Discrepancy Between Desired Time in Bed and Desired Total Sleep Time, Insomnia, Depression, and Dysfunctional Beliefs About Sleep Among the General Population
Article information
Abstract
Objective
The aim of this study was to explore the factors that can influence the severity of insomnia in the general population. We also aimed to examine whether sleep effort mediates the association between dysfunctional beliefs about sleep or the discrepancy between desired time in bed and desired total sleep time (DBST) and insomnia severity in individuals.
Methods
A total of 387 participants enrolled in this e-survey study. The symptoms were rated using the insomnia severity index (ISI), Patients Health Questionnaire-9 items, Dysfunctional Beliefs about Sleep-2 items, Glasgow Sleep Effort Scale, and Stress and Anxiety to Viral Epidemics-6 items. In addition, we defined a new sleep index named the DBST index. A linear regression analysis was performed to explore the factors predicting ISI scores, and mediation analysis was implemented to explore whether persistent preoccupation with sleep mediated the influence of dysfunctional beliefs about sleep and DBST on insomnia severity.
Results
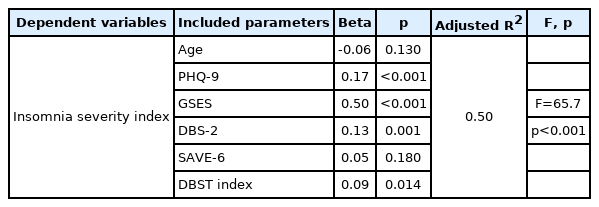
A linear regression analysis investigated depression (β=0.17, p<0.001), sleep effort (β=0.50, p<0.001), dysfunctional beliefs about sleep (β=0.13, p=0.001), and DBST (β=0.09, p=0.014) (adjusted R2=0.50, F=65.7, p<0.001). Additionally, we observed that persistent preoccupation with sleep partially mediated the influence of dysfunctional beliefs about sleep and DBST on insomnia severity.
Conclusion
Depression, preoccupation with sleep, dysfunctional beliefs about sleep, and DBST influenced the insomnia severity of the general population. We also observed that a persistent preoccupation with sleep partially mediated the influence of dysfunctional beliefs about sleep and the DBST index on insomnia severity.
INTRODUCTION
Insomnia disorder involves difficulty initiating and/or maintaining sleep despite adequate opportunities. Insomnia has an impact on personal, professional, and social functioning along with fatigue, cognitive impairments, and poor motivation. In South Korea, according to the statistics from the National Health Insurance Service-National Sample Cohort, the prevalence of insomnia increased from 3.10% among women and 1.62% among men in 2005 to 7.20% among women and 4.32% among men in 2013 [1].
Dysfunctional beliefs about sleep refer to maladaptive ideas and worry about sleep that are detrimental to sleep. Indeed, these dysfunctional beliefs are one of the critical factors that adversely impact sleep and exacerbate insomnia [2]. Poor sleepers with dysfunctional belief about sleep tend to excessively worry about the immediate or long-term negative consequences of insomnia. For instance, “If I don’t get enough sleep, my immune system will be broken down and then I will get sick” or “I may get dementia.” Others fear the potential consequences of insomnia on their daytime functioning. Such unhelpful faulty expectations and excessive worry produce emotional distress and trigger autonomic arousal, which perpetuates the vicious cycle of insomnia. Chronic insomnia patients have more dysfunctional beliefs about sleep and complain more negatively about the consequences of insomnia compared to healthy sleepers [3].
Discrepancy between the desired time in bed and desired total sleep time
Generally, people think that they need to sleep for at least 6–8 h a day. However, patients with dysfunctional beliefs about their sleep problem often go to bed early in the evening to obtain quick sleep [4]. They believe that an early bedtime may induce an early sleep onset. However, based on the two-process model, maintaining wakefulness for several hours is essential for falling asleep in a timely manner [5,6]. The two-process model of sleep regulation is one of the most prevalent conceptual models of sleep regulation, which posits that sleep is regulated by the interaction of a homeostatic process (Process S) with a circadian pacemaker (Process C). Especially, Process S sets forth that the sleep-inducing force increases as wakefulness is prolonged. Previously, we have reported that insomnia patients with sleep latency ≤30 min tended to go to bed late.7 We showed that the duration from the wake-up time to bedtime in patients with sleep latency ≤30 min (16.5±1.1 h) was longer than in the patients with sleep latency >30 min (15.8± 1.5 h, p<0.01). In addition, in the same paper, a short sleep latency was significantly correlated with a long duration from wake-up time to bedtime (r=-0.43, p<0.01). The study showed that a pressure to sleep (homeostatic drive) is also needed to promote good sleep, even though the circadian rhythm is adequate. Going to bed early might increase the time in bed (TIB) during the night. Therefore, we considered that the discrepancy between one’s desired total sleep time (TST) and desired TIB may be related to the severity of insomnia.
In this study, we defined a new sleep index, namely ‘discrepancy between desired time in bed and desired total sleep time (DBST) index.’ People who suffer from insomnia desire to sleep more and to fall asleep at an earlier time, and they often state, “I have no wish if I can have at least 6 hours of sleep!” In order to sleep for at least 6 hours, these individuals should go to bed 6 hours before their waking time (i.e., 11 pm bedtime and 5 am wake-up time). However, they tend to go to bed earlier in the evening to attempt falling asleep early, yet they wake up late in the morning since they cannot easily fall asleep. From this clinical observation in the specialized sleep clinic, we hypothesized that DBST may be associated with insomnia severity. A high DBST indicates that one desires to sleep more even though he/she states that they only require a short duration of sleep.
Mediating effect of persistent preoccupation with sleep
Preoccupation with sleep has long been established as a key factor for insomnia. Sleep preoccupation mediated the overall attributions for poor sleep and, specifically, sleep effort and sleep pattern problem attributions. According to Harvey’s model [2], excessively negative-toned cognitive activity, selective attention and monitoring, distorted perceptions, dysfunctional beliefs, and safety behaviors interact to fuel insomnia. These types of preoccupations with sleep begin at the point of waking and continue throughout the day. People with insomnia selectively attend to and monitor the physical sensations of the deficit throughout the day. Additionally, compensatory behaviors, such as taking a nap or drinking a lot of coffee, are used to solve the perceived deficit. Together, these appraisal processes and behaviors confirm the presence of a sleep deficit and create a vicious cycle of negative thinking and worry, leading to actual decrements in functioning. However, to the best of our knowledge, there is no previous literature on the mediating effect of preoccupation with sleep on the association between dysfunctional beliefs about sleep or DBST and insomnia severity.
In this study, we attempted to identify the factors that can influence the severity of insomnia of the general population, among depression, viral anxiety, sleep effort, or dysfunctional beliefs about sleep. Additionally, we examined whether sleep effort mediates the association between dysfunctional beliefs about sleep or the DBST index and insomnia severity. We hypothesized the following: 1) dysfunctional beliefs will be positively related to insomnia severity, 2) DBST will be positively associated with insomnia severity, and 3) persistent preoccupation with sleep will partially mediate the relationships.
METHODS
Participants and procedure
This anonymous online survey was conducted during November 9–15, 2021; additionally, a total of 400 individuals of the general population voluntarily participated through the survey system of the professional survey company, EMBRAIN (www.embrain.com). The study protocol was approved by the Institutional Review Board (IRB) of the Asan Medical Center (2021-1490), and requirement for written informed consent was waived by the IRB. We collected information regarding the participants’ age, sex, area of residence, and marital status; however, we did not collect any identifiable personal information. In this survey, we also collected responses to questions on coronavirus disease (COVID-19), such as “Did you experience being quarantined due to infection with COVID-19?”, “Did you experience being infected with COVID-19?”, or “Did you get vaccinated?” to exclude the influence of the COVID- 19 pandemic on the results of this study. In addition, we checked the participants’ past psychiatric history with the question, “Have you had experience with or been treated for depression, anxiety, or insomnia?” and checked current psychiatric distress with the question, “Now, do you think you are depressed or anxious, or do you need help for your mood state?” This e-survey was developed according to the Checklist for Reporting Results of Internet e-Surveys (CHERRIES) guidelines; [8] additionally, investigators (S.C. and C.HK.P) tested the usability and technical functionality before its implementation. The sample size was estimated based on 30 participants per cell [9]. We allocated 30–40 samples for ten cells (two groups of biological sex×five groups of age), and 400 participants were enrolled in this study.
Measures
Discrepancy between desired time in bed and desired total sleep time
The DBST index was defined as the difference between the desired TIB and desired TST. The participants’ desired TST was queried as “For how many hours do you want to sleep a day?” and the desired TIB was asked as “From what time to what time do you want to sleep?”. The desired TST was calculated by averaging the duration variable responses; (i.e., if a participant answered, “I want to sleep for 6 or 7 hours,” we calculated it as 6.5 h). The desired TIB was calculated as follows. First, we transformed the time variables into numeric variables based on 60 min; 15 min (one quarter of 1 h) was transformed to 0.25 (one quarter) and 30 min (half of 1 h) was 0.50 (i.e., 22:15 was transformed to 10.25) [10]. Second, we calculated the duration of TIB as a desired TIB (i.e., if a participant answered, “I want to sleep from 11:30 pm to 6:30 am,” we calculated the desired TIB as 7 h). The DBST index was calculated as [desired hours of TIB]-[desired hours of TST].
Insomnia severity index
The insomnia severity index (ISI) was developed to measure the severity of insomnia of an individual [11]. It consists of seven items that can be measured on a five-point Likert scale (0=no problem, 4=very severe problem), yielding a total score ranging from 0 to 28. We applied the Korean version of ISI in this study; [12] the Cronbach’s alpha among this sample was 0.86.
Patient Health Questionnaire
The Patient Health Questionnaire-9 items (PHQ-9) scale was developed to measure the severity of depression in an individual [13]. It consists of nine items, which can be rated on a fourpoint Likert scale ranging from 0 (not at all) to 3 (nearly every day). The total PHQ-9 score ranges from 0 to 27, and high scores denote severe levels of depression. We applied the Korean version of PHQ-9 (www.phqscreeners.com); additionally, the Cronbach’s alpha in this sample was 0.93.
Glasgow Sleep Effort Scale
The Glasgow Sleep Effort Scale (GSES) was developed to measure the persistent preoccupation of an individual with sleep [14]. It consists of seven items, which can be rated on a threepoint Likert scale, including not at all (0), to some extent (1), and very much (2). Higher scores reflect a greater effort to sleep. In this study, we applied the Korean version of GSES; [15] additionally, the Cronbach’s alpha among this sample was 0.84.
Dysfunctional Beliefs about Sleep-2 items
We measured the participants’ dysfunctional beliefs about sleep using the Dysfunctional Beliefs about Sleep-2 items (DBS-2) scale, which was edited from the original Cancerrelated Dysfunctional Beliefs about Sleep scale (C-DBS) [16]. The original C-DBS scale consists of two items, namely “My immune system will have serious problems if I don’t go to sleep at a certain time” (question 1, immune dysfunction) and “If I don’t sleep well at night, my cancer may recur or metastasize” (question 2, cancer recurrence). In this study we applied an edited C-DBS scale named as the DBS-2 scale after editing item 2 as “If I don’t sleep well at night, my health status will worsen.” The split-half coefficient among this sample was 0.86.
Stress and Anxiety to Viral Epidemics-6 items
The Stress and Anxiety to Viral Epidemics-6 items (SAVE- 6) is a rating scale that can measure anxiety regarding viral epidemics [17]. It consists of six items, and each can be rated on a five-point Likert scale ranging from 0 (never) to 4 (always). The total score of SAVE-6 ranges from 0 to 24; additionally, a high score reflects high levels of anxiety. In this study, we applied the original SAVE-6, which was developed in the Korean language, since we tried to adjust for the influence of the COVID-19 pandemic on the results of this study. The Cronbach’s alpha among this sample was 0.86.
Statistical analysis
The demographic variables and rating scales scores are summarized as mean±standard deviation. The level of significance was defined as two-tailed at values of p<0.05. Continuous variables were analyzed using the Student’s t-test and categorical variables were analyzed using the chi-squared test. Correlation analyses were conducted using Pearson’s correlation analysis. To explore the clinical variables predicting the ISI score, a linear regression analysis was performed adjusting rating scales scores, which were correlated with insomnia severity or the DBST index at a significance level of p<0.10. In addition, to explore whether persistent preoccupation with sleep mediated the influence of dysfunctional beliefs about sleep and the DBST index on insomnia severity, a bootstrap method with 2,000 resamples was implemented. We used SPSS version 21.0 and AMOS version 27 for Windows (IBM Corp., Armonk, NY, USA) to perform the statistical analysis.
RESULTS
Among a total of 400 patients, 13 participants were excluded due to inadequate response to their desired TIB and TST. All 387 participants were residents of Seoul (n=113, 29.2%), Pusan (n=30, 7.8%), Daegu (n=18, 4.7%), Daejeon (n=8, 2.1%), Gwangju (n=9, 2.3%), Incheon (n=29, 7.5%), Ulsan (n=8, 2.1%), Gyeonggi Province (n=106, 27.4%), Chungcheong Province (n=18, 4.7%), Jeolla Province (n=11, 2.8%), Gyeongsang Province (n=28, 7.2%), Gangwon Province (n=7, 1.8%), and Jeju Province (n=2, 0.5%). Table 1 shows the clinical characteristics of the participants. All 45 (11.6%) participants experienced being quarantined, 7 (1.8%) had been infected, and 353 (91.2%) participants were vaccinated. All 74 (19.1%) participants reported past psychiatric history and 49 (12.7%) participants reported current psychological distress.
The age of the participants was negatively correlated (Table 2) with ISI (r=-0.17, p<0.01), GSES (R=-0.15, p<0.01), PHQ-9 (r=-0.23, p<0.01), desired TST (r=-0.25, p<0.01), and desired TIB (r=-0.17, p<0.01). The ISI score was correlated with GSES (r=0.68, p<0.01), DBS-2 (r=0.36, p<0.01), PHQ-9 (r=0.53, p<0.01), SAVE-6 (r=0.31, p<0.01), desired TIB (r= 0.14, p<0.01), and DBST (r=0.17, p<0.01). The GSES score was significantly correlated with DBS-2 (r=0.31, p<0.01), PHQ- 9 (r=0.57, p<0.01), SAVE-6 (r=0.30, p<0.01), desired TIB (r= 0.13, p=0.013), and DBST (r=0.11, p=0.025). The DBS-2 score was correlated with PHQ-9 (r=0.29, p<0.01), SAVE-6 (r=0.31, p<0.01), desired TST (r=0.10, p=0.048), and desired TIB (r= 0.12, p=0.018). The PHQ-9 score was correlated with SAVE-6 (r=0.32, p<0.01) and desired TIB (r=0.15, p<0.01). The SAVE- 6 score was correlated with the desired TIB (r=0.16, p<0.01). The desired TST, desired TIB, and DBST index were significantly correlated with each other.
A linear regression analysis with enter methods was conducted to explore the expected variables for insomnia severity among the general population in this pandemic. The analyzed variables were depression (β=0.17, p<0.001), sleep effort (β=0.50, p<0.001), dysfunctional beliefs about sleep (β=0.13, p=0.001), and DBST index (β=0.09, p=0.014) (adjusted R2= 0.50, F=65.7, p<0.001) (Table 3).
A mediation analysis showed that the complete pathway from dysfunctional beliefs about sleep and DBST index (independent variable) through preoccupation with sleep (mediator) to insomnia severity (dependent variable) was significant (Table 4). This indicates that persistent preoccupation with sleep partially mediates the influence of dysfunctional beliefs about sleep and DBST index on their insomnia severity (Figure 1).
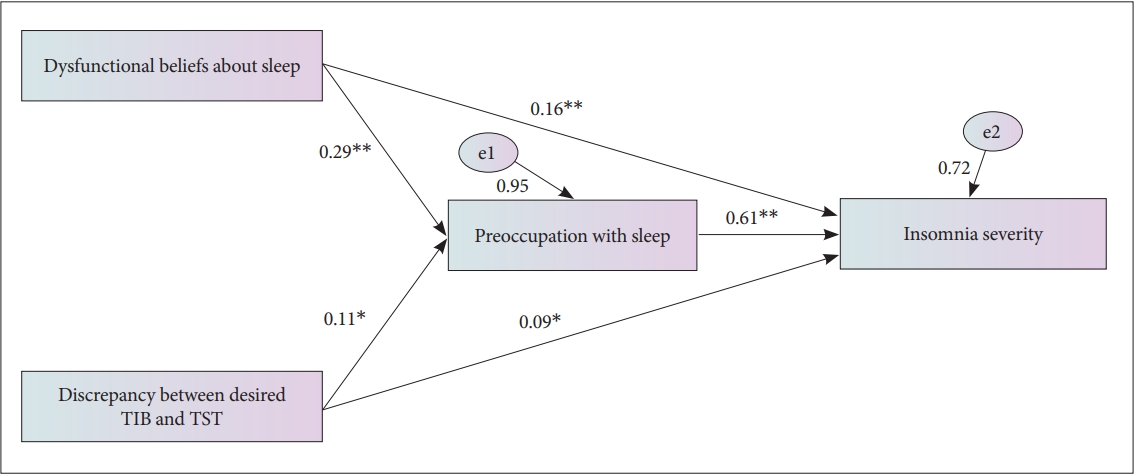
Mediation model showing the pathway from the effect of dysfunctional beliefs about sleep and discrepancy between desired time in bed and desired total sleep time (independent variables) on insomnia severity (outcome) through preoccupation with sleep (mediator). *p<0.05; **p<0.01. TST, total sleep time; TIB, time in bed.
DISCUSSION
In this study, we explored and identified the component that may influence the insomnia severity of the general population. We observed that the insomnia severity of the general population was influenced by their depression, preoccupation with sleep, dysfunctional beliefs about sleep, and DBST index. Furthermore, a persistent preoccupation with sleep partially mediated the influence of dysfunctional beliefs about sleep and DBST index on their insomnia severity.
Insomnia, depression, and dysfunctional beliefs about sleep
In general, depression is a significant factor influencing insomnia; [18] additionally, there is a bidirectional relationship between depression and insomnia [19]. Especially during the COVID- 19 pandemic, individuals have been shown to suffer from sleep disturbance or insomnia [20,21], and depression is one of the most significant predictors for the latter [22]. Post-pandemic insomnia was reported to be associated with higher levels of depression; [23] conversely, a change in sleep pattern due to COVID- 19 was significantly associated with depression [24]. Moreover, dysfunctional belief about sleep was a significant predictor of insomnia during the COVID-19 pandemic [25,26]. Dysfunctional sleep-related beliefs can be expected to be increased during the COVID-19 pandemic [26] and might affect the severity of insomnia.
However, in this study, anxiety regarding viral diseases was not a significant predictor of the insomnia severity of the general population during the COVID-19 pandemic. Previously, a high prevalence of anxiety and insomnia was reported among the general population [20,21]. Although we reported the possibility of the influence of anxiety on sleep disturbance among healthcare workers [27], the association of viral anxiety, assessed using the viral epidemic-specific rating scale, with insomnia was rarely reported among the general population. First, during the COVID-19 pandemic, we can presume that depression or stress, rather than anxiety, might be a strong predicting factor for sleep disturbances among the general population, although further studies are needed to provide evidence. Second, during the 2 years of the pandemic, individuals adapted to the viral anxiety, and it may be that their anxiety no longer influences the insomnia severity.
Discrepancy between desired time in bed and desired total sleep time and insomnia
We observed that the DBST index was significantly correlated with insomnia severity from the correlation analysis, as we hypothesized. Furthermore, this might be the first study that showed that a discrepancy between one’s desired TIB and desired TST can predict the severity of insomnia. The concept of DBST originated from the idea that patients with dysfunctional beliefs about their sleep problem often go to bed early in the evening, since they believe that an early bedtime may induce early sleep onset [4]. However, they will not get up early in the morning, although they went to bed early in the evening. Therefore, going to bed early in the evening might increase the TIB during the night. Previously, we have reported that the duration from the wake-up time to bedtime in patients whose sleep latency was ≤30 min was longer than that of patients whose sleep latency was >30 min [7]. In addition, a longer duration from wake-up time to bedtime predicted a sleep latency ≤30 min in our previous study [28], which was conducted among cancer patients. This concept might affect the sleeping pill ingestion time.
In our previous study on the association between the sleeping pill ingestion time and satisfaction with sleeping pills [10], we reported that a shorter interval between pill administration and wake-up time increased patient subjective satisfaction with sleeping pills. Additionally, we proposed to advise patients to take sleeping pills approximately 7 h before their usual getting- out-of-bed time, not 30 min before bedtime, which can lead to confusion regarding the time the pills must be taken for patients to induce short sleep latency. Among cancer patients [29], we reported that reducing the duration from the sleeping pill ingestion to wake-up time can influence the satisfaction of sleeping pills. Furthermore, we proposed using the sleep in- dex time in bed during a day (TIB/d) as the total TIB during 24 h. This concept is also similar to the concept of DBST in terms of a homeostatic drive (Process S). In this study, we considered that a high DBST means that one presumes to sleep more even though they say they need just a short duration of sleep. We hypothesized that the insomnia severity will be correlated with a high DBST; additionally, we confirmed it from the results of this study.
Mediation effect of persistent preoccupation with sleep
Individuals with insomnia suffer unpleasant intrusive thoughts and excessive and uncontrollable worry during the pre-sleep period [30]. It is suggested that dysfunctional beliefs were a major source of worry and preoccupation. These erroneous beliefs about sleep are highlighted as exacerbating factors of insomnia and fuel the excessive negative cognitive activity and preoccupation [2]. Subsequently, counterproductive maladaptive coping strategies, such as excessive TIB and staying in bed while awake are adopted to cope with the excessive cognitive activity [31]. Cognitive processes, dysfunctional beliefs about sleep, distorted perception, and attention work to make individuals increasingly anxious and preoccupied with the sleep problem. These excessive worries and ruminations trigger the activation of the sympathetic nervous system, autonomic arousal, and emotional distress contributing to the maintenance of insomnia.
This study has a few limitations. First, it was conducted via an anonymous online survey system. This might lead to bias; however, we conducted this study via online surveys rather than face-to-face interviews, to prevent the risk of a viral outbreak. Second, the relatively small sample of participants selected from a national area might decrease the statistical power of this study. In the COVID-19 pandemic chaos, it is difficult to gather enough participants from all national areas via a face-to-face interview. Third, the concept of DBST is not still sound, and it might be biased since the responses came from participants via the anonymous online survey system.
In conclusion, we observed that depression, preoccupation with sleep, dysfunctional beliefs about sleep, and DBST influence insomnia severity in the general population. Additionally, we observed that a persistent preoccupation with sleep partially mediates the influence of dysfunctional beliefs about sleep and DBST on their insomnia severity. Though we do not know whether this relationship was shown since it was influenced by COVID-19 or whether it will be present in the normal situation in the absence of the COVID-19 pandemic, we consider that reducing the preoccupation with sleep might be effective in improving sleep problems. Further, the DBST concept can be a useful index for predicting the severity of insomnia.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Seockhoon Chung, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Seockhoon Chung, Changnam Kim, Kikyoung Yi. Data curation: Seockhoon Chung, C. Hyung Keun Park, Joohee Lee, Inn-Kyu Cho, Kyumin Kim. Formal analysis: Seockhoon Chung. Funding acquisition: C. Hyung Keun Park. Writing—original draft: Joohee Lee, Seockhoon Chung. Writing—review & editing: all authors.
Funding Statement
This study was supported by the Institute for Information & communication Technology Planning & evaluation (IITP) grant funded by the Korea government (MIST) [2021-0-01521, Development of patient-specific cognitive behavioral therapy (CBT-I) digital treatment technology to improve insomnia].