The Influence of Physical Distancing, Sense of Belonging, and Resilience of Nursing Students on Their Viral Anxiety During the COVID-19 Era
Article information
Abstract
Objective
We aimed to explore how nursing students’ adherence to physical distancing, sense of belonging, or resilience may be associated with viral anxiety during the coronavirus disease (COVID-19) era in South Korea.
Methods
We conducted an online survey among nursing students from December 8–10, 2021. The survey gathered participants’ age, sex, grades, living area, and responses to questions on COVID-19. In addition, responses to Stress and Anxiety to Viral Epidemics-6 items (SAVE-6), adherence to physical distancing, Sense of Belonging Instrument, Calling and Vocation Questionnaire, Patient Health Questionnaire-9 items (PHQ-9), and Connor-Davidson Resilience Scale-2 (CD-RISC2) items were gathered.
Results
The SAVE-6 score was significantly correlated with adherence to physical distancing (r=0.29), PHQ-9 (r=0.26), and CD-RISC2 (r=-0.34, all p<0.01) similar to partial correlation analysis adjusting participants’ group (freshmen and sophomores vs. juniors and seniors). A linear regression analysis revealed that viral anxiety of nursing students was predicted by sex (female, β=0.20, p=0.001), adherence to physical distancing (β=0.25, p<0.001), sense of belonging (β=0.16, p=0.014), and CD-RISC2 score (β=-0.32, p<0.001) (adjusted R2=0.24, F=10.01, p<0.001).
Conclusion
We observed that adherence to physical distancing, sense of belonging, and their resilience influenced nursing student’s viral anxiety. An appropriate support system to manage viral anxiety is needed for nursing students during the COVID-19 pandemic.
INTRODUCTION
The coronavirus disease (COVID-19) pandemic that occurred in January 2020 caused great disruption in education, politics, economy, society, and culture. The prolonged pandemic situation and occurrence of new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) mutations have posed a threat to physical and mental health [1]. The COVID-19 outbreak has brought about major changes in education. College students faced a sudden change in the expansion of online classes instead of face-to-face classes and experienced difficulties in adjusting to campus life [2-4]. Due to the government’s strengthening of social distancing measures against COVID-19, college students did not experience actual campus life [5]. Within the Department of Nursing, it is mandatory to participate in clinical practice. However, considering the safety of nursing students, clinical practice was withheld or reduced. Various education methods using simulation and virtual reality were used as an alternative to reduced clinical practice [6]. Interruptions to theoretical and clinical practice following the COVID-19 pandemic were unexpected for nursing students. Furthermore, nursing students are experiencing anxiety, stress, and uncertainty owing to the changing circumstances of classes and hospital practice during the COVID-19 pandemic [7]. They also experience excessive mental pressure and worry about their future jobs [8]. Anxiety and stress can negatively affect college students’ resilience due to disruptions, including sudden delays in the start of classes, suspension of campus life, and changes to non-face-to-face classes due to COVID-19 [9,10]. The lower the anxiety of nursing students during the COVID-19 pandemic, the higher their resilience [9]. Thus, at this time, it is important to build resilience to maintain the mental and psychological well-being of nursing students and improve their life satisfaction [10].
Infection control strategies, such as physical distancing and staying home, prevent young people from interacting with colleagues and friends, leading to social and emotional isolation, anxiety, stress, and emotional exhaustion [11]. The pandemic has influenced nursing education, and during in-person education, there is emphasis on adherence to physical distancing and respecting health protocols [8]. In February 2020, the government declared Daegu a disaster zone because about 5,300 additional confirmed COVID-19 cases surged in 15 days in Daegu Metropolitan City, South Korea. As social and economic activities were reduced due to COVID-19, it was found that providing the National Disaster Relief Fund to the public, starting with small businesses, raised the awareness of local belonging among Daegu citizens. In Japan, the COVID-19 pandemic has also strengthened a sense of belonging and decision-making processes among Japanese nursing students [12]. Clinical placements are stressful environments, which can be overwhelming and undermine nursing students’ learning and confidence. The higher the sense of belonging of nursing students, the lower the stress experienced by them during clinical placements [13]. Students who experience a sense of belonging in an educational environment are more active and motivated to engage in educational activities, which has a greater impact on their learning [14]. Thus, it is important to promote a sense of belonging among nursing students through clinical practice, which can reduce stress and tension [15]. Understanding the impact of a sense of belonging and perceived stress on students is invaluable for nursing educators, faculties, and hospital managers [13].
Recently, the Korean government announced the policy of “living with coronavirus,” which began from November, 2021 [16,17], but the number of confirmed cases rapidly increased after that [18]. In this situation, this study was conducted not only among freshmen who did not fully experience campus life due to COVID-19 but also among nursing students who suddenly experienced a change in the educational environment from face-to-face to online classes. Despite the efforts of nursing schools and clinical sites, nursing students often felt lost in the chaos of the pandemic [8]. In this study, we tried to explore how nursing students’ adherence to physical distancing, sense of belonging, or resilience may be associated with viral anxiety during the COVID-19 pandemic in South Korea.
METHOD
Participants and procedure
This study was conducted among nursing students in South Korea from December 8–10, 2021. The target population was nursing students in Korea; freshmen or sophomores from a university and juniors or seniors undergoing clinical clerkship in a hospital were selected. The online survey was anonymously conducted and no personal identifiable information was gathered. Moreover, participation was voluntary. At the beginning of the survey, students were informed about the aim of the study, anonymity of results, and of the possibility to withdraw from the study at any time. Moreover, they were assured that there would be no disadvantages for not participating in this study. The study protocol was approved, and obtaining the written informed consent was waived by the Institutional Review Board (IRB) of University of Ulsan (approval number 2021R0052).
We developed the survey form using Google Forms, which can collect the responses to questions regarding participant’s age, sex, grades, living area, and responses to questions on COVID-19 such as “Did you experience quarantine due to COVID-19 infection?” or “Did you get vaccinated?” Participants’ past psychiatric history and current psychiatric symptoms were also assessed. We developed the online survey in Korean and followed the Checklist for Reporting Results of Internet e-Surveys (CHERRIES) guidelines [19]. Investigator (S.C.) tested the usability and technical functionality before its implementation. Participants could voluntarily access this survey form using the link presented on the poster for the enrollment, which was placed on a bulletin board at the nursing school. We provided participants a gift card valued at about $3.00 for participation.
Measures
Stress and Anxiety to Viral Epidemics-6 items
The Stress and Anxiety to Viral Epidemics-6 items (SAVE-6) is a rating scale which can measure one’s viral anxiety specifically in response to viral epidemics [20]. It was driven from the original SAVE-9 scale, which was developed to measure healthcare workers’ work-related stress and anxiety response to the viral epidemic [21]. The six items of the SAVE-6 are rated on a 5-point Likert scale ranging from 0 (never) to 4 (always). The total score of SAVE-6, which ranges from 0–24, reflects the levels of anxiety in response to viral epidemics. We divided participants into two groups based on the 15 points of SAVE-6 based on the previous studies, which reported the cut-off score of the SAVE-6 among the general population and medical students [22]. In this study, we applied the original SAVE-6, developed in the Korean language, to nursing students. Cronbach alpha was 0.833 in this sample.
Adherence to physical distancing scale
The adherence to physical distancing scale is a self-reported scale which can measure one’s adherence to the government’s physical distancing directives [23]. It contains seven items rated on a 5-point Likert scale ranging from 1 (never) to 5 (almost always). The scale has not yet been formally validated in the Korean language. With permission from the developer, we translated the original version into Korean and back-translated it to check the accuracy. Cronbach’s alpha was 0.722 in this sample.
Sense of Belonging Instrument
The Sense of Belonging Instrument (SOBI) is a self-reported scale that measures an individual’s sense of belonging [24]. In this study, SOBI-A, which measures the antecedents of an individual’s sense of belonging, was used. It comprises nine items that are rated on a 4-point Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree). Moreover, we applied the Korean version of the scale [25], and Cronbach’s alpha was 0.834 in this sample.
Calling and Vocation Questionnaire
The Calling and Vocation Questionnaire (CVQ) is a selfreported rating scale that assesses calling [26]. The 12 items of the CVQ scale are rated on a 4-point Likert scale ranging from 1 (not at all) to 4 (absolutely), and one item was reverse scored. A high total score reflects a high level of calling. In this study, we applied the Korean version of this scale (CVQ-K) [27], and Cronbach’s alpha in this sample was 0.826.
Patient Health Questionnaire-9 items
The Patient Health Questionnaire-9 items (PHQ-9) scale is a self-reported rating scale that measures the severity of depression [28]. The nine items of the PHQ-9 scale are rated on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). A high total score reflects a severe level of depression. In this study, we applied the Korean version of PHQ-9 [29], and Cronbach’s alpha was 0.871 in this sample.
Connor-Davidson Resilience Scale-2
The Connor-Davidson Resilience Scale-2 (CD-RISC2) scale is a 2-item shortened version of the original 25-item CD-RISC used to assess one’s resilience [30]. The CD-RISC2 is based on items 1 and 8 of the original scale. Respondents can answer the two items, with scores ranging from 0–8. In this study, the Korean version of CD-RISC2 was applied with the permission of the developer, and the Split-Half reliability coefficient was 0.778 in this sample.
Statistical analysis
We explored the association of nursing students’ viral anxiety during the COVID-19 pandemic with their demographic characteristics and symptoms rating scales scores. Demographic characteristics and rating scales scores are summarized as mean±standard deviation. The level of significance for the analyses was defined as two-tailed at values of p<0.05. We divided participants into two groups: high viral anxiety group (SAVE-6 score ≥15) and low viral anxiety group (SAVE-6 score <15). For comparisons between groups, continuous variables and categorical variables were analyzed using the Student’s ttest and chi-square test. Partial correlation analysis was conducted to explore the association between SAVE-6 and other rating scales scores by adjusting the effect of clinical clerkship (two groups; freshmen and sophomores vs. juniors and seniors). Finally, a linear regression analysis was performed to reveal the predicting variables for nursing student’s viral anxiety. We used Statistical Package for the Social Sciences version 21.0 (IBM Corp., Armonk, NY, USA), and JASP version 0.16 (Amsterdam, The Netherlands) to perform statistical analyses.
RESULTS
All 227 nursing students participated in this study (Table 1). Their mean age was 22.0±2.7 years (19–41 years old), and 196 (86.3%) were female. Among participants, 15 (6.6%) were freshmen, 65 (28.6%) were sophomores, 64 (28.2%) were juniors, and 83 (36.6%) were seniors. Moreover, 147 (64.8%) had undergone the clinical clerkship, 219 (96.5%) got vaccinated, 15 (6.6%) experienced being quarantined, and 35 (15.4%) reported presence of past psychiatric history. Between the two groups categorized based on the 15 points of the SAVE-6 scale [20,22], the proportion of female (p<0.001), SAVE-6 scores (p<0.001), adherence to physical distancing score (p=0.003), and PHQ-9 score (p<0.001) were significantly higher among high viral anxiety group (SAVE-6 ≥15) compared with the low viral anxiety group (SAVE-6 <15), whereas CD-RISC2 score was significantly lower (p<0.001) among high viral anxiety group compared with the low viral anxiety group. Between female (n=196) and male (n=31) nursing students, the SAVE-6 [t(225)=4.01, p<0.001] and PHQ-9 [t(225)=3.08, p<0.001] were significantly higher, and CD-RISC2 [t(225)=2.56, p=0.01] was significantly lower among female students compared to males. Between nursing students who are in the clinical clerkship (juniors/seniors) and not (freshmen/sophomores), there was no significant difference in all symptoms rating scales scores.
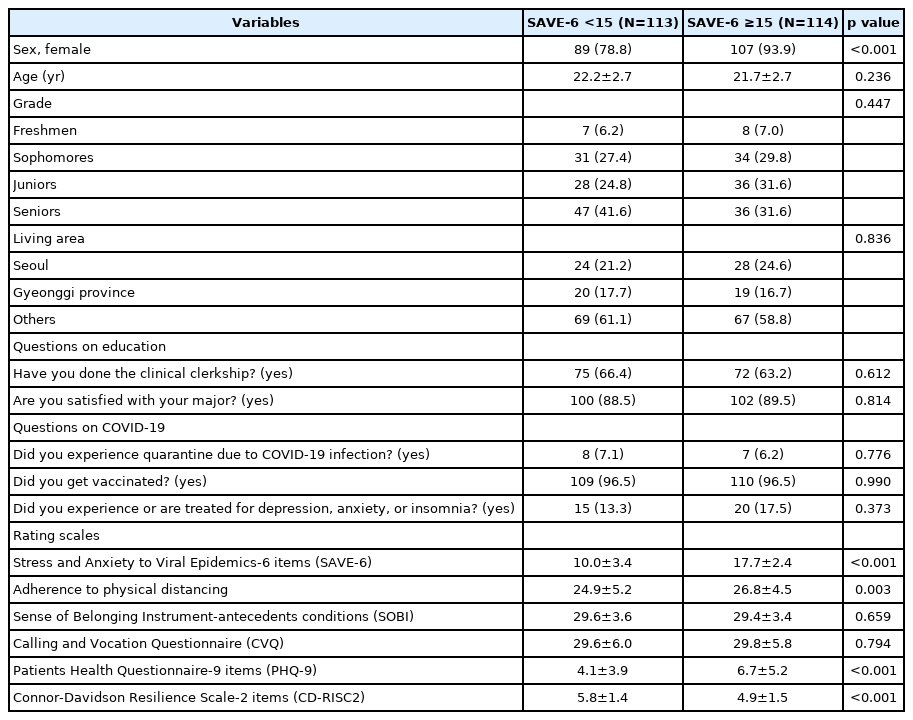
Comparison of clinical characteristics between high and low viral anxiety groups among nursing students (N=227)
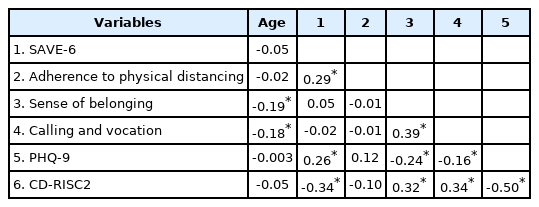
Pearson’s correlation coefficients for participants’ age and rating scales are shown in Table 2. Age was significantly correlated with sense of belonging (r=-0.19, p<0.01) and calling and vocation (r=-0.18, p<0.01). SAVE-6 was significantly correlated with adherence to physical distancing (r=0.29, p<0.01), PHQ-9 (r=0.26, p<0.01), and CD-RISC2 (r=-0.34, p<0.01). Sense of belonging was significantly correlated with calling and vocation (r=0.39, p<0.01), PHQ-9 (r=-0.24, p<0.01), and CD-RISC2 (r=0.32, p<0.01). Calling and vocation was significantly correlated with PHQ-9 (r=-0.16, p<0.01) and CD-RISC2 (r=0.34, p<0.01). PHQ-9 was significantly correlated with CD-RISC2 (r=-0.50, p<0.01). Partial correlation analysis adjusting participants’ group (freshmen and sophomores vs. juniors and seniors) did not show the difference in the results from that in Pearson’s correlation analysis.
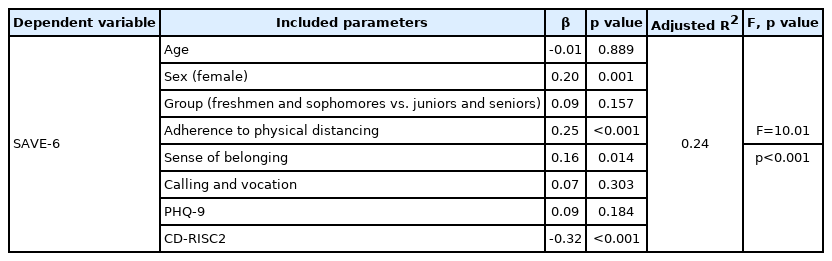
A linear regression analysis revealed that viral anxiety of nursing students was predicted by sex (female, β=0.20, p=0.001), adherence to physical distancing (β=0.25, p<0.001), sense of belonging (β=0.16, p=0.014), and CD-RISC2 score (β=-0.32, p<0.001) (adjusted R2=0.24, F=10.01, p<0.001) (Table 3).
DISCUSSION
In this study, we explored the predicting factors for nursing students’ viral anxiety during the COVID-19 era in South Korea. We also observed that nursing students’ viral anxiety was predicted by sex (female), adherence to physical distancing, sense of belonging, and resilience.
Clinical education is an integral part of nursing education. However, nursing students mentioned gaps in clinical education due to reduced numbers and diversity of non-COVID-19 patients, shortage of personal protective equipment, and reduced educational capacity of hospitals due to decline in the hospitalization of non-COVID-19 patients [8].
Adherence to physical distancing, sense of belonging, and viral anxiety
Physical distancing is an effective measure which can prevent transmission of the virus [31]. However, it imposed psychological distress on people and large costs on society. Previously, it was reported that social isolation was associated with increased fear, anxiety, loneliness, or depression [32]. Physical distancing is different than social isolation. Since the term social distancing may seem to be associated with social isolation, the term physical distancing rather than social distancing is now recommended [33]. During the COVID-19 pandemic, adherence to physical distancing was related to sense of personal responsibility or control over one’s own behavior [34], whereas decreased psychosocial well-being and lack of social support were associated with non-adherence to physical distancing [35]. Viral anxiety was also associated with adherence to physical distancing [36,37]. People who felt anxious about being infected with viruses tended to adhere to physical distancing. Nursing students, especially those under clinical clerkship, might feel anxious about becoming infected with SARS-CoV-2. They may worry about discontinuing their clinical clerkship [38], being infected while caring for patients [39], or fear transmitting the virus to their family members or friends [40]. Thus, clear guidelines and recommendation are needed to ensure medical education safety during the pandemic [8].
In a previous study targeting the general population, 49.7% of the participants showed mild degree of anxiety response to the viral epidemic (SAVE-6 score ≥15) [20], which was similar to the result obtained in this study. Due to the COVID-19 pandemic, in some countries, nursing students have been asked to voluntarily provide patient care [39]. However, in South Korea, nurses who were on leave or retired voluntarily returned to work to care for COVID-19 patients, while nursing students who were juniors and seniors cared for COVID-19 patients only as a part of their clinical practice.
In this situation, a sense of belonging can be considered an important part of one’s attitude to enhance adherence to physical distancing. Previously, sense of belonging was associated with low anxiety among medical students [41]; this reflects that sense of belonging may play a protective role for psychological distress during the pandemic. However, in this study, we observed that sense of belonging can act as a provoking factor for viral anxiety. We can consider that they felt a “forced” sense of belonging from their society, colleagues, or friends. During this pandemic, a sense of belonging or sense of community might be helpful to prevent the transmission of virus, but it can be stressful to individuals at the same time. To promote the sense of belonging of nursing students, it is necessary to provide a supportive and facilitating clinical environment and make students feel valuable through positive interactions [15].
Resilience and viral anxiety
Nursing students have high levels of anxiety even in normal environments but are exposed to additional stressors, such as fear of infection during a pandemic. Resilience, which refers to an individual’s ability to face adversity and respond effectively to challenges, was positively associated with nursing students’ ability to successfully participate in clinical practice and maintain well-being [42]. As in previous studies, resilience was found to be lower as anxiety increased and was confirmed to be a predictor of anxiety [9]. In nursing students who perceived themselves as having strong personalities, moderate and severe anxiety were significantly lower [43]. Resilience was found to reduce the negative effects of pandemic-associated stress on the life satisfaction and psychological well-being of nursing students [10]. Nursing faculty members should play an important role in teaching and strengthening the resilience of nursing students and help them maintain their mental and psychological well-being during the pandemic. For example, nursing schools can develop and integrate a resilience building program throughout the nursing curriculum to assist students with managing stress associated with academic, social, and personal challenges.
In this study, we also observed that being female was significantly associated with higher anxiety scores [43], and resilience was significantly lower. This is in line with the results of prior studies regarding the psychosocial distress caused by the COVID-19 pandemic [44]. In addition to their professional roles, women also play a social role as the primary caregiver in the family. Women are more sensitive than men, making them more vulnerable to anxiety [45]. Compared to men, women are more likely to find happiness in social networks and in their families but have lower self-confidence, lower self-efficacy, and fewer personal and material resources. When faced with adversity, women have a weaker sense of mastery than men. Moreover, age moderates the relationship between resilience and negative indicators of mental health; adults are stronger than children and adolescents, as resilience increases with age [46]. Therefore, the low resilience in this study is thought to be because most of the participants were women and college students.
Considering the fact that the majority of nursing students are female and that they account for 85.9% of participants in this study, this may partially explain the high prevalence of anxiety. During the COVID-19 pandemic, social isolation, economic instability, uncertainty about the future, difficulties in distance learning, and fear of infection are believed to have resulted in high anxiety. Thus, nursing faculties should keep in touch with their students to encourage and support them through this challenging period.
In this study, depression was not associated with adherence to physical distancing, and it was not included in the final model for predicting viral anxiety of nursing students. Previously, physical distancing or social distancing was considered to influence one’s depression [32]. However, depression can decrease adherence to physical distancing [47]. For example, depression might decrease one’s compliance with medical advice [48]. Thus, the relationship between depression and adherence to physical distancing was mixed in this sample. Furthermore, depression was not a predicting variable for viral anxiety despite the correlation between them. We can speculate that depression was phenomenologically associated with viral anxiety, but nursing students’ viral anxiety was not directly associated with their depression. Another explanation is that we applied the viral epidemic-specific anxiety scale and non-specific depression scale.
This study had several limitations. First, the proportion of classifications of the participants was not even in this sample. The high proportion of juniors and seniors who already underwent the clinical clerkship might influence the results. Second, a small sample size of 227 students and female preponderance in this sample can lead to bias. Third, this anonymous online survey possibly led to bias; however, it was not easy to conduct face-to-face interviews during the pandemic. Finally, this survey was conducted in December 2021, and students might have already adjusted to two years of the pandemic. However, the recent announcement of living with coronavirus policy from the Korean government might influence these results simultaneously.
In conclusion, we observed that adherence to physical distancing, sense of belonging, and their resilience influenced nursing student’s viral anxiety. Further studies should explore the importance of adherence to physical distancing and its mediating factors for psychological distress among nursing students.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Jeong Hye Kim, Seockhoon Chung. Data curation: Jeong Hye Kim, Min-Sook Seo. Formal analysis: Jeong Hye Kim, Seockhoon Chung. Investigation: Seockhoon Chung. Methodology: all authors. Project administration: Seockhoon Chung. Resources: Jeong Hye Kim. Software: Seockhoon Chung. Supervision: Jeong Hye Kim, Min-Sook Seo. Validation: Jeong Hye Kim, Min-Sook Seo. Visualization: Jeong Hye Kim, Min-Sook Seo. Writing—original draft: Jeong Hye Kim, Min-Sook Seo. Writing—review & editing: all authors.
Funding Statement
None