly among the three groups: 39.18±39.11, 28.58±30.67, 28.40±33.17 in the DL, OLED, and LED conditions, respectively (p=0.018). The mean AUC under OLED and LED LE was lower than that under DL (p=0.002 and p=0.012, respectively), but there was no statistically significant difference between OLED LE and LED LE (p=0.909). The median suppression percentages for melatonin under OLED LE and LED LE were 18.2% and 24.8%, respectively, but the difference was not significant (p=0.458).
In terms of mean melatonin level by time (18:00–24:00), the groups did not differ significantly from 18:00 to 23:00. However, the mean melatonin level at 24:00 differed significantly among the three groups: 22.4±17.5, 17.8±14.7, and 15.8±15.3 in the DL, OLED, and LED conditions, respectively (p=0.006). Post hoc tests revealed that the mean melatonin level at 24:00 was significantly lower under LED LE than under DL (p=0.001), whereas there were no significant differences between OLED LE and DL (p=0.026) or between OLED and LED LE (p=0.086).
The melatonin onset time, delay, and suppression under the different light conditions are summarized in Figure 2 and Table 1.
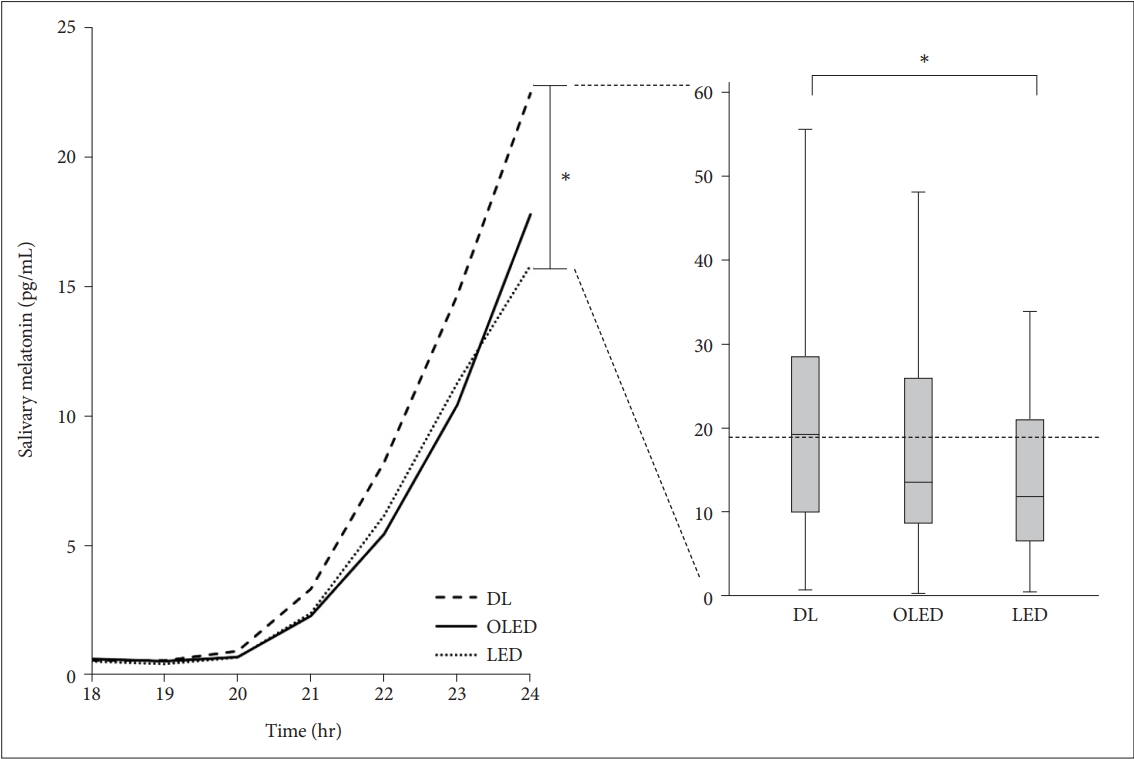
The mean melatonin level. The mean melatonin level from 18:00 to 24:00 under the three light conditions (DL, OLED, and LED). There were no significant differences in mean melatonin level among groups from 18:00 to 23:00, but there are significant differences at 24:00. The mean melatonin level at 24:00 was significantly lower in LED LE than in DL (p=0.002), whereas there were no significant differences between OLED LE and DL (p=0.068), and between OLED and LED LE (p=0.562). DL: dim light, OLED: organic light-emitting diode, LED: light-emitting diode, LE: light exposure.
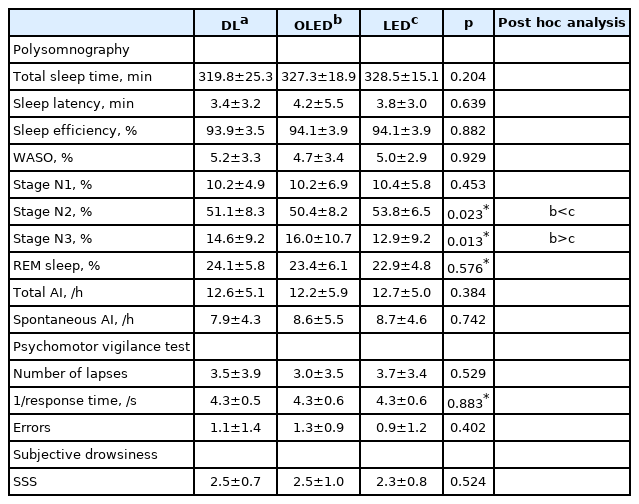
Sleep and vigilance
Most PSG parameters did not differ significantly among the three groups, but the percentage of slow wave sleep (N3) did (p=0.013). The percentage of N3 under LED LE was significantly lower than that under OLED LE (p=0.010).
In PVT, number of lapses, reaction time, and number of errors did not differ significantly among the conditions. SSS also did not differ among the conditions (p=0.524).
The sleep parameters, vigilance tests, and SSS score under the different light conditions are summarized in Table 2.
DISCUSSION
In this study, we compared the effects of exposure to OLED and LED used as room lights on melatonin profile, sleep quality, and vigilance in young adults. We found that the mean melatonin level at 24:00 under LED LE was significantly lower than that under DL, but there was no significant difference between OLED LE and DL. The percentage of N3 sleep under LED LE was lower than that under OLED LE.
Blue light is known to suppress secretion of melatonin, which can disrupt the circadian rhythm and sleeping behavior [18,19]. Brainard et al. [3] reported approximately 60% suppression of melatonin after 2 h of light at 460 nm and 12.1 μW/cm2. In another recent report, exposure to 3,000 K LED ceiling light induced statistically significant melatonin suppression compared with melatonin concentrations under a dim condition. Lightinduced melatonin AUC %change relative to the AUC under the dim condition was 30.4% in adults (41.7±4.4 years old) and 58.1% in children (8.9±2.2 years old) [20].
Thus, OLED can be a good substitute for LED because the spectrum of an OLED contains a smaller proportion of blue light, which has the greatest influence on the melanopsin in intrinsically photosensitive retinal ganglion cells. Furthermore, OLED has several benefits as a future lighting source with high efficiency and low power consumption [21,22]. In addition, OLED light panels emit diffuse light from their surfaces, which helps to reduce fatigue in the human eye. It is presumed that OLED is a human-friendly type of lighting that will disturb the circadian rhythm less than other light sources and facilitate sleep [23].
However, only a few studies have directly compared the effects of LED LE and OLED LE. Our team previously reported that early-night OLED LE exerts weaker effects on the melatonin phase delay than LED LE at a color temperature of 4,000 K [9]. There was no difference in melatonin onset between OLED and LED LE (p=0.078), however melatonin onset under LED LE was significantly delayed under DL (p=0.007), whereas under OLED LE, there was no significant delay compared to DL (p=0.287) [9]. In this study, we investigated the effects of OLED LE and LED LE on melatonin profiles at a different color temperature (3,000 K), which is widely commercialized for indoor lighting.
Our present data show that melatonin onset time did not differ significantly between OLED and LED LE. Although melatonin suppression also did not differ between OLED and LED LE, we attribute that to our inability to measure salivary melatonin level during sleep. Typically, melatonin level begins to rise significantly around 21:00 and peaks in the middle of the night, around 03:00. We measured the amount of melatonin when patients were awake from 18:00 to 24:00 and found that the amount of melatonin from 18:00 to 23:00 did not differ between the two LED groups, but there was a significant difference at 24:00. The mean melatonin level at 24:00 under LED LE was significantly lower than that under DL, but there was no significant difference between OLED LE and DL.
Our data also show that the percentage of N3 sleep was significantly lower under LED LE than under OLED LE. Stage N3 is considered as deep sleep and generally cycles frequently in the first third of the night and begins to decrease toward the second half of the night [24]. Therefore, we hypothesize that LED LE affects deep sleep early in the night. Considering that these results are linked to the lower melatonin level at 24:00 under LED LE, we propose that LED LE suppresses melatonin secretion at bedtime and prevents people from falling into deep sleep in the initial period of sleep.
When we put together the results of our previous study conducted at a 4,000 K color temperature and those of the present study at 3,000 K, we found that OLED LE caused smaller delay in melatonin onset time and less disturbed melatonin secretion than did LED LE. However, those differences between OLED and LED LE were not as distinct as we expected, possibly due to the limitations of our studies. First, we did not control subjects’ light exposure during the daytime. The participants were allowed to perform their daytime activities as usual before entering the unit. Although we monitored the amount of LE by actigraphy data from the day before the visit, a more definite difference would have been made if the daytime LE was more strictly controlled. Second, another limitation in our study is the absence of a control night, when no light pulses were conducted. Thus, the extent to which light affects sleep structure remains unclear. Although it was confirmed that the baseline circadian profile was similar using wrist actigraphy, control night data was required for accurate evaluation. Third, the amount of light actually delivered to the eyes would have been less than we had expected. We used the ceiling-mounted light panels, but participants spent most of their time reading books in the head-down position. Thus a sufficient amount of light may not have delivered to the eyes for 6.5 hours of LE. Firth, evening LE under a specific condition was performed for only one night during each session in this study. That short-term exposure might have been insufficient to detect alterations in the circadian rhythm and sleep. Finally, an illuminance of 150 lux seems not to be bright enough to interfere with circadian rhythms and sleep in young, healthy participants, even during the evening.
Although those limitations did affect our study, the present experimental setting might better reflect real lighting environments during the evening and nighttime. Despite those limitations, we did find that OLED LE had less effect on melatonin phase and sleep quality than did LED LE. Further research in a strictly controlled experimental setting with a larger number of subjects is needed to identify the significant effects of evening light sources on sleep and vigilance.
In conclusion, we suggest that evening and early-night OLED LE may induces less melatonin suppression and less disturbs deep sleep compared to LED LE. It needs further follow-up test to confirm that OLED is a suitable evening light source to minimize the harmful effects of artificial light on melatonin and sleep quality.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2020.0348.
Acknowledgements
This research was supported by Samsung Biomedical Research Institute grant (PHO0183941).
Notes
The authors have no potential conflicts of interest to disclose.
Authors’ contribution
Conceptualization: Eun Yeon Joo, Hyunjin Jo, Hea Ree Park. Data curation: Eun Yeon Joo, Hyunjin Jo, Hea Ree Park, Su Jung Choi. Formal analysis: Hyunjin Jo, Hea Ree Park. Funding acquisition: Eun Yeon Joo. Investigation: Hyunjin Jo, Hea Ree Park. Methodology: Eun Yeon Joo, Hyunjin Jo, Hea Ree Park, Soo-Youn Lee. Project administration: Eun Yeon Joo, Hyunjin Jo. Resources: Eun Yeon Joo. Software: Eun Yeon Joo, Hyunjin Jo. Supervision: Eun Yeon Joo. Validation: Eun Yeon Joo, Soo-Youn Lee, Seog Ju Kim. Writing—original draft: Hyunjin Jo. Writing—review & editing: Eun Yeon Joo, Hyunjin Jo.