A Call for a Rational Polypharmacy Policy: International Insights From Psychiatrists
Article information
Abstract
Objective
Recently, rational polypharmacy approaches have been proposed, regardless of the lower risk and cost of monotherapy. Considering monotherapy as first-line treatment and polypharmacy as rational treatment, a balanced attitude toward polypharmacy is recommended. However, the high prevalence of polypharmacy led the Japanese government to establish a polypharmacy reduction policy. Based on this, the association between the policy and psychiatrists’ attitude toward polypharmacy has been under debate.
Methods
We developed an original questionnaire about Psychiatrists’ attitudes toward polypharmacy (PAP). We compared the PAP scores with the treatment decision-making in clinical case vignettes. Multiple regression analyses were performed to quantify associations of explanatory variables including policy factors and PAP scores. The anonymous questionnaires were administered to psychiatrists worldwide.
Results
The study included 347 psychiatrists from 34 countries. Decision-making toward polypharmacy was associated with high PAP scores. Multiple regression analysis revealed that low PAP scores were associated with the policy factor (β=-0.20, p=0.004). The culture in Korea was associated with high PAP scores (β=0.34, p<0.001), whereas the culture in India and Nepal were associated with low scores (β=-0.15, p=0.01, and β=-0.17, p=0.006, respectively).
Conclusion
Policy on polypharmacy may influence psychiatrists’ decision-making. Thus, policies considering rational polypharmacy should be established.
INTRODUCTION
In the field of psychiatry, polypharmacy refers to the prescription of multiple psychotropic drugs to one patient. Polypharmacy is of concern because it can increase the risk of adverse effects and mortality rate and reduce medication adherence and patients’ quality of life [1]. In addition, polypharmacy imposes a large economic burden. Although most practice guidelines recommend monotherapy as a first-line treatment, polypharmacy has become common practice. The widespread implementation of polypharmacy prompted collaborative research to evaluate the prescription patterns of psychotropic drugs in Asia (Research on Asian Psychotropic Prescription Pattern, REAP) in 2001 [2]. The study revealed a high prevalence of polypharmacy in Japan. For example, >50% of patients with schizophrenia used ≥2 psychotropic drugs [3]. This high prevalence of polypharmacy led the Japanese government to establish a polypharmacy reduction policy, and polypharmacy limitations have been adopted in a stepwise manner since the medical fee revision in 2012 [4]. Initially, the reduction of the national fee schedule was based on prescriptions of ≥3 anxiolytics or ≥3 hypnotics, and the list of prescriptions which apply to this reduction policy has been updated and extended every two years until 2018. Since the introduction of the polypharmacy reduction policy, polypharmacy is less frequently observed [4].
Considering the decreased polypharmacy rate in Japan, some psychiatrists doubt whether the decrease in polypharmacy rate improved the clinical practice of psychiatry, especially when “rational polypharmacy” is taken into consideration. “Rational polypharmacy” has recently been proposed by several reports, regardless of the low risk and lower cost of monotherapy [5-7]. One example of “rational polypharmacy” pertains to cross-titration: when switching from one medication to another, the overlap of the two medications is inevitable during a certain period. Another example of “rational polypharmacy” arises when the benefits of polypharmacy are supported by evidence. For example, in a nationwide cohort study in Finland that collected clinical data from >62,000 patients with schizophrenia, within-individual analyses minimizing selection bias were conducted [8]. The analyses revealed that using clozapine plus aripiprazole combination therapy yielded the lowest risk of psychiatric rehospitalization and was associated with a 14%–23% lower risk of rehospitalization relative to the use of clozapine monotherapy. The specific polypharmacy patterns supported by this report would be considered “rational polypharmacy.”
Even when a specific polypharmacy pattern is not supported by previous evidence, polypharmacy can be regarded as rational. In terms of clinical practice, psychiatrists tend to choose the most appropriate treatment strategy for each patient based on their individual circumstances, not big data. When evidence-based monotherapies with optimal dosages and enough duration are ineffective, non-evidence-based polypharmacy prescription can be attempted as a last resort. In this case, careful studies on individual patients (i.e., n=1) should be performed. Preskorn and Lacey [6] proposed criteria for rational polypharmacy in psychiatry and guidelines for using a combination of medication based on an n=1 trial in clinical practice. If the criteria and guidelines are followed, administering polypharmacy to the patient would be considered rational. In this way, polypharmacy in psychiatry is rational in some settings. However, in the context of “rational polypharmacy,” the negative attitudes of psychiatrists toward polypharmacy might interfere with selecting the best treatment for an individual patient. Considering both monotherapies as a first-line treatment and polypharmacy as a rational treatment, a balanced attitude toward polypharmacy should be recommended.
Aims of the study
To test the hypothesis that public policies, such as laws, rules, and regulations could distort the balanced attitude toward polypharmacy among psychiatrists, we first developed an original questionnaire to evaluate Psychiatrists’ attitudes toward polypharmacy (PAP). Then, the correlation between the results of the original questionnaire and treatment decision-making toward polypharmacy evaluated using the case vignette-based questionnaire was analyzed to assess PAP in a way that better aligns with real-world clinical practice. Finally, we examined the association between PAP scores and the five factors reported to be associated with polypharmacy across countries. To the best of our knowledge, this is the first international survey about both psychiatrists’ attitudes toward polypharmacy and treatment decision-making using case vignettes.
METHODS
In this study, we created a self-report questionnaire for psychiatrists practicing in different countries. The contents of the questionnaire are described in the following paragraph. The survey was developed in Japanese before being translated into English using forward-backward translation. The Japanese or English questionnaire was distributed both online and offline using the psychiatrists’ networks, such as the consortium of REAP, Early Career Section of the World Psychiatric Association, and the Japan Young Psychiatrists Organization. All participants were requested to complete the questionnaire within the survey period between June 1, 2018 and October 31, 2019.
Questionnaire
The questionnaire was composed of the following three sections: a PAP questionnaire, a case vignette-based questionnaire, and a questionnaire covering factors related to polypharmacy. The details of each part are described below.
Psychiatrists’ attitudes toward polypharmacy questionnaire
The questionnaire items were developed based on published research on polypharmacy and expert opinion from several psychiatrists who have been engaged in clinical research on polypharmacy. The questionnaire asking “What do you think about polypharmacy?” was composed of the following four items: 1) depending on the situation, it can be an important treatment option; 2) absolutely needs to be avoided; 3) inevitable in severe cases; and 4) are you careful to avoid polypharmacy in your usual clinical practice? The responses were recorded on a 5-point Likert scale, where a score of 1 indicated “do not agree at all” and a score of 5 indicated “fully agree.” The sum of the scores was obtained by adding the scores of each item after reverse scoring for items 2 and 4. A higher score indicated a more positive attitude of the psychiatrist toward polypharmacy.
Case vignette
“Typical” anonymized cases of patients with schizophrenia were described by professional psychiatrists with extensive experience and used to draft a fictitious case vignette. After confirmation and modification by mental health professionals, including psychiatrists and psychologists, a case vignette questionnaire based on two patients with schizophrenia was developed in Japanese. The Japanese case vignette was translated into English using forward-backward translation (Table 1). Using the case vignette, treatment decision-making, including polypharmacy and non-polypharmacy (e.g., electroconvulsive therapy), were evaluated.
Questionnaire covering factors related to polypharmacy
Ghaemi [9] suggested that five factors were associated with the rise of polypharmacy: scientific, clinical, economic, political, and cultural factors. Based on these five factors, we designed our questions in this fashion:
1) With respect to the scientific factor, clinical evidence on psychotropic medications is known to contribute to polypharmacy. Thus, we added a question on the personal importance of prescription guidelines on psychotropic drugs and recorded responses on a 6-point Likert scale with 1=“no use,” 2=“useful, but not important,” and 6=“useful, very important.”
2) As for the clinical factor, the association between standardized diagnostic criteria and polypharmacy has been suggested as the criteria sometimes result in overlapping diagnoses, which can lead to polypharmacy [7,9]. In our study, we asked to what extent responders were committed or devoted to the diagnosis of a psychiatric disease using the ICD-10 or DSM-5 and recorded the responses on a 6-point Likert scale with 1=“small extent” and 6=“large extent.”
3) Considering our study’s hypothesis, the policy factor indicating “public policy,” such as laws, rules, and regulations, was evaluated by a question asking about the importance of a limitation on the use of psychotropic drugs using a 6-point Likert scale: 1=“there is no limitation,” 2=“there is a limitation, but it is not important,” and 6=“there is a limitation, and it is very important.”
4) The economic factor was assessed by asking a question about the extent of prescription of psychotropic drugs covered financially by the government or national insurance coverage using a 3-point Likert scale to record responses with 1=“many restrictions,” 2=“a few exceptions,” and 3=“100% covered.”
5) The cultural factor related to the hypothesis that a preference for pharmacological treatments tends to differ across countries. Thus, a question on nationality was added.
Statistical analyses
Normality tests (skewness, kurtosis, and boxplots) were performed to determine if the PAP scores had a normal distribution. When the PAP scores in each country were not normally distributed, the Kruskal-Wallis H test and post hoc Dunn’s pairwise comparison with Bonferroni correction were used to evaluate differences in PAP scores between major countries. Correlations between the PAP scores and treatment decision-making in the case vignette were evaluated using Spearman’s correlation coefficient. Finally, multiple linear regression analyses were then conducted to assess whether known factors related to polypharmacy predicted the PAP scores; the PAP score was entered as an independent variable, whereas the answers on known four factors related to polypharmacy, except for the cultural factor (i.e., scientific, clinical, economic, and policy factors), were entered as dependent variables. With respect to the cultural factor, dummy variables for major countries were added, which at least took some account of cultural differences in countries. The significance level was set at 0.05 for all statistical analyses. Stata 15.1 (Stata Corp., College Station, TX, USA) software was used to perform the statistical analyses.
Study approval
This study was performed in accordance with the Declaration of Helsinki and was approved by Kyushu University (IRB approval number: 30-251). All subjects were informed that participation was completely voluntary and return of the anonymous questionnaire implied consent.
RESULTS
Participants
A total of 347 psychiatrists from 34 countries participated in our study (Table 2). The six countries with the highest number of participants were Japan, Korea, Nepal, Iran, Thailand, and India (n=65, 54, 49, 40, 33, and 19, respectively). The average age of participants was 36.7 years (standard deviation [SD]=8.6), and the average amount of clinical experience was 8.5 years (SD=7.8). Sixty-one percent of participants were male (n=212). The average PAP score was 12.6 (SD=3.0).
Psychiatrists’ attitudes toward polypharmacy scores and treatment decision-making toward polypharmacy across countries
The PAP scores and treatment decision-making toward polypharmacy in case vignettes are plotted across countries in Figures 1 and 2. Although a normal distribution was confirmed for the overall PAP scores, a normal distribution was not confirmed for the PAP scores in each country. A significant difference in PAP scores between major countries was revealed by the Kruskal-Wallis H test (χ2-value=71, degrees of freedom=6, and p=0.0001). The post hoc Dunn’s pairwise comparison with Bonferroni correction revealed significant differences between Korea and all other countries, as well as between Iran and the other major countries except for Thailand (Table 3).
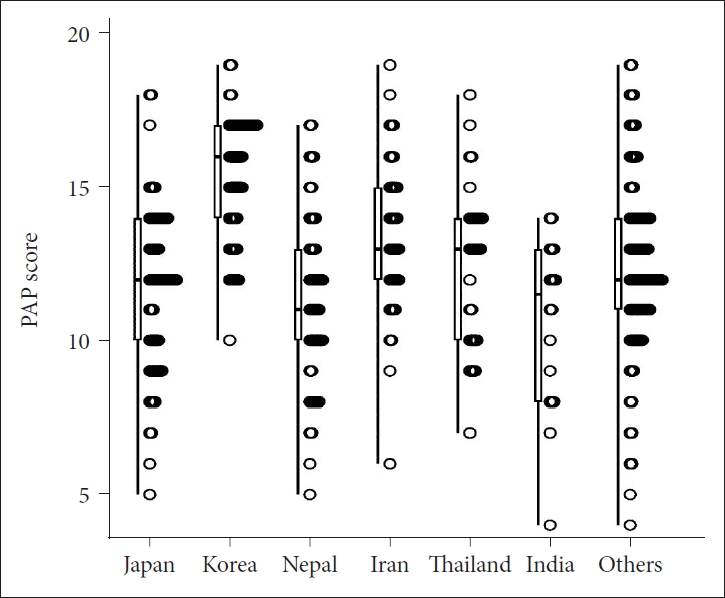
Psychiatrists’ attitudes toward polypharmacy (PAP) scores across countries. PAP scores are plotted across six major countries.
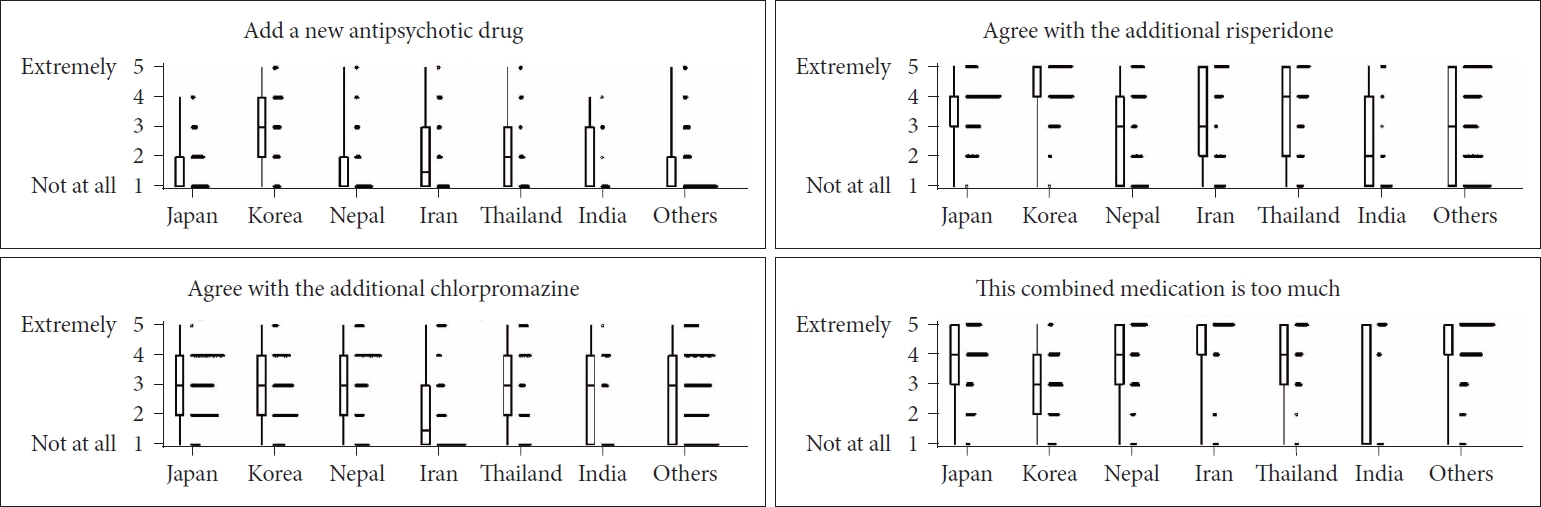
Treatment decision-making toward polypharmacy across countries. Treatment decision-making toward polypharmacy in the case vignettes is plotted across six major countries.
Correlation between Psychiatrists’ attitudes toward polypharmacy scores and treatment decision-making in the case vignettes
The PAP scores reflected the positive decision-making toward polypharmacy in the case vignettes; item A-4 (How likely are you to add a new antipsychotic drug to his present medication?), item B-1 (How likely are you to agree with the additional risperidone at 4 mg/day?), and item B-3 (How likely are you to think that this three-type-combined medication is too much?) were correlated with the PAP scores (Spearman rho=0.28, 0.21, and -0.29; p<0.0001, p=0.00001, and p<0.0001; respectively). The other treatment decision-making parameters (e.g., electroconvulsive therapy, dosage adjustment, or replacement of already taken psychotics) were not correlated with the PAP scores (Table 4). The PAP scores and treatment decision-making toward polypharmacy in the case vignettes are plotted in Figure 3.
Results of multiple linear regression analyses on predicting the Psychiatrists’ attitudes toward polypharmacy scores
The results of the multiple regression analyses performed to predict the PAP scores are presented in Table 5. A significant association was found (F[10, 277]=8.88, p<0.001), with an R2 of 0.243. The policy factor was significantly negatively predicted by the PAP scores (β=-0.20, p=0.004). Regarding the cultural factor among the six major countries, culture in Korea was associated with higher PAP scores (β=0.34, p<0.001), whereas culture in India and Nepal was associated with lower scores (β=-0.15, p=0.01, and β=-0.17, p=0.006, respectively). When a dummy variable for sex (male=1, female=2) and the years of clinical experience were also introduced as independent variables, similar results were obtained (Table 6).
DISCUSSION
We developed an original questionnaire to evaluate attitudes toward polypharmacy among psychiatrists. The PAP scores reflected decision-making toward polypharmacy in clinical case vignettes. The PAP scores differed among psychiatrists from different countries: in Korea, high PAP scores were found among psychiatrists. Beyond these differences between countries (cultural factor), the policy factor also predicted PAP scores.
In our study, a policy factor was significantly associated with relatively lower PAP scores. This association between the limitation on the use of psychotropic drugs and lower PAP scores is compatible with the hypothesis that the Japanese polypharmacy reduction policy has influenced psychiatrists’ attitudes and reduced the prevalence of polypharmacy. To the best of our knowledge, this is the first report indicating the effect of policy on PAP, although the effects of policy on attitudes toward mental disorders [10] and smoking behavior [11] have been reported previously.
In the context of the effects of a policy on psychiatrists’ attitudes and decision-making toward polypharmacy, the content of the policy is important. In Japan, polypharmacy limitations have been placed as follows [4]: 1) in 2012, a reduction of the medical fee reimbursement was introduced for prescriptions of three or more anxiolytics or three or more hypnotics; 2) in 2014, the prescription of four or more antidepressants or four or more antipsychotics was added as a condition for this reduction; 3) in 2016, the rule was strengthened, and prescription of three or more anxiolytics, hypnotics, antidepressants, or antipsychotics was targeted for reimbursement reduction; and 4) in 2018, the prescription of four or more anxiolytics and hypnotics was added as a condition to this reduction scheme. Evidently, this Japanese policy has focused on the mere number of medications, lacking consideration for medical conditions or the severity of mental disorders. This sweeping policy can hamper the rational polypharmacy that is required for specific settings. Furthermore, it can lead to psychiatrists refusing the medical examination of patients with severe mental disorders because they have higher risks and likelihood of polypharmacy and a subsequent reduction in income. This policy-induced decline in medical care should be avoided. By contrast, the policy should be established for the improvement of medical care, which is only possible when the reduction policy is established thoughtfully based on scientific and empirical evidence, perspectives from patients, psychiatrists’ expertise, and constructive debate.
In addition to the policy factor, we found that the cultural factor partially influenced psychiatrists’ attitudes, which was evaluated using dummy variables for major countries. Indian and Nepalese cultures were associated with lower PAP scores (i.e., negative attitudes toward polypharmacy), whereas Korean culture was associated with higher PAP scores (i.e., positive attitudes toward polypharmacy). Some of these cultural differences may be caused by religion. For example, according to a book on religion and medicine [12], traditional Hindus are reluctant to go to the hospital and take medications because they believe in the existence of three body humors, and an imbalance in body humors is believed to cause illnesses. These kinds of religious beliefs possibly influence attitudes toward polypharmacy, although further research is required to confirm the effect of religion on the psychiatrist’s attitude.
For future studies, the association between psychiatrists’ attitudes and the time trend of the polypharmacy prevalence rate should be considered. In Japan, a high prevalence of polypharmacy (i.e., more than 50%) has been reported even now. However, in our study, the PAP scores indicating psychiatrists’ attitudes toward polypharmacy were not high; by contrast, it was lower than the average score within our study. These apparently paradoxical facts are compatible with the time trend of polypharmacy in Japan. According to the comparison of polypharmacy rates across countries in 2001, 2004, 2009, and 2016 [3], the rate has been continuously decreasing only in Japan; however, Japan was one of the top three countries with the highest polypharmacy rates among 15 countries in 2016. This sequential reduction in polypharmacy could be attributable to the relatively negative attitudes toward polypharmacy, as indicated in our study. The time trend of polypharmacy rates also indicated that the prevalence rate of polypharmacy is continuously increasing only in Korea across the four time points examined in our previous study [3]. This sequential increase in polypharmacy would be related to the positive attitudes toward polypharmacy among Korean psychiatrists. Considering the similarity of PAP scores to the time trend of polypharmacy rate, the PAP scores can be used as a marker to predict the time course of polypharmacy prevalence, although further studies are required.
In our study, PAP were assessed, although we focused on the prevalence rate of polypharmacy in collaborative research on the prescription patterns of psychotropic drugs in Asia (REAP). Compared to the prevalence rate, it would be easier to interpret the results about psychiatrists’ attitudes across countries as the polypharmacy rate is more susceptible to local factors, such as drug approval, over-the-counter drugs (non-prescription drugs), and the barriers to psychiatric treatments. Regarding drug approval, for example, in Japan, brexpiprazole is approved at 2 mg/day during the maintenance period for patients with schizophrenia [13], whereas 2–4 mg is approved by the United States Food and Drug Administration [14]. This difference in the approved drug dosage may lead to polypharmacy. For a patient whose appropriate dosage of brexpiprazole is 4 mg, 2 mg brexpiprazole is not effective; thus, more than one type of psychotic medication needs to be prescribed in Japan. Regarding over-the-counter drugs, the types and dosages of non-prescription drugs differ among countries. Drugs without prescriptions are not usually included in the prescription survey, which makes it difficult to compare the prevalence of polypharmacy across countries. Furthermore, barriers to psychiatric treatments can delay seeking care and treatment, potentially leading to the deterioration of mental conditions. If only severe cases are treated because of barriers in a country, the prevalence of polypharmacy will increase. In this way, the prevalence rate of polypharmacy in psychiatry is influenced by both local medical factors and PAP.
PAP have been assessed in several reports, although these are much fewer than studies on polypharmacy rates. Previous surveys on psychiatrists’ attitudes were conducted in America, Japan, and Nigeria and have shown similarities in the PAP among both high and low polypharmacy prescribers [15-17]. Contrary to these previous results, our results indicated a significant association between attitude toward polypharmacy and treatment decision-making toward polypharmacy using case vignettes. This discrepancy between our results and previous findings could be attributed to differences in evaluating the following two aspects: 1) attitudes toward polypharmacy and 2) treatment decision-making toward polypharmacy. In previous studies, psychiatrists’ attitudes were evaluated based on the levels of concerns toward polypharmacy and the reasons for justifying or being against polypharmacy, whereas treatment decision-making toward polypharmacy was evaluated by the self-reported percentage of patients on polypharmacy. In our present study, psychiatrists’ attitudes were evaluated using original questions based on expert opinion, which does not target justification or concerns about polypharmacy because we thought that common knowledge about the advantages and disadvantages of polypharmacy could distort the answers focusing on concerns and justification. In addition, in our study, treatment decision-making toward polypharmacy was evaluated using clinical case vignettes, which are useful tools for measuring health professionals’ attitudes [18].
This study has several limitations. First, there may be an inconsistency between the real attitudes and attitudes recorded in our survey. PAP were evaluated using self-reported questionnaires, and their scores were validated using the results of the attitudes in response to case vignettes. It is possible that the self-reported answers were distorted by some factors, such as social desirability bias. In addition, the attitudes in response to a case vignette cannot completely and accurately reflect actual attitudes in clinical settings. Second, the study results cannot be generalized to psychiatrists in each country. Due to the process of distributing questionnaires and the voluntariness of participation, participants in our study may have had more interest in polypharmacy than the average psychiatrist in the country (self-selection bias). Finally, only five factors (i.e., scientific, clinical, economic, policy, and cultural factors), already known to be related to polypharmacy, were introduced as one question per factor in our study. Whether other factors, such as socioeconomic status, religion, race, hospital type, and the professional field, have an impact on the attitudes toward polypharmacy cannot be evaluated, although we have discussed the possible impact of religion.
In conclusion, we developed a questionnaire that reflected treatment decision-making toward polypharmacy among psychiatrists. Based on this questionnaire, international comparison and multiple regression analyses were conducted. Our results suggested that psychiatrists’ attitudes may be affected by cultural differences in each country. Beyond these cultural differences, the policy factor significantly influenced psychiatrists’ attitudes. Considering its effect on treatment decision-making, thoughtful policies on polypharmacy considering “rational polypharmacy” should be established. We also discussed the possibility that the PAP scores may predict the future prevalence rate of polypharmacy. If psychiatrists’ attitudes are useful for predicting future prevalence rates, they may be useful for better policymaking. Further research is warranted to assess whether predictions can be made using PAP scores.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Seon-Cheol Park, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Naotaka Shinfuku, Takahiro A. Kato. Data curation: Yukako Nakagami, Kohei Hayakawa, Toru Horinouchi, Victor Pereira-Sanchez, Marcus P.J. Tan, Seon Cheol Park, Yong Chon Park, Seok Woo Moon, Tae Young Choi, Ajit Avasthi, Sandeep Grover, Roy Abraham Kallivayalil, Yugesh Rai, Mohammadreza Shalbafan, Pavita Chongsuksiri, Pichet Udomratn, Samudra T. Kathriarachchi, Yu-Tao Xiang, Kang Sim, Afzal Javed, Mian-Yoon Chong, Chay-Hoon Tan, Shih-Ku Lin, Toshiya Inada, Toshiya Murai. Formal analysis, Software, and Visualization: Yukako Nakagami, Kohei Hayakawa, Takahiro A. Kato. Funding acquisition: Yukako Nakagami, Takahiro A. Kato. Project administration, Investigation, Methodology, and Resources: Naotaka Shinfuku, Takahiro A. Kato. Supervision and Validation: Shigenobu Kanba, Norman Sartorius, Naotaka Shinfuku, Takahiro A. Kato. Writing—original draft: Yukako Nakagami, Kohei Hayakawa, Takahiro A. Kato. Writing—review & editing: Toru Horinouchi, Victor Pereira-Sanchez, Marcus P.J. Tan, Seon Cheol Park, Yong Chon Park, Seok Woo Moon, Tae Young Choi, Ajit Avasthi, Sandeep Grover, Roy Abraham Kallivayalil, Yugesh Rai, Mohammadreza Shalbafan, Pavita Chongsuksiri, Pichet Udomratn, Samudra T. Kathriarachchi, Yu-Tao Xiang, Kang Sim, Afzal Javed, Mian-Yoon Chong, Chay-Hoon Tan, Shih-Ku Lin, Toshiya Inada, Toshiya Murai, Shigenobu Kanba, Norman Sartorius, Naotaka Shinfuku.
Funding Statement
This work was supported by the Japan Agency for Medical Research and Development (AMED) (Syogaisya-Taisaku-Sogo-Kenkyu-KaihatsuJigyo: JP17dk0307047, JP19dk0307073, and JP18dk0307075, and Yugo-N: JP19dm0107095), and KAKENHI - the Japan Society for the Promotion of Science (JP15K15431, JP16H06403, JP16H03741, and JP19K21591 to T. A.K.; and JP20K16647 to Y.N.).
Acknowledgements
The authors would like to thank all the psychiatrists involved in this study for their contributions.







