Mediation Effect of Insomnia Symptoms on Relation Between Stress and Quality of Life
Article information
Abstract
Objective
Among various causes of insomnia, stress is the most common and representative cause. Insomnia is also known to negatively affect the quality of life (QoL). The objective of this study was to explore the effect of stress on QoL and the mediating role of insomnia symptoms in the relationship between stress and QoL.
Methods
In this study, the mediating effect of insomnia symptoms on the relationship between stress and QoL was analyzed by enrolling 3,714 participants from the Ansung and Ansan cohorts of the Korea Association Resource project from 2001 to 2004. These cohort participants were asked about how much they felt stressed during their everyday life. Insomnia symptoms were evaluated by asking participants whether they had trouble sleeping such as difficulty in falling asleep, disrupted sleep, and early morning awakening due to the lack of a validated questionnaire for this cohort. QoL was evaluated using the World Health Organization QoL Scale Brief Version.
Results
In total, stress was positively associated with insomnia symptoms, which in turn predicted QoL. The same result could be derived from subgroup analysis according to sex, and it was confirmed that insomnia symptoms acted as a mediating factor more significantly in female than in male.
Conclusion
In this study, insomnia symptoms were confirmed to act as a significant mediating factor between stress and QoL, suggesting that insomnia symptoms should be actively identified and controlled to alleviate the negative effect of stress on QoL in clinical practice.
INTRODUCTION
Many countries are making socioeconomic investments to improve people’s quality of life (QoL). In the past, humans regarded material abundance related to survival and safety as necessary. However, due to economic development, there is a growing trend of emphasizing mentally satisfying lives rather than survival and security issues. The World Health Organization (WHO) defines the QoL as an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns [1]. Many factors can influence the QoL of an individual. Variables identified to be able to predict the QoL of young adults include social support and income. Marital status is a significant predictor for middle-aged people while income is an important predictor for older adults [2]. Older people are also more satisfied with life than younger people [3]. People with more severe depressive and irritability symptoms have lower QoL [4]. In particular, stress is closely related to QoL because perceptions of the world can induce negative emotions and affect human health and life by changing the autonomic nervous system and the endocrine system [5].
Stress is defined as a response to change to maintain the state of stability or homology that the body has maintained against stimulus that can break the body’s mental and physical balance and stability [6]. Stress is a feeling produced by uncontrollable events or noxious stimuli. Selye [6] in 1956 has defined stress as a nonspecific response of the body to any demand. A previous study has found that high levels of stress in general are closely related to poor QoL of college students [7]. A study of psychiatric outpatients has also reported that even after psychiatric disorders are corrected, stress can deteriorate the QoL [8].
Although previous studies have noted a direct effect of stress on QoL, mediating effects of various physiological responses on stress should also be considered. Among them, insomnia can be a variable that mediates the relationship between stress and QoL. People who do not sleep well show the highest levels of sympathetic arousal and high levels of glucocorticoids in their bloodstream [9]. They also show increased adrenocorticotropic hormone (ACTH) levels and cortisol secretion for 24 hours [10]. Therefore, a lot of stress may lead to insomnia. Sleep occupies around one-third of human life. It restores functions of the body and muscles consumed during the day and regenerates vital energy. Thus, sleep plays an important role in maintaining physical function, memory consolidation, and mental health [11].
Insomnia is characterized by difficulty in initiating or maintaining sleep, frequent awakenings or problems returning to sleep after awakening, and early-morning awakening with inability to return to sleep [12]. Insomnia can predict psychiatric disorders such as depression, anxiety disorder, and alcohol abuse or dependence [13]. It is well known that stress can induce physiological arousal, leading to insomnia [14]. Hicks and Garcia [15] have studied sleep time and stress levels for four months and found that sleep time is decreased during periods of high stress but increased during periods of low stress. Overall, higher daily stress levels are associated with shorter sleep duration and higher cortisol levels [16]. Thus, stress can cause insomnia and insomnia can affect QoL. According to previous studies, stress can cause insomnia that is likely to be closely related to physical and mental QoL. Perhaps because stress goes through a chain-mediated process in which numerous factors appear before the QoL is affected. Stress can cause physiological and psychological arousal, which can lead to sleep disturbance [14]. In particular, insomnia can negatively affect QoL and daily functioning [17]. In this regard, insomnia might play a sufficient role as a mediator between stress and QoL. The process of its effect can be identified and understood through analysis that takes insomnia into account.
The objective of this study was to explore the effect of stress on QoL and the mediating role of insomnia in this relationship. Everyone experiences stress. Therefore, if we can analyze effects of stress on QoL and mediating effects of insomnia on the relationship between stress and QoL in the general population, it will be possible to understand more reality-based phenomena rather than those in serious diseases or specific groups. Based on a community-based cohort sample constructed from the general population, we analyzed the effect of stress on QoL using stress, insomnia symptoms, and QoL as variables and how insomnia symptoms could work as a mediating factor affecting the relationship between stress and QoL. We also examined the difference in the mediating effect according to subgroup analysis of sex, age, and income.
METHODS
Study population
We obtained data from Ansung and Ansan cohorts of the Korea Association Resource (KARE) project, which were investigated as part of the Korea Genome Epidemiology Study (KoGES) [18]. In this cohort, a total of 7,515 people aged 40 to 69 years were enrolled from 2001 to 2004. Various epidemiologic and health-related information such as demographic information, personal and family medical histories, health-related conditions, lifestyle, stress, and mood state, QoL, and sleep-related symptoms were collected. Among them, samples with responses to all evaluations of stress, insomnia, and QoL were selected and a cohort sample of 3,714 participants was finally obtained for analysis. The KoGES project obtained prior basic written informed consent and ethics committee approval for the cohort study. We also received Institutional Review Board of the Korea University Anam Hospital (IRB No. IEC107014) approval for our project to analyze the cohort data.
Assessment
Insomnia symptoms, stress, and QoL were evaluated for the cohort. Participants in the cohort were asked how much they felt stressed during their everyday life on a Likert-type scoring ranging from 0 to 3 points. To evaluate insomnia symptoms, difficulty in falling asleep, disrupted sleep, and early morning awakening were evaluated based on their presence or absence (scored as one or zero point, respectively). These scores were totaled, ranging from 0 to 3 points (having all three insomnia symptoms yielded a score of 3 points; having no insomnia symptom had a score of 0 point). Stress and insomnia symptoms were inevitably quantified by referring to their answers to questions because the information evaluated with the verified questionnaire was insufficient in this cohort study. QoL was evaluated using the Korean version of the World Health Organization Quality of Life Scale Brief Version (WHOQOL-BREF) scale ranging from 20 to 100 points [19]. Scores of WHOQOL-BREF were summed, with a higher score indicating a higher QoL.
Statistical analysis
Data used in this study were analyzed using IBM SPSS version 21 (IBM Corp., Armonk, NY, USA). SPSS PROCESS macro was used to test models. First, measurement data of stress, insomnia, and QoL were expressed as mean±standard deviation (SD). Second, t-test and chi-squared test were performed to compare differences in major variables between insomnia symptom and non-insomnia symptom groups. Third, correlation analysis was performed using Pearson correlation test. Fourth, to examine whether insomnia symptoms mediated the relationship between stress and QoL, PROCESS macro (model 4) was used. PROCESS offers 95% bias-corrected bootstrap confidence intervals for indirect effects from 5,000 resamples. Mediation analysis was performed for the total insomnia symptom group. Further subgroups analysis was performed according to age, sex, and average monthly income. An additional multiple regression analysis with age, sex, average monthly income, and stress as covariates was performed to determine correlations of three insomnia sub-symptom groups with QoL.
RESULTS
Among a total of 3,714 participants, 42.7% were males and 57.3% were females. Their mean age was 57.3 years (SD=8.74 years). In terms of average monthly income, 2,011 participants earned from ₩0 to ₩990,000, 1,394 participants earned from ₩1,000,000 to ₩2,990,000, and 309 participants earned more than ₩3,000,000.
Table 1 shows differences in QoL, stress, income, and sex between insomnia and non-insomnia symptom groups. We divided cohort participants into two groups using the following three items: 1) difficulty in falling asleep, 2) disrupted sleep, 3) early morning awakening. Participants who answered yes to at least one symptom were classified into the insomnia symptom group. Participants who answered no to all symptoms were classified into the non-insomnia symptom group. QoL was better in the non-insomnia symptom group (t=77.036, p<0.001) than in the insomnia symptom group (t=71.374, p<0.001). Stress levels were lower in the non-insomnia symptom group (t=0.93, p<0.001) than in the insomnia symptom group (t=1.18, p<0.001). When average monthly income level was analyzed, 60.4% of the insomnia symptom group earned ₩0–990,000, 32.7% earned ₩1,000,000–2,990,000, and 6.9% earned ₩3,000,000. In the non-insomnia symptom group, 45.3% of participants earned ₩0–990,000, 44.4% earned ₩1,000,000–2,990,000, and 10.3% earned ₩3,000,000 or more. These results confirmed a difference in income level between insomnia and non-insomnia symptom groups (χ2=83.410, p<0.001).
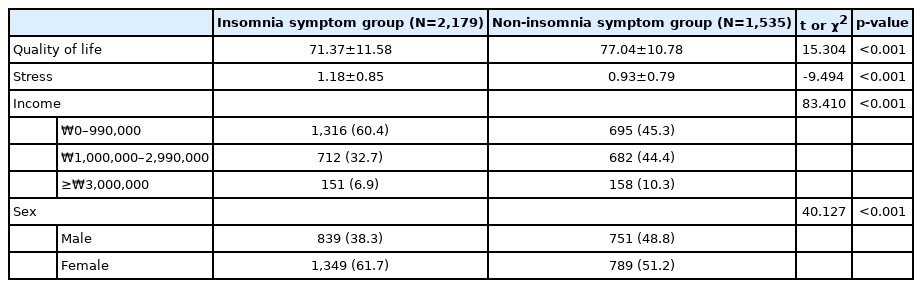
Differences in quality of life, stress, average monthly income, and sex between insomnia symptom group and non-insomnia symptom group (N=3,714)
Differences were also analyzed according to sex. There were 38.3% males and 61.7% females in the study cohort. In the non-insomnia symptom group, the percentage was 48.8% for males and 51.2% for females. There was a significant difference in sex between insomnia and non-insomnia symptom groups (χ2=40.127, p<0.001).
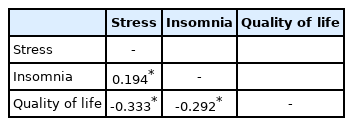
Results of descriptive analysis of correlations are shown in Table 2. According to the analysis, all measures were significantly associated with each other. Stress showed a significant positive correlation with insomnia symptoms (r=0.194, p<0.01) and a significant negative correlation with QoL (r= -0.333, p<0.01). Moreover, insomnia symptoms and QoL were negatively related with each other (r=-0.292, p<0.01). Mean scores of stress, insomnia, and QoL are 1.08±0.81, 1.13±1.14, and 73.71±11.60, respectively.
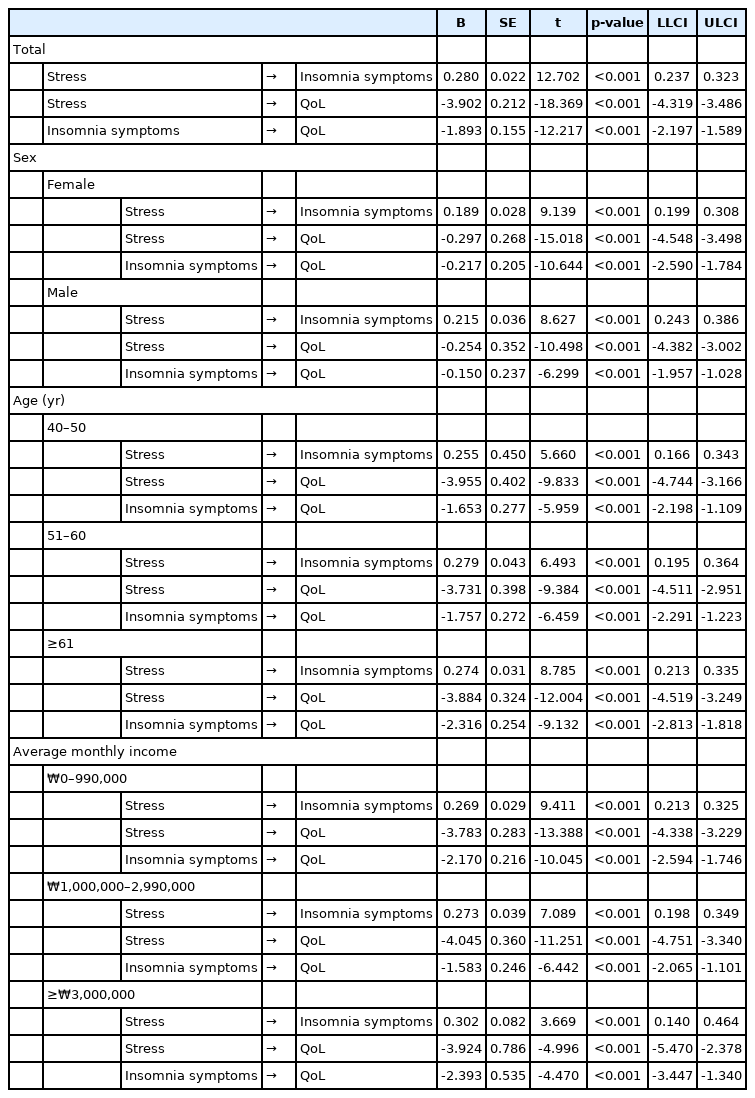
Mediation analysis results of stress, insomnia symptoms, and QoL are summarized in Table 3 and Figure 1. Age, sex, and average monthly income were included as covariates in the model. Stress was positively associated with insomnia symptoms (B=0.280, p<0.001), which in turn predicted QoL (B=-1.893, p<0.001). In Table 4, bootstrapping analysis further indicated that had insomnia symptoms a significant indirect effect on QoL (indirect effect=-0.530, SE=0.061, 95% CI=-0.658, -0.418). The residual direct relationship between stress and QoL was also significant (B=-3.902, p<0.001). Therefore, insomnia symptoms partially mediated the relationship between stress and QoL.
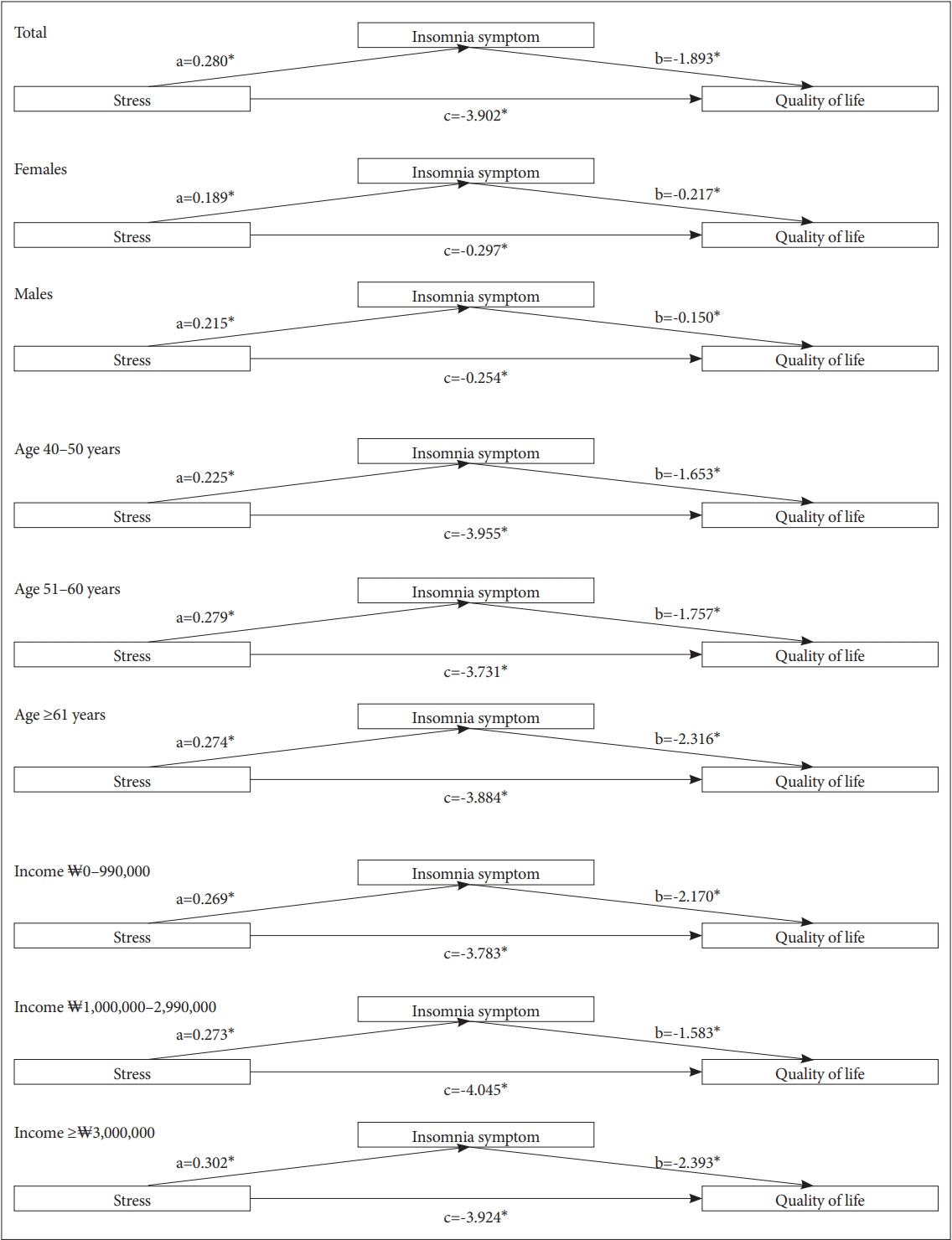
Mediation analysis of stress, insomnia symptom, and quality of life according to factors. *p*lt;0.001. a, path coefficient between stress and insomnia symptom; b, path coefficient between insomnia symptom and quality of life; c, path coefficient between stress and quality of life after controlling for insomnia symptom.
Mediation analysis results of stress, insomnia symptoms, and QoL according to sex are summarized in Table 3 and Figure 1. Age and average monthly income were included as covariates in the model. In females, stress was positively associated with insomnia symptoms (B=0.189, p<0.001), which in turn predicted QoL (B=-0.217, p<0.001). As shown in Table 4, bootstrapping analysis further indicated that had insomnia symptoms a significant indirect effect on QoL (indirect effect=-0.555, SE=0.082, 95% CI=-0.719, -0.403). The residual direct relationship between stress and QoL was also significant (B=-0.297, p<0.001). In males, stress was positively associated with insomnia symptoms (B=0.215, p<0.001), which in turn predicted QoL (B=-0.150, p<0.001). In Table 4, bootstrapping analysis further indicated that had insomnia symptoms a significant indirect effect on QoL (indirect effect=-0.469, SE=0.096, 95% CI=-0.669, -0.293). The residual direct relationship between stress and QoL was also significant (B=-0.254, p<0.001). The effect of stress on QoL by insomnia symptoms was greater in females than in males. Mediation analysis results of stress, insomnia symptoms, and QoL according to age are summarized in Table 3 and Figure 1. Sex and average monthly income were included as covariates in the model. In the age category of 40–50 years, stress was positively associated with insomnia symptoms (B=0.255, p<0.001), which in turn predicted QoL (B=-1.653, p<0.001). As shown in Table 4, bootstrapping analysis further indicated that had insomnia symptoms a significant indirect effect on QoL (indirect effect=-0.421, SE=0.107, 95% CI=-0.639, -0.229). The residual direct relationship between stress and QoL was also significant (B=-3.955, p<0.001). In the age category of 50–60 years, stress was positively associated with insomnia symptoms (B=0.279, p<0.001), which in turn predicted QoL (B=-1.757, p<0.001). As shown in Table 4, bootstrapping analysis further indicated that had insomnia symptoms a significant indirect effect on QoL (indirect effect=-0.491, SE=0.112, 95% CI=-0.729, -0.291). The residual direct relationship between stress and QoL was also significant (B=-3.731, p<0.001). In the age category of 61 years or older, stress was positively associated with insomnia symptoms (B=0.274, p<0.001), which in turn predicted QoL (B=-2.316, p<0.001). As shown in Table 4, bootstrapping analysis further indicated that had insomnia symptoms a significant indirect effect on QoL (indirect effect=-0.634, SE=0.101, 95% CI=-0.838, -0.445). The residual direct relationship between stress and QoL was also significant (B=-3.884, p<0.001). Mediation analysis results of stress, insomnia symptoms, and QoL according to average monthly income are summarized in Table 3 and Figure 1. Sex and age were included as covariates in the model. For those with an average monthly income ₩0–990,000, stress was positively associated with insomnia symptoms (B=0.269, p<0.001), which in turn predicted QoL (B=-2.170, p<0.001). As shown in Table 4, bootstrapping analysis further indicated that had insomnia symptoms a significant indirect effect on QoL (indirect effect=-0.584, SE=0.086, 95% CI=-0.761, -0.427). The residual direct relationship between stress and QoL was also significant (B=-3.783, p<0.001). For those with average monthly income of ₩1,000,000–2,990,000, stress was positively associated with insomnia symptoms (B=0.273, p<0.001), which in turn predicted QoL (B=-1.583, p<0.001). As show in Table 4, bootstrapping analysis further indicated that had insomnia symptoms a significant indirect effect on QoL (indirect effect=-0.433, SE=0.093, 95% CI=-0.627, -0.262). The residual direct relationship between stress and QoL was also significant (B=-4.045, p<0.001). For those with average monthly income of ₩3,000,000, stress was positively associated with insomnia symptoms (B=0.302, p<0.001), which in turn predicted QoL (B=-2.393, p<0.001). As shown in Table 4, bootstrapping analysis further indicated that had insomnia symptoms a significant indirect effect on QoL (indirect effect=-0.723, SE=0.277, 95% CI=-1.325, -0.242). The residual direct relationship between stress and QoL was also significant (B=-3.924, p<0.001).
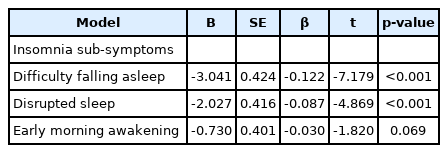
Results of multiple regression analysis for the relationship between insomnia sub-symptoms and QoL after adjusting for covariates including age, sex, average monthly income, and stress are summarized in Table 5. Among insomnia sub-symptoms, difficulty in falling asleep (β=-0.122, p<0.001) and disrupted sleep (β=-0.087, p<0.001) sub-symptoms were significantly negatively correlated with QoL as an independent predictive variable. However, early morning awakening sub-symptom had no significant correlation with QoL (β=-0.030, p=0.069).
DISCUSSION
QoL generally refers to the state perceived and felt by an individual concerning their goals, expectations, standards, and interests in the context of the culture and value system in which they live. The concept of QoL can be expressed in terms of individual-reported health, social and occupational status, and other life-related satisfaction measures such as the WHOQOL-BREF scale [19,20]. A high QoL scale score reflects a reduction in symptoms of a person with a particular illness or condition as well as an overall improvement in self-assessment of one’s health [21]. This is especially important when assessing whether a therapeutic intervention has achieved the goal of restoring health rather than merely treating symptoms.
Studies have shown that annual prevalence of insomnia symptoms and insomnia disorders are 35%–50% and 10%–22%, respectively, depending upon how insomnia is defined [22-24]. In Korea, the prevalence of insomnia symptoms and insomnia disorders have been reported to be approximately 17%–23% and 5%, respectively [25-27]. In this study, it was found that about 58% of participants experienced at least one of three insomnia symptoms (difficulty in falling asleep, disrupted sleep, and early morning awakening). Due to the nature of the cohort data, this study did not evaluate insomnia disorder according to the diagnostic criteria, but evaluated it by asking participants about insomnia symptoms. Therefore, limitations of these evaluation methods could be the cause of the relatively high proportion of insomnia symptom in subjects of this study.
It is known that insomnia is more common in women than in men. Its prevalence increases with age in both men and women [27]. This study also confirmed that females experienced Insomnia symptoms more frequently than males. The difference in sex ratio was significant between insomnia and non-insomnia symptom groups. Socioeconomic status itself is a critical stressor that can affect social activities, support systems, occupational distribution, living environment, and sleep [28,29]. This study also confirmed that the rate of experiencing insomnia symptoms showed a tendency to be much higher in the low-income group, suggesting that socioeconomic status was closely related to insomnia symptoms.
QoL can be used as an indicator of consequences and effects of insomnia to help understand its effects on daily lives of people experiencing it directly or indirectly. From this study, we found that insomnia symptoms negatively affected QoL in the Korean cohort population, suggesting negative consequences of insomnia symptoms in our daily lives. In this study, multiple regression analysis was additionally performed to determine effects of sub-symptoms of insomnia on QoL. Among the three insomnia sub-symptoms, difficulty in falling asleep and disrupted sleep were found to be significant independent variables that could have a negative effect on QoL, whereas early morning awakening did not have a significant effect. Researchers have made various attempts to classify sub-symptoms of insomnia by reflecting the duration of insomnia, an integrated classification of insomnia and personality aspects, and clinical features of insomnia (such as early, middle, and late insomnia) [30-32]. Based on this, studies have been conducted on how detailed symptoms of insomnia could lead to various outcomes such as QoL [30-33]. The present study attempted to analyze the effect on QoL based on detailed symptoms reflecting clinical aspects of insomnia symptoms. As a result, it was confirmed that early (difficulty falling asleep) and middle (disrupted sleep) insomnia sub-symptoms had a significant effect on QoL. This is a meaningful finding as few such analytical approaches have been used in previous studies. Applying this finding, it is necessary to intensively treat patients with early and middle insomnia sub-symptoms and to closely evaluate their effects on QoL in the clinical field.
Stress is a widespread phenomenon inevitably experienced by everyone during their lifetime. It is necessary to respond appropriately to stress, which is the ability to cope with stress. Allostasis, a normal physiological response to stress, can activate sympathetic-adrenal-medullary and hypothalamic-pituitary-adrenal (HPA) axes and stimulate adrenal glands to produce stress hormones (e.g., corticosteroids) and catecholamine (e.g., epinephrine and norepinephrine), allowing one to cope with or fight stressful situations [34]. Repeated cycles of activation and inactivation of allostasis over time or the inability to adequately cope with stress can alter a person’s diurnal cortisol rhythm and trigger hormone dysfunction called glucocorticoid resistance [5,35]. If these stresses are not adequately resolved or become chronic, changes in physiological (e.g., diurnal cortisol rhythm or inflammatory functions) or behavioral factors (e.g., physical activity, harmful use of cigarettes and alcohol, or eating patterns) due to stress can occur, which are known to negatively impact physical and psychological health [36].
Several studies have reported that major or minor stress has a negative effect on sleep, which is known to cause insomnia or worsen insomnia symptoms [37,38]. A study analyzing patients with insomnia has reported that adverse life events centered on interpersonal relationships are more common, stress coping skills are diminished, and self-esteem is relatively low in those with insomnia than in those with normal sleep [39]. In general, hyperarousal is considered a key mediating factor in stress-induced insomnia [40]. Several studies have reported that arousal is increased physiologically and cognitively in subjects with sleep disturbances [41,42]. Experimental studies have also confirmed that pre-sleep stress can increase physiological arousal at bedtime for insomniac and non-insomniac subjects [43]. If a person experiences stress without coping with it appropriately, internal conflicts can worsen and he or she can repeatedly ruminate on past situations. Such series of psychological reactions are likely to result in insomnia by increasing arousal.
Although previous studies have reported a significant relationship between stress and QoL, most studies investigating the relationship between stress and QoL were limited to a specific age, occupational group, or health status [7,44-46]. To the best of our knowledge, no study has reported whether insomnia could act as a mediating factor affecting the relationship between stress and QoL. This study was meaningful in that it explored the role of insomnia symptoms as a mediating factor affecting the relationship between stress and QoL in a cohort sample of the general population. Our analysis confirmed that stress could have a significant adverse effect on QoL and that insomnia symptoms could act as an important factor mediating the relationship between stress and QoL. A series of processes were confirmed in which stress increased insomnia symptoms. The more severe the insomnia symptoms, the lower the QoL. In particular, it could be estimated that the effect of insomnia symptoms on QoL was more significant than that of stress on insomnia symptoms. Stress can be experienced universally in daily life. However, how one is affected by stress and experiences difficulties such as insomnia can vary from person to person depending on how they cope with stress. Although there might be differences in the degree of discomfort caused by insomnia symptoms perceived by some individuals, insomnia symptoms can significantly affect QoL.
When an additional analysis was conducted according to sex, we found that the effect of stress on QoL was more significant in females than in males and that insomnia symptoms as a mediating factor significantly affected QoL of females. These results showed that when insomnia symptom was a mediating factor and stress affected QoL, females might have more difficulty than males. In general, it is known that women have more frequent and severe somatic symptoms and mental distress than men. Their medical help-seeking behaviors have also been reported to be more common [47]. The persistence of insomnia symptoms is also significantly higher in women [48]. Women experience relatively more severe social stress. They often have lower socioeconomic levels than men. In addition, they have a complex female hormone process with different physiological indicators such as HPA axis dysfunction which is related to hyperarousal [49-51]. Women also tend to perceive stressful events as more distressing than men [52]. The higher response to stress and the higher frequency of depression and anxiety in women also support the sex difference found in this study [53].
An additional analysis of the mediating effect of insomnia according to age showed that the effect of stress on QoL was significantly mediated by insomnia symptoms in all age groups. In particular, insomnia symptoms had a larger mediating effect in the age group of 61 years or older than in the age category 40–50 years. It has been reported that older adults who are 61 years or older frequently experience difficulty in falling asleep, disrupted sleep, and early morning awakening. Insomnia in the elderly can affect their daily life [54]. It can decrease their QoL and daytime functioning and increase their psychological disorders [55]. A previous study has investigated effects of stress, insomnia symptoms, and QoL and found that differential diagnosis for stress, medications, and psychiatric disorders of the elderly are required to understand reasons of insomnia [56].
This study has several limitations. First, the evaluation methods of insomnia and stress were relatively insufficient to derive quantitative values. Although QoL was measured using a scale, stress and insomnia were not assessed with validated scales. Stress was evaluated by a Likert-type scoring. Insomnia symptoms were divided into early, middle, and late types of insomnia and scored according to the number of symptoms. Although the weak point that evaluation methods were not assessed with validated scales could be partially compensated, insomnia symptoms need to be analyzed carefully in the future. Second, this was not a prospective study. Since there were limitations in the study design, we should be careful when interpreting findings of this study, especially when estimating the influence or causal relationship of factors. However, it was sufficiently strong mediation analysis using a large, community-based cohort sample of 3,714 patients. Third, we did not adequately identify, correct, or analyze confounding factors that might affect stress, insomnia, and QoL. In this study, sex, age, and income level were adjusted as confounding factors. However, many more factors could have a profound effect. Due to difficulties in securing data, other variables that could be confounding factors were not sufficiently considered in this analysis. There was a clear limitation in that the average monthly income included in the analysis of this study was not about average income per household because it was based on individual income. This should be interpreted considering the fact that more than half of individuals reported that their average monthly incomes were less than ₩1,000,000 per month. In future research, we intend to obtain significant results by ensuring a large-scale sample with more variables. Fourth, in additional analysis of independent variables affecting QoL, limited covariates should be applied to only insomnia sub-symptoms. In this study, stress was scored with a simple Likert type. It was not suitable for regression analysis. In addition, there was a limitation in securing additional covariates such as psychological state. Thus, sufficient confounding factors could not be applied to the analysis. However, regression analysis is not the main purpose of this study, but an additional analysis. It is meaningful as an interpretation of study results considering its limitations.
Stress is pervasive in our lives. We are constantly responding to stress in our lives. Although there is a difference in severity, insomnia symptoms are also frequently experienced. To achieve a more comprehensive and holistic state of health, understanding the impact of stress and insomnia on QoL can provide meaningful clues. For a better and stable QoL, it is necessary to focus clinical and social competence on identifying, improving, and preventing the degree and influence of stress and the state of insomnia as a mediating factor.
Notes
Availability of Data and Material
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
Heon-Jeong Lee, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Heon-Jeong Lee, Chul-Hyun Cho. Data curation: Heon-Jeong Lee, Chul-Hyun Cho. Formal analysis: Seulki Lee, Chul-Hyun Cho. Funding acquisition: Chul-Hyun Cho. Investigation: Seulki Lee, Chul-Hyun Cho. Methodology: Seulki Lee, Chul-Hyun Cho. Project administration: Heon-Jeong Lee, Chul-Hyun Cho. Resources: Heon-Jeong Lee. Software: Seulki Lee, Chul-Hyun Cho. Supervision: Heon-Jeong Lee, Chul-Hyun Cho. Validation: Chul-Hyun Cho. Visualization: Seulki Lee. Writing—original draft: Seulki Lee, Chul-Hyun Cho. Writing—review & editing: Heon-Jeong Lee, Chul-Hyun Cho.
Funding Statement
This work was supported by grants (NRF-2020R1C1C1007463 and NRF-2021R1A5A8032895) of the National Research Foundation of Korea (NRF) funded by the Government of Korea (MSIT).
Acknowledgements
This study obtained biospecimens and data from the Korean Genome Analysis Project (4845-301), the Korean Genome and Epidemiology Study (4851-302), and the Korea Biobank Project (4851-307, KBP2013-000), which were supported by the Center for Disease Control and Prevention, Republic of Korea.