Reconciliation of Two Cognitive Models in Obsessive-Compulsive Disorder: An fMRI Study
Article information
Abstract
Objective
Although cognitive models of obsessive-compulsive disorder (OCD) fall into two categories: cognitive deficit models and dysfunctional belief models, these approaches have their own ways and have hardly been reconciled. Therefore, this study aimed to investigate the potential relationships between cognitive deficit (using the Wisconsin Card Sorting Task, WCST) and dysfunctional belief (measured by scales of dysfunctional beliefs) mediated by neural activity in OCD patients.
Methods
Thirty OCD patients and 30 healthy participants performed the WCST condition and a baseline MATCH condition during the 3T-functional magnetic resonance imaging (fMRI) acquisition.
Results
Engagement of additional frontoparietal networks with poorer performance of WCST was found during the fMRI scan in OCD patients. Selected regions of interest from activated regions have positive relationships with dysfunctional beliefs and with the unacceptable thoughts symptom dimension in the OCD group.
Conclusion
Findings suggest that alteration in frontoparietal networks related to cognitive deficits can be associated with dysfunctional beliefs while performing conventional neurocognitive tasks and this association with dysfunctional beliefs may be pronounced in the unacceptable thoughts domain-dominant OCD patients.
INTRODUCTION
Since the 1980s, several cognitive models have been developed as general models of obsessive-compulsive disorder (OCD) [1]. Many researchers have conducted studies for elucidating cognitive abnormalities concerning the etiology and maintenance of OCD [2]. Broadly, cognitive models fall into two categories: cognitive deficit models, which propose that OCD is characterized by deficits in neuropsychological and information- processing functioning; and dysfunctional belief models, which postulate that OC symptoms arise from particular types of dysfunctional beliefs or appraisals [3]. However, these two approaches have their own way and have hardly been reconciled [2].
Previous studies on cognitive deficits have demonstrated that individuals with OCD show reduced performance on cognitive tasks such as executive functioning, cognitive inhibition, attention, and memory [4,5]. This line of research relies on behavioral measures such as reaction time and neuropsychological assessment [6]. In addition, these cognitive tasks have easily been used as cognitive activation paradigms in neuroimaging studies, and consequently, have greatly contributed to the development of the current neurobiological model of OCD [7]. However, cognitive deficit models have their own limitations, wherein such impairments in these cognitive functions do not fully explain clinical symptoms [8], and could be caused by the effects of anxiety or fear which characterize OCD. They also do not account for the heterogeneity of OCD symptoms or their specificity, which differs from many psychiatric disorders that present mild cognitive deficits [2].
By contrast, cognitive appraisal models propose that obsession and compulsions arise from specific types of dysfunctional beliefs and accordingly, the content of dysfunctional beliefs influences the types of OC symptoms [9,10]. The Obsessive- Compulsive Cognitions Working Group has outlined three domains of dysfunctional beliefs including 1) over-estimation of threat and inflated responsibility, 2) importance of and need to control thoughts, and 3) perfectionism and intolerance of uncertainty [11,12]. Unlike cognitive deficits, research on dysfunctional beliefs relies on self-reporting [2]. As a result, the scientific adequacy of the appraisal models has been criticized [6]. In fact, cognitive appraisal models have been developed in a way that has largely ignored the mounting body of research concerning the importance and role of neurobiological factors in OCD [1].
However, some researchers have argued that cognitive deficits, dysfunctional beliefs, and metacognitive beliefs are likely interconnected. For instance, certain beliefs, such as thoughtaction fusion (TAF) cause people to dwell on potential threats, which in turn, could foster attentional biases or memory biases to address threats [2,13]. Cognitive appraisals such as self-conscious beliefs could interfere with performance on neurocognitive tasks measuring cognitive deficits, thus perhaps leading patients with OCD to respond compulsively to achieve certainty [2,6]. However, to our knowledge, no studies have specifically elucidated that different cognitive biases could affect or interact with one another [2]. Getting a better understanding of the relationship between these two cognitive areas may help us understand how they might complement each other and offer a more comprehensive cognitive model of OCD.
The current study aimed to investigate the potential relationship between cognitive deficits, which were assessed by a computerized Wisconsin Card Sorting Test (WCST), and dysfunctional beliefs, which were measured by questionnaires. We chose the WCST as a measure of cognitive deficit because neural correlates of cognitive inflexibility or executive dysfunction have been well studied and closely relate to the current neurobiological model of OCD [7]. We hypothesized that patients with OCD, relative to healthy controls (HC), would show poorer performance on the WCST [5] and experience activation in additional areas of the brain [4,14]. Then, we tested possible correlations between brain activity in differentially activated regions and dysfunctional beliefs in patients with OCD.
METHODS
Participants
Thirty patients with OCD (27 male and 3 female) and 30 healthy volunteers (29 male and 1 female) participated in this study. All participants were right-handed and between the ages of 18 and 35 years. For determining the presence of OCD and other comorbidities, a Structured Clinical Interview for DSM-5 Disorders, Clinical Version (SCID-5-CV) was carried out. Patients were excluded if they had a current comorbid Axis I diagnosis, psychotic symptoms, mental retardation, neurological disease, or a history of head injury or medical illness with documented cognitive sequelae. For healthy participants, psychiatric interviews were conducted for the exclusion of existing psychiatric pathology, psychotic symptoms, mental retardation, neurological disease, and history of head injury or medical illness. All interviews were completed by two experienced psychiatrists (S.W.L. and S.J.L.). All participants provided written informed consent according to the procedures approved by the Institutional Review Board of Kyungpook National University Hospital (2018-04-029).
Psychological measures
Clinical symptoms were assessed using the Obsessive-Compulsive Inventory-Revised (OCI-R) [15], Dimensional Obsessive- Compulsive Scale (DOCS) [16], and Beck Depression Inventory (BDI) [17]. Dysfunctional beliefs including guilt and importance of thoughts and responsibility were measured using the Guilt Inventory and Obsessive Beliefs Questionnaire-44 (OBQ-44), respectively [18].
Computerized Wisconsin Card Sorting Test
All participants performed a modified version of the WCST during fMRI scanning. This paradigm was adapted from previous reports (Supplementary Figure 1 in the online-only Data Supplement) [19]. The task paradigm was a randomized block design, composed of the original WCST condition and a baseline MATCH condition. Instruction words were given for each condition: ‘Card’ for the WCST and ‘Identical card’ for MATCH condition. After the instruction word, participant performed the trial task following the rules of each condition and a feedback of response was shown as ‘O’ for a correct response or ‘X’ for an incorrect response on the screen. Four reference cards and one target card were presented on the screen during the trial task. The target card was characterized from the four reference cards by three categories based on color, shape, and number. The participant was asked to find the correct category by selecting one of four reference cards according to characteristics of a target card in the WCST condition, and was asked to select a card that matches the target card within the four reference cards in the MATCH condition. If the participant correctly sorts the cards four times in a row in the WCST condition, a new category is created without instructions (set shifting). In addition, participants were measured based on their perseverative error score, which is the number of errors that the participant has chosen in the same category as the previous choice.
MRI data acquisition and analyses
All structural and functional imaging data was obtained via a 3.0 Tesla 750W MRI scanner (GE Healthcare, Milwaukee, WI, USA) with a 24 channel head and neck coil. A 3D brain volume imaging sequence was used to acquire structural brain image data [repetition time (TR)=8.5 ms, echo time (TE)=3.2 ms, flip angle (FA)=12-degree, matrix size=256×256, and field of view (FOV)=25.6 cm2]. The gradient echo planer T2* weighted imaging was used for acquiring functional image data (TR= 3,000 ms, TE=30 ms, FA=90-degree, matrix size=64×64, and FOV=23.0 cm2). All functional image data were analyzed using a statistical parametric mapping toolbox (SPM12; http://www.fil.ion.ucl.ac.uk/spm), and statistical package for social sciences (SPSS25; http://www.ibm.com/analytics/spss-statistics-software). Preprocessing steps included realignment, slice timing, co-registration, normalization to the Montreal Neurological Institute (MNI) space, and smoothing (FWHM=8 mm). The motion parameter and outlier time series were detected using the artifact detection tools. The global signal change of 5 sigma and motion of 9 mm were thresholded for removing significant motion effects. The motion parameter and outlier effect were included as covariate factor in the first-level analysis. After first-level analysis was performed on individual images based on general linear model, full factorial ANOVA analysis was performed on each condition and group. The main effect of conditions was thresholded at p<0.05, false discovery rate (FDR) corrected level across whole brain (Bonferroni correction was performed for main effects including WCSTMATCH or MATCH-WCST). Additional group comparison analysis in WCST condition was conducted with thresholded at p<0.05, FDR corrected level for multiple comparisons. Regions of interest (ROIs) were created at locations of gray matter having maximum T-values on the conjunction map between main effect of condition and group comparison. After spheres (7 mm) were created at the location, the final ROIs were created by multiplying between spheres and activated regions on the conjunction map. The beta values were extracted using the REX toolbox (https://www.nitrc.org/projects/rex) on the conjunction map. Partial correlation analysis was applied between beta values and psychological measures after controlling for the effects of depression.
RESULTS
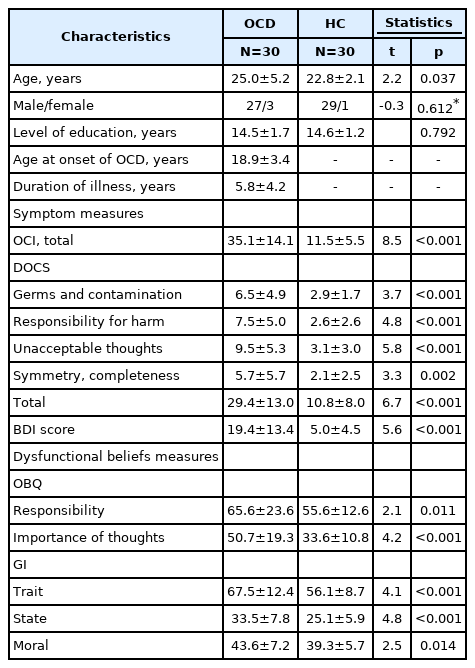
Demographic and psychological information
The demographic variables for each group are presented in Table 1. There were no significant differences between the groups in terms of sex or education. However, patients with OCD (25.0± 5.2) were older than the healthy controls (22.8±2.1). The OCD group demonstrated significantly greater scores for symptoms of OC, depression, and dysfunctional beliefs such as responsibility, importance of thoughts, feelings of guilt (all p<0.001). The OCI revealed mild to moderate levels of severity in the OC group. Eleven (37%) patients were drug naïve or had been drug-free for three months while 19 (63%) patients were taking Selective Serotonin Reuptake Inhibitors (SSRIs), mostly escitalopram (Supplementary Table 1 in the online-only Data Supplement).
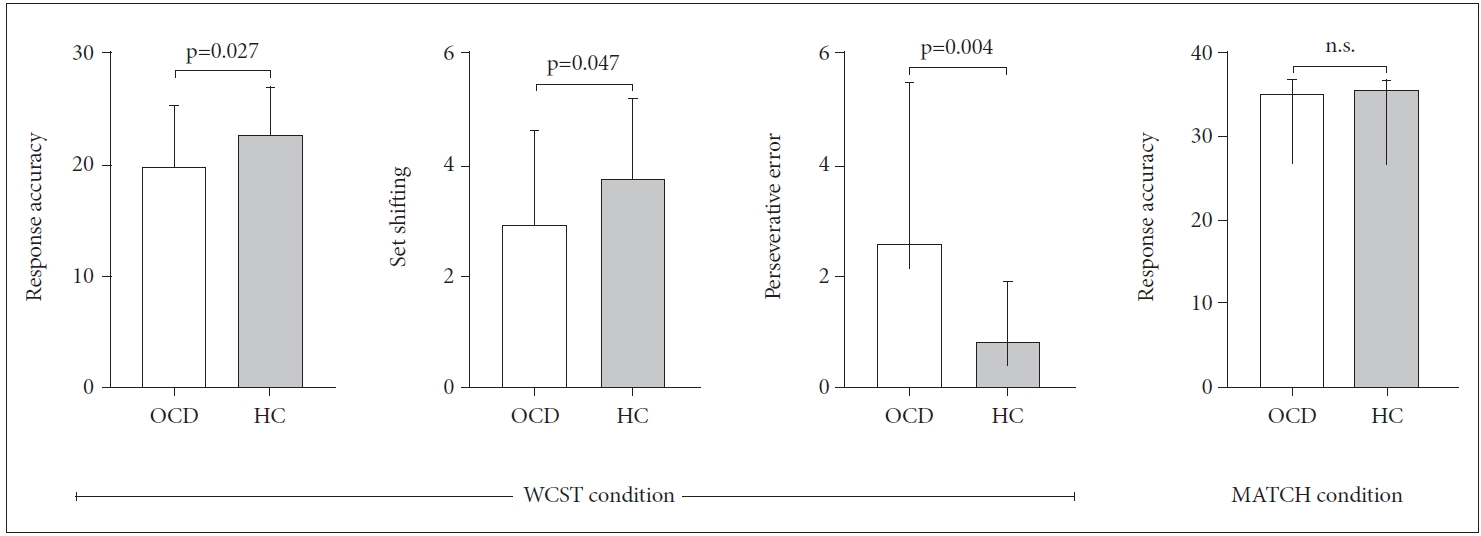
Behavioral data
Patients with OCD exhibited poorer performances than healthy individuals in the WCST condition; they had lower mean scores in numbers of response accuracy and set shifting yet higher perseverative errors in the WCST condition. However, there were no differences in accuracy in the MATCH condition (Figure 1).
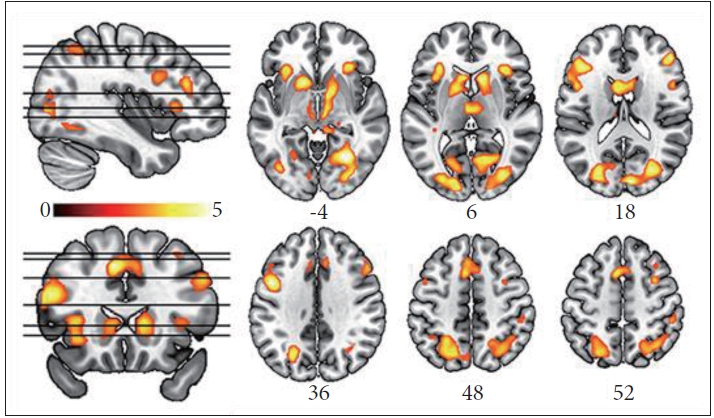
Effects of group and WCST condition in ANOVA analyses
Full factorial ANOVA analysis showed there was a significant main effect of condition and group but no interaction effect. Post-hoc analysis revealed that the main effect of condition was exclusively explained by the contrast of WCST> MATCH, in which frontoparietal network, salience network (anterior insula, caudate, putamen, and thalamus), occipital gyri, lingual gyri, brain stems, and cerebellum (FDR corrected p<0.05) (Figure 2, Supplementary Table 2 in the online-only Data Supplement) were activated. However, there were no significant brain regions in contrast of WCST<MATCH.
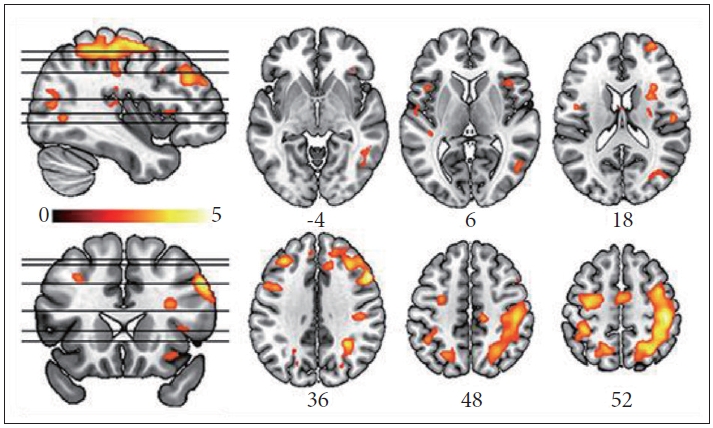
Group comparison analyses in WCST condition
Within the WCST condition, group comparison analysis revealed that patients with OCD showed higher activations mostly in frontal and parietal regions, especially a right-side dominant pattern compared to the HC group (Figure 3 and Supplementary Table 3 in the online-only Data Supplement). However, the HC group showed no greater brain activations than the OCD group. Although statistical power of group differences was decreased after controlling for the effect of depression in a group comparison analysis (uncorrected p<0.001), the initial pattern of group differences were still maintained (Supplementary Figure 2 in the online-only Data Supplement).
Brain activity vs. WCST performance, dysfunctional beliefs, and OC symptom dimensions
Conjunction map was used to select WCST related brain ROIs in OCD patients. Conjunction map between WCST> MATCH map in ANOVA analyses and OCD>HC map of WCST condition in group comparison analyses revealed activation in right medial frontal gyrus, bilateral dorsolateral prefrontal cortices, right inferior orbito-frontal gyrus, right insula, and bilateral superior and inferior parietal lobules (Figure 4A, Supplementary Table 4 in the online-only Data Supplement).
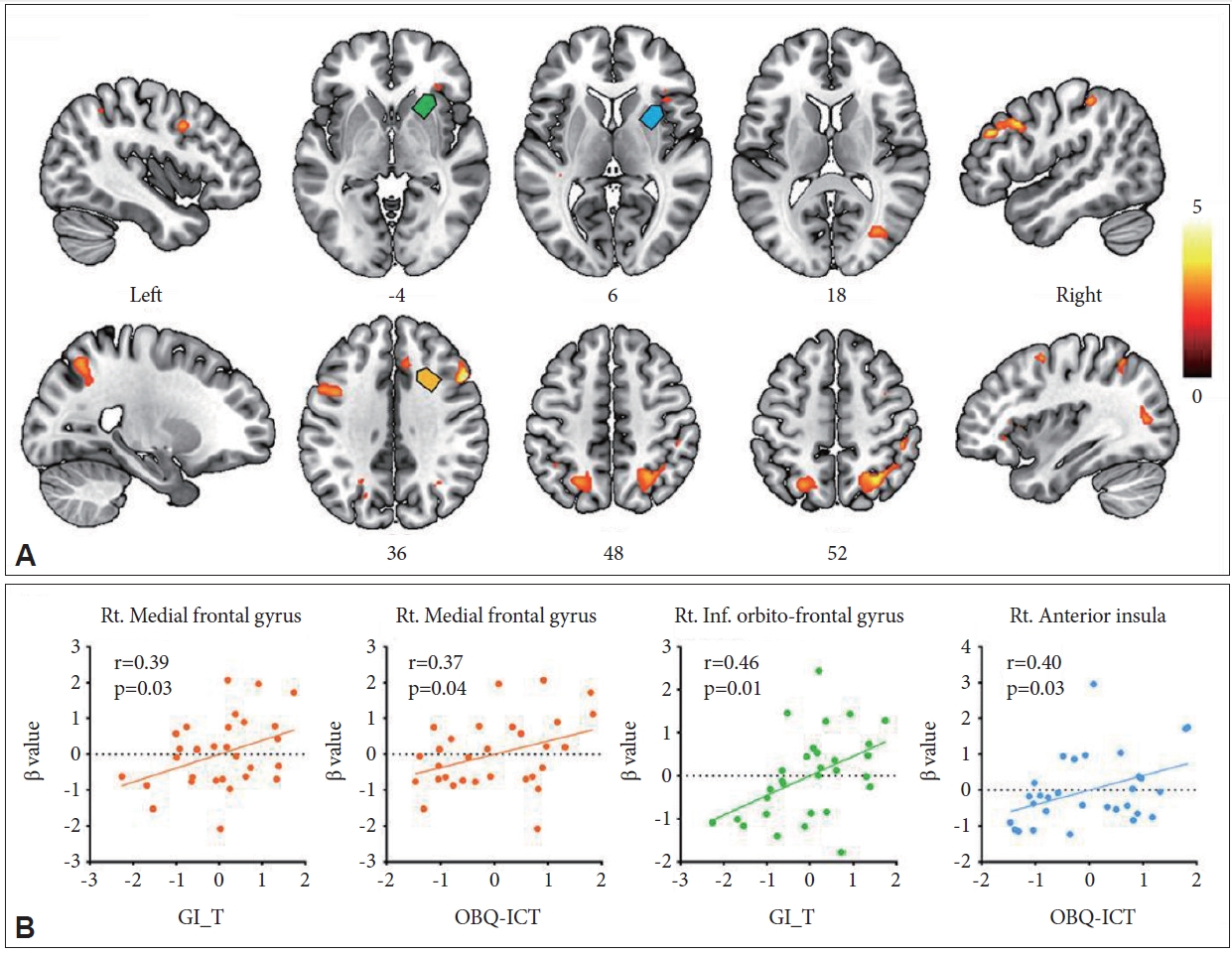
Conjunction map of condition effect (WCST>MATCH) and group effect of WCST condition (obsessive-compulsive disorder>healthy control). Activated brain regions are shown in (A) and correlations between beta activity in some of these regions (green, blue, and orange arrows for right inferior orbito-frontal gyrus, insula, and medial frontal gyrus) and dysfunctional beliefs such as guilt and importance/control of thoughts in (B). WCST: Wisconsin Card Sorting Test, GI-T: Guilt Inventory-Trait, OBQ-ICT: Obsessional Beliefs Questionnaire-Importance/control of thoughts.
Among individuals with OCD, three variables of performance on the WCST were not correlated with any brain activity in ROIs.
The subscale of importance of thought on OBQ scale had significant relationships with the right medial frontal gyrus (r=0.37, p=0.04) and anterior insula (r=0.40, p=0.03), respectively. The score of guilt trait subscale was also significantly correlated with right medial frontal gyrus (r=0.39, p=0.03) and inferior orbito-frontal gyrus (r=0.46, p=0.01), respectively (Figure 4B). However, no relationship with responsibility subscale of OBQ was found.
In terms of OC dimensions, only the unacceptable thought (pure obsession) dimension was significantly correlated with five out of ten ROIs such as bilateral DLPFC and IPL, and right SPL. However, any other relationships with the other three domains were not found (Supplementary Table 5 in the onlineonly Data Supplement).
WCST performance vs. Dysfunctional beliefs and OC symptom dimensions
Within the OCD group, three variables of performance on the WCST found no relationships with any dysfunctional belief scales and OC symptom dimensions except the only negative correlation between score of set shifting and unacceptable thought dimension (r=-0.43, p=0.02).
DISCUSSION
To the best of our knowledge, the current study is the first fMRI study to investigate the potential relationship between cognitive deficit (measured by WCST) and dysfunctional belief (measured by scales related to dysfunctional beliefs) mediated by neural activity in OCD. We found that patients with OCD recruited additional frontoparietal regions while performing the WCST task. Several selected ROIs from these additionally activated regions had positive relationships exclusively with dysfunctional beliefs such as importance of thoughts which included TAF and guilt, and with unacceptable thought dimension among four OC symptom dimensions in the OCD group. However, no ROIs showed relationships with variables of performance on the WCST.
This study revealed the engagement of additional frontoparietal network with poorer performance of WCST during MR scan in patients with OCD. First, patients in this study showed lower scores on all three variables of the WCST condition. Poorer performance on WCST, especially perseverative errors, has been confirmed in a series of meta-analysis with approximately 0.5 of effect size [20]. Second, consistent with previous fMRI studies, our cognitively complex WCST induced activation in a distributed network of brain regions, which includes not only frontoparietal network and posterior multimodal association cortices but also subcortical structures (Figure 2) [21,22]. Our between-group comparison showed additional activation mostly in frontoparietal network in the OCD group. The frontoparietal network, one major subsystem of the control system, is thought to be particularly involved in highly adaptive control processes and has extensive brain-wide connectivity [23]. Moreover, this system contains flexible hubs, which are updated according to current task demands [24]. In effect, the evidence for control system alterations has been identified in OCD [25] and compensatory frontoparietal brain activity during working memory may constitute a neurocognitive endophenotype for OCD [26].
Regarding relationships between differentially activated regions and dysfunctional beliefs in patients with OCD, activity in right medial frontal gyrus (namely, the dorsomedial prefrontal cortex; dmPFC) and anterior insula were correlated with importance of thoughts. Activation in these two regions were observed in a recent fMRI study using TAF evoking paradigm in healthy participants [27]. In particular, the right anterior insula may play a role adjusting the intensity of TAF. The anterior insula was, for example, activated more to close person than neutral person in the TAF eliciting statements. Another finding is that feelings of guilt were correlated with activity in the right dmPFC and inferior orbito-frontal gyrus (namely, ventrolateral PFC; vlPFC). Previous studies have revealed guilt-specific activations in the dmPFC and vlPFC [28,29]. The dmPFC plays a crucial role in self-referential processing [30] and mentalizing [31], whereas the vlPFC is concerned with moral decision-making; patients with OCD showed activation of this region during moral judgment [32]. Conversely, these activated regions were not correlated with any variables of WCST performance. Simply put, added activation of frontoparietal regions in patients with OCD while performing WCST did not correlate significantly with WCST scores, but rather with dysfunctional beliefs. If we did not see the relationships with dysfunctional beliefs, this study typically would conclude that additional activation of frontoparietal regions might be due to “compensation” of their cognitive dysfunction, like previous studies on cognitive dysfunction in OCD have suggested [26]. However, these findings were suggestive of another possibility that additional activation may be related not with performance of WCST itself but with dysfunctional beliefs. Patients with OCD may recruit these regions to process accessory beliefs on the performance of the WCST or the whole experiment including the scanning procedures, such that, for example, they would feel guilty if they ruined this experiment or performed tasks poorly. In turn, these additional thoughts or feelings may distract their attention from performance of the task itself and affect their performance.
Another interesting finding is that, among the four OC symptom domains, the unacceptable thoughts domain was the only one that correlated with brain activity in several ROIs exclusively in this study. Moreover, these ROIs were all lateral frontal and parietal cortices, which did not show any correlations with dysfunctional beliefs. In fact, the domain of importance/ control of thought, as measured by OBQ-44, showed the greatest correlation with obsessing symptom of OCI [33], and emerged as the only significant predictor for DOCS unacceptable thoughts scores [34]. In addition, one recent fMRI study using a TAF induction experiment observed activation in bilateral superior parietal lobules [35]. However, dysfunctional beliefs can account for all variance in the unacceptable thoughts domain (R2=0.14) [34]. This finding may explain discrepant relationships of ROIs with dysfunctional beliefs and the unacceptable thoughts domain.
Taken together, among additionally activated frontoparietal areas, medial and inferior frontal portions were related to dysfunctional beliefs while lateral frontal and parietal regions were related to the unacceptable thoughts dimension in patients with OCD. We assumed that the former may produce inner thoughts or feelings with prediction while the latter may offer a system to operate these contents under the context of metacognition (thoughts about thoughts) and self-conscious feelings (feelings about feelings). In particular, these responses may be pronounced in the pure obsessional type of OCD.
There are several limitations to our study. First, dysfunctional beliefs which showed relationships with neural activity were measured using trait-like questionnaires. We did not assess state-dependent thoughts or feelings during MRI scans. Further studies are needed to explore the direct relationship with state-dependent beliefs. Second, our study cannot confirm the direct relationship between two cognitive models since dysfunctional beliefs were only measured by questionnaires, and significance of correlation results was relatively low without multiple correction. However, we believe our results might be a cornerstone to connect two different models for understanding pathophysiology of OCD from an integrative perspective. Third, although one-third of the patients were drugfree during the experiment, the possibility that medication had an effect on our results cannot be completely excluded [36]. SSRIs can have effects on functional connectivity in OCD patients [37], and SSRI treatment can directly associated with function of frontoparietal networks during cognitive task [38]. Therefore, medication effects can modulate our fMRI results. Fourth, effects of depressive symptoms were not clearly excluded in our results. Although the patterns of group differences were maintained at an uncorrected level, several activations of group differences were attenuated after adjusting for depressive symptoms. Fifth, a male-dominant sample may raise gender issues in this study. However, previous literature has found little evidence for differences in obsessive beliefs between the sexes, suggesting that these beliefs may not be dependent on demographic characteristics [39]. Lastly, it should be noted that the WCST and MATCH condition as a whole was included in the analysis whether individual trial was correct or not. This is due to several reasons: First, our fMRI task design was block design. Second, WCST inevitably has incorrect trials and responses of incorrect trials can affect followed trials. Third, individual subjects had different correct and incorrect trials, thus amounts of time and data for analysis were inconsistent across subjects.
In conclusion, this fMRI study found that additional activation of frontoparietal regions in patients with OCD while performing the WCST did not correlate with WCST scores, but rather with dysfunctional beliefs and the unacceptable thoughts domain of OCD. These findings suggest that cognitive errors and cognitive deficits may be interrelated in the brain even when performing conventional neurocognitive tasks and coinvolvement of cognitive errors may be pronounced in the unacceptable thoughts domain-dominant OCD patients.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2020.0347.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (NRF-2018R1A2B6007374).
Notes
The authors have no potential conflicts of interest to disclose.
Authors’ contribution
Conceptualization: Sang Won Lee, Seung Jae Lee. Data curation: Seungho Kim, Hyunsil Cha, Eunji Kim, Sang Won Lee. Formal analysis: Seungho Kim, Hyunsil Cha, Eunji Kim. Funding acquisition: Seung Jae Lee. Investigation: Seung Jae Lee. Methodology: Seungho Kim, Sang Won Lee. Project administration: Seung Jae Lee. Resources: Yongmin Chang, Seung Jae Lee. Software: Seungho Kim, Sang Won Lee. Supervision: Yongmin Chang, Seung Jae Lee. Validation: Yongmin Chang, Seung Jae Lee. Visualization: Seungho Kim, Writing—original draft: Seungho Kim, Sang Won Lee, Seung Jae Lee. Writing—review & editing: Yongmin Chang, Seung Jae Lee, Seungho Kim, Sang Won Lee.