Mediation Effect of the Coping Strategies on the Relation Between Stress and Sleep Quality
Article information
Abstract
Objective
Recently data has been accumulated regarding the role of coping strategies in the relationship between stress and sleep quality. Therefore, we set out to identify the mediating effects of coping strategies between stress and sleep quality.
Methods
A online-based cross-sectional study was performed using the Perceived Stress Scale-10, the Pittsburgh Sleep Quality Index, and a simplification of the 60-item Coping Orientation to Problems Experienced (Brief COPE) inventory in the nonclinical adult sample. The 24 items of Brief COPE were categorized into four factors (social support, problem solving, avoidance, positive thinking). Then, we used the PROCESS macro to conduct the multiple mediation analysis for the four coping styles as potential mediators in the relationship between stress and sleep quality, and an additional subgroup analysis was examined to identify a gender difference for the mediation effect.
Results
As a group, four coping styles mediated significantly the association between perceived stress and poor sleep quality. And avoidance has maintained its significance thought all regression analyses. Finally, this results remained as same in the females.
Conclusion
The effect of perceived stress on poor sleep quality was mediated by coping strategies, especially by avoidance. Thus, further research should consider the coping styles of individuals to reduce the influence of stress on sleep quality.
INTRODUCTION
Sleep quality is a complex concept defined as subjective satisfaction with overall sleep and ability in daytime function [1]. The effect of sleep quality on mental health has been reported in the nonclinical population and patients with many types of physical diseases [2,3]. Poor sleep quality can also be attributed to depression and anxiety, which can negatively influence quality of life [4,5]. Prior studies have also shown that individuals with poor sleep quality tend to have impaired memory function and academic output [6,7].
Several factors are known to contribute to poor sleep quality [8]. Stress, defined as disruptive physiological and psychological reactions to events that threaten an individual’s ability to cope, has been found to have a directional relationship with poor sleep quality in the prospective studies [9,10], and the impact of psychological stress on sleep was reported in the prior studies recruiting civil servants. In Japanese civil workers aged 35 years and over, high perceived stress increased the possibility of poor quality of sleep and the odds ratio was 2.96 [11]. And Hansen et al. [12] found the association between poor sleep quality and low level of morning salivary cortisol, which is thought as related to experiencing a stressful situation, among Denmark public officials.
Coping could be described as the process of deciding how to respond to stressful events after appraising them [13], and the individuals’ preference for choosing certain types of coping skills may affect the relationship between stress and sleep. For this reason, Harvey et al. [14] emphasized the role of coping strategies for understanding interindividual differences in sleep. Specifically, the previous study suggested that escape-oriented avoidant strategies influence negatively on initiating sleep, and active approach coping was not related to sleep quality, conversely [15,16]. Another study revealed that problem-focused coping has an association with less adequate sleep [17], but the opposite results for same coping strategies as the protective factor for stress have been also reported [18]. In seventy patients with systemic lupus erythematosus, poor sleep quality was related to self-blame and emotion-focused coping [19].
However, the effect of each coping strategy from prior studies was shown too diversely to prevent the broad application of the models with coping skills on sleep. This may be because previous studies analyzed coping strategies based on somewhat arbitrary theoretical or conceptual classification rather than based on statistical analysis. In addition, prior data focused on pathological conditions such as sleep disorders or insomnia patients, and there was a limitation to broadening the scope of application of the results to the population with sleep problems that are insufficient for diagnosis. Nevertheless, little data delineate the role of coping skills between stress and sleep quality. To our knowledge, only Morin et al. [20] reported that controlling stressful events could help enhance sleep quality and that coping skills have a mediating role between stress and sleep.
Hence, we set a hypothesis that each coping strategy would mediate differently the association between stress and sleep quality and this might induce the different impacts of stress on sleep in individuals among civil servants. To prove our hypothesis, we explored the status of perceived stress and sleep quality in the non-clinical population and evaluate the mediating role of coping strategies that are categorized by statistical analysis, between perceived stress and sleep quality. And the additional analysis was performed to determine the sex differences for the mediation effect of coping skills between them.
METHODS
Study design and participants
Our cross-sectional study recruited the participants from a group of employees in the city hall of Suwon, Gyeonggi-do, South Korea. Our study population contains civil officials in all departments, from the finance and accounting sector to welfare, education, environment, and transportation. Their working environment and hours varied from office workers to field workers, and from daytime regular work to shift work. Informed consent form and self-report questionnaires were provided to all participants through an online survey using the intranet network system of the city hall. Participants were included if they were between 18 and 70 years old and expressed their agreement to participate in this survey. Subjects who did not complete the whole questionnaire or did not provide consent for this study were excluded. The whole data collection procedure was done from September 2018 to February 2019. The study has been approved by The Catholic University of Korea St. Vincent’s Hospital Institutional Review Board (VC19QISI0238).
Measures
Demographic characteristics
We collected the following general information: age, sex, height, body weight, marital status, and amount of education. Body mass index (BMI) was calculated from height and body weight.
Dependent variable: perceived stress
We assessed the perception of stress with the Perceived Stress Scale-10 (PSS-10). The questionnaire is composed of 10 items that evaluate the degree to which respondents judge life events as stressful during the preceding month [21]. Each item evaluates how unpredictable, uncontrollable, and overloaded events were experienced by respondents. In the Korean version of the PSS-10, which was validated by Lee et al. [22], questions 1, 2, 3, 6, 9, and 10 are positive questions (0=not at all, 1=almost, 2=sometimes, 3=often, 4=very often), and items 4, 5, 7, and 8 are scored as negative questions. The total score ranges from zero to forty, with a high score indicating that the respondent is suffering severely from stress. The Cronbach’s alpha of the Korean version of the scale was 0.819, and test–retest reliability was 0.66 (p=0.01).
Independent variable: sleep quality
Sleep quality was evaluated with the Pittsburgh Sleep Quality Index (PSQI). It uses 19 self-rated items categorized into seven components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleeping medication, and daytime dysfunction. Every component is scored from zero to three points [23]. A score of zero indicates having no difficulty with sleep, and a score of three means serious difficulty. The total score of zero to twenty-one for the PSQI is determined by adding up all seven sub-domain scores. Sohn et al. [24] validated the Korean version of the PSQI.
Potential mediating variables: coping strategy
To estimate participants’ coping strategies, we used a simplification of the 60-item Coping Orientation to Problems Experienced (Brief COPE) inventory developed by Carver [25]. The Brief COPE uses 28 items classified into 14 coping strategies of 2 items each on a 4-point Likert scale. The higher the score, the more a particular coping strategy is used. The 14 coping strategies in the scale are self-distraction, active coping, denial, substance use, use of emotional support, use of instrumental support, behavioral disengagement, venting, positive reframing, planning, humor, acceptance, religion, and self-blame. Prior studies regarding coping strategies have used all 14 coping strategies in the scale or several coping styles categorized following conceptual or theoretical models by authors. These might limit the ability of researchers to quantify the application of each strategy. To diminish the limitation, we used a 4-factor structure for the Brief COPE validated by Baumstarck et al. [26]. They structured all 28 items of the inventory into four dimensions: seeking social support (8 items), problem solving (4 items), avoidance (10 items), and positive thinking (6 items). The score of each dimension is summed for the statistical analysis. In this study, we used the Brief COPE inventory translated by Joo [27], and the Cronbach’s alpha of the scales was 0.901.
Statistical analysis
The demographic and clinical characteristics were described as the mean±standard deviation or percentage in the study. First, the general characteristics were tested using t-test and chi-square test to identify significant differences according to gender. Second, we conducted a preliminary correlation analysis of perceived stress, sleep quality, and the four coping styles. To determine the linear relationships among them, we treated the total scores of the PSS-10, PSQI, and each coping style as continuous variables and calculated the Spearman correlation coefficient. Third, we ran a multiple parallel mediator model to examine their combined mediating effect on the association between perceived stress and sleep quality with the PROCESS macro for SPSS (IBM Co., Armonk, NY, USA) using the script described by Hayes [28]. As it is shown in Figure 1, we considered the total score of the PSS-10, indicating perceived stress, as the independent variable and the summed score of the PSQI, which the higher the PSQI score is, the worse sleep quality would be, as the dependent variable. It was supposed that the four coping styles, including 1) seeking social support, 2) problem-solving, 3) avoidance, 4) positive thinking, would mediate the relationship between perceived stress and sleep quality. 95% confidence intervals (CI) were demonstrated to show indirect effects, following the suggestion of Preacher and Hayes [29]. Age and the period of education were set as covariates, and the number of bootstrapping repetitions was 5,000. Fourth, to confirm the differences in the mediating effect of coping skills according to gender, subjects were divided by gender, and a subgroup analysis was conducted. The bootstrapping samples and covariates in this step were the same as the prior multiple mediator model. We analyzed the collected data using SPSS software 21.0 (IBM Co.), and two-sided p-values less than 0.05 was considered significant. The estimated sample size was calculated by Daniel’s method and adjusted for the population of the study [30], and the estimation of sample size was 299.
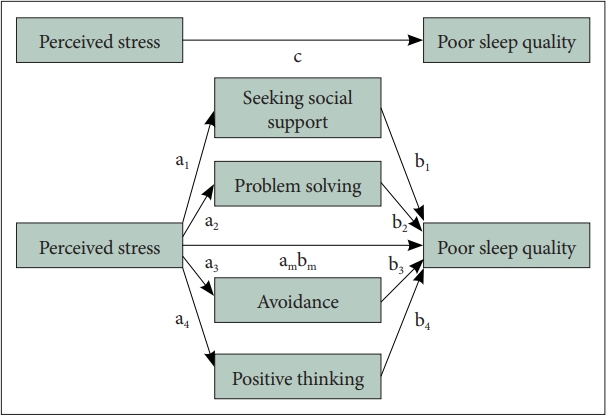
A conceptual diagram of the parallel multiple mediation model. a, the effect of perceived stress effect on mediators (coping skills); b, the effect of a mediator variable on the sleep quality; c, total effect of perceived stress on sleep quality; ambm, the indirect effect of perceived stress on sleep quality through proposed mediators.
RESULTS
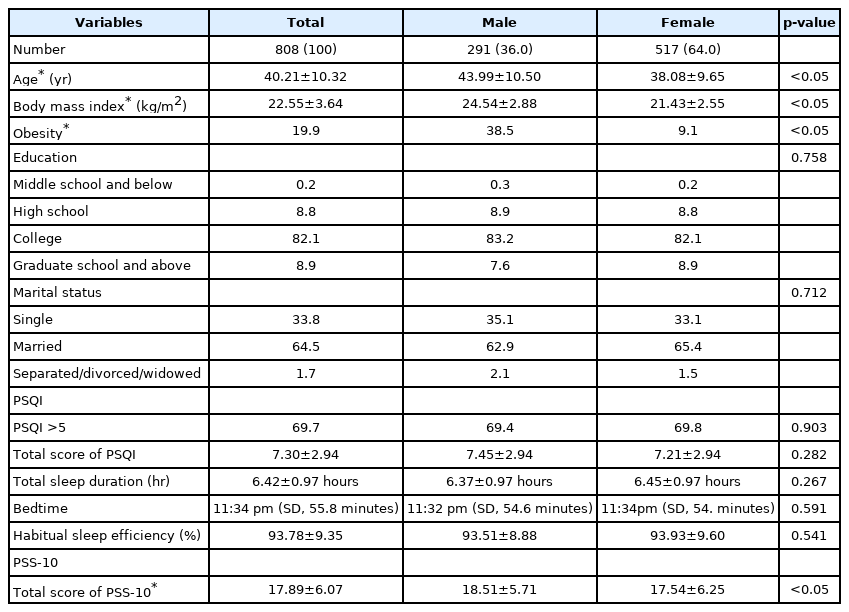
Demographic and clinical characteristics of the participants
Of the 4,072 employees of Suwon city hall, 811 individuals agreed to enroll in our study and responded to the questionnaires, for a response rate of 19.9%. During the data review, 3 subjects were excluded due to missing responses, so the results from 808 participants were analyzed. The mean age of participants was 40.21±10.32 years, with males accounting for 36.0% of the total sample. The average BMI among participants was 22.55±3.64 kg/m2, and 19.9% of participants were obese. The average PSQI score was 7.30±7.94, and 69.7% reported a PSQI score exceeding 5, indicating that their sleep quality was poor. The total score of the PSS-10 was 17.89±6.07 (Table 1). In comparison with female participants, male responders were significantly older (male, 43.99±10.50 years; female, 38.08±9.65 years; p<0.05) and reported higher score of PSS-10 (male, 18.51±5.71; female, 17.54±6.25; p<0.05). And we found that there was a significant difference in the BMI between the male and female subgroup (male, 24.54±2.88 kg/m2; female, 21.43±2.55 kg/m2; p<0.05), and the proportion of obesity among participants was larger in the male subjects (male, 38.5%; female, 9.1%; p<0.05). However, the level of education, marital status, and habitual sleep parameters (the PSQI score, total sleep duration, bedtime, habitual sleep efficiency, the ratio of participants whose PSQI score more than five) were not significantly different between the two subgroups.
Preliminary correlation analysis
A Pearson’s correlation analysis of perceived stress, poor sleep quality, and the four coping strategies is presented in Table 2. We found that the total score of PSS-10 correlated positively the PSQI score (r=0.544, p<001), meaning the correlation of perceived stress and poor sleep quality. Also, perceived stress had a significantly positive correlation with the avoidance coping strategy (r=0.463, p<0.001) and negative correlations with problem solving (r=-0.133, p<0.001) and positive thinking (r=-0.195, p<0.001). Among the four coping styles, avoidance (r=0.327, p<0.001) was positively correlated with the PSQI score, and positive thinking (r=-0.077, p=0.028) was negatively correlated with the PSQI score. In other words, avoidance correlated with poor sleep quality but positive thinking with better sleep quality. All of the coping strategies were significantly correlated with one another.
Results of the multiple mediation analysis for the entire participants
Results from the mediation analysis for the whole population were illustrated in Figure 2. First, our four potential mediators were regressed onto perceived stress (a path). Among the mediators, problem solving (a2=-0.040, standard error [SE]=0.016, p=0.014, CI=-0.072 to -0.008) and avoidance (a3=0.349, SE=0.023, p<0.001, CI=0.303 to 0.394) and positive thinking (a4=-0.092, SE=0.021, p<0.001, CI=-0.133 to -0.051) were significantly associated with perceived stress. But social support (a1=0.018, SE=0.026, p=0.487, CI=-0.032 to 0.068) did not show significant association with perceived stress.

The multiple mediation model of relationships between perceived stress, four proposed mediators, and poor sleep quality for the entire participants. All mediated effects were estimated using PROCESS macro in SPSS (IBM Co.). *p<0.05; **p<0.01; ***p<0.001. a, perceived stress effect on mediators (coping skills); b, association between mediators and sleep quality; ambm, the total indirect or ‘mediated’ effect of a combination of four coping skills on the relationship between perceived stress and poor sleep quality; SE, standard error; CI, confidence interval.
Next, we examined the associations between all proposed mediators and poor sleep quality (b path). Results indicated that only avoidance (b3=0.065, SE=0.025, p=0.009, CI=0162 to 0.114) had a significant positive association with poor sleep quality. And social support (b1=-0.013, SE=0.029, p=0.697, CI=-0.068 to 0.046), problem solving (b2=0.043, SE=0.047, p=0.365, CI=-0.050 to 0.135), and positive thinking (b4=-0.015, SE=0.037, p=0.692, CI=-0.068 to 0.058) was not significant predictors for poor sleep quality.
Finally, the total effect of perceived stress on poor sleep quality was tested (c path), and we found that the higher perceived stress was associated with worse sleep quality (c=0.263, SE=0.015, p<0.001, CI, 0.234 to 0.292). From the analysis for the total indirect effect of perceived stress on poor sleep quality (ambm path), perceived stress predicted worse sleep quality, and a group of four coping strategies mediated the relationship between perceived stress and poor sleep quality (ambm=0.022, boot SE=0.010, CI, 0.004 to 0.043).
Results from the multiple mediation analysis of the subgroups
To elucidate the sex difference of the mediation effect of coping strategies, an additional subgroup analysis was conducted with the same procedure for the entire subjects (Figure 3). In the male subgroup, the regression test for a path showed a significant association between avoidance and perceived stress (a3=0.357, SE=0.043, p<0.001, CI=0.273 to 0.441). Other three proposed mediators failed to their significant relationship to perceived stress; social support (a1=0.070, SE=0.045, p=0.124, CI=-0.019 to 0.158), problem solving (a2=-0.043, SE=0.030, p=0.153, CI=-0.102 to 0.016), and positive thinking (a4=-0.042, SE=0.038, p=0.278, CI=-0.117 to 0.034). However, there was no significant predictor for poor sleep quality among coping strategies (b path). More specifically, social support (b1=-0.026, SE=0.052, p=0.614, CI=-0.127 to 0.075), problem solving (b2=0.0411, SE=0.079, p=0.604, CI=-0.114 to 0.197), avoidance (b3=0.036, SE=0.041, p=0.372, CI=-0.044 to 0.116), and positive thinking (b4=-0.012, SE=0.066, p=0.856, CI=-00.27 to 0.537) had a positive directional relationship to poor sleep quality, but found out as insignificant. The total effect of perceived stress was significantly associated with poor sleep quality (c path) in the male subgroup (c=0.278, SE=0.026, p<0.001, CI=0.228 to 0.329). And regarding the indirect effect of perceived stress on poor sleep quality (ambm path), zero was placed within the CI of the association between them (ambm=0.089, boot SE=0.017, CI=-0.024 to 0.044), meaning its insignificancy.
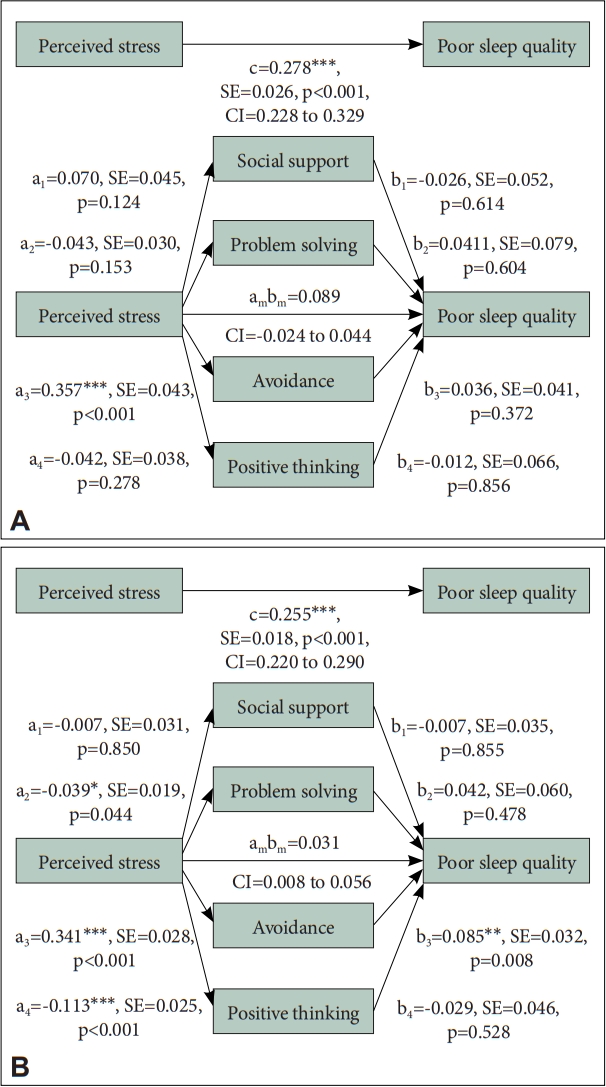
Results from the multiple mediation analysis of the male and female subgroup. A: The multiple mediation model of the male subgroup. B: The multiple mediation model of the female subgroup. All mediated effects were estimated using PROCESS macro in SPSS (IBM Co.). *p<0.05; **p<0.01; ***p<0.001. a, perceived stress effect on mediators (coping skills); b, association between mediators and sleep quality; ambm, the total indirect or ‘mediated’ effect of a combination of four coping skills on relationship between perceived stress and sleep quality; SE, standard error; CI, confidence interval.
From the analysis of a path in the female participants, the higher use of problem solving (a2=-0.039, SE=0.019, p=0.044, CI=-0.077 to -0.001) and positive thinking (a4=-0.113, SE=0.025, p<0.001, CI=-0.162 to -0.065) was related to the lower level of perceived stress. And the direction was opposite in the association between avoidance and perceived stress (a3=0.341, SE=0.028, p<0.001, CI=0.280 to 0.395). Among the relationship of four coping skills and poor sleep quality (b path), avoidance remained its significant association on poor sleep quality (b3=0.085, SE=0.032, p=0.008, CI=0.023 to 0.147), unlike the male subgroup. Social support (b1=-0.007, SE=0.035, p=0.855, CI=-0.076 to 0.063), problem solving (b2=0.042, SE=0.060, p=0.478, CI=-0.074 to 0.159), and positive thinking (b4=-0.029, SE=0.046, p=0.528, CI=-0.119 to 0.061) did not have the significant associations with poor sleep quality in the female group. Perceived stress showed its significant relationship with poor sleep quality in the female group, as well (c path; c=0.255, SE=0.018, p<0.001, CI=0.220 to 0.290), and results of ambm path showed a positive and significant association between them (ambm=0.031, boot SE=0.012, CI=0.008 to 0.056).
DISCUSSION
In this study, we examined the degree of perceived stress and sleep quality status in a nonclinical population to identify the association between perceived stress and poor sleep quality and the mediation effect of different coping strategies in that association. The mean PSS-10 score in our population was 17.89±6.07, which is comparable to the rates in recent studies conducted in the general population, supporting the generalizability of our results [31]. However, we found that 69.7% of our respondents reported poor sleep quality, which is surprisingly higher than recent data reported in a healthy population, which was between 22% and 36% [32,33]. A discrepancy could be caused by short sleep duration among our participants. The PSQI results indicated that participants usually slept 6.42±0.97 hours a day, possibly because of their late bedtime, around 11:34 pm. The result was consistent with the previous data finding that the sleep duration of civil workers was the shortest among many professions [34]. And short sleep duration may be the result of the long working hours, which is popular in Korean civil workers [35].
Male participants were older and fatter, and their rate of obesity was larger, compared to female subjects. The differences in the age distribution of each subgroup might explain the results. Because the male gender itself and older age are related to an increase in the prevalence of obesity, as shown in the past studies [36]. And it was found that male subjects were suffering from higher levels of stress than females, not consistent with other studies revealing that females are vulnerable to work and family stress [37]. The inconsistency might be originated from confounding factors that were not analyzed in our study. For instance, several previous studies found that higher job rank is associated with larger levels of stress [38]. Considering that the job rank of the subjects was generally determined based on their seniority, we could expect that males might be positioned at the higher rank for the jab, and it might affect the result in our study. Moreover, working environment, working schedule, the experience of violence in the workplace could be associated with higher levels of perceived stress [39].
Consistent with previous research, a significant and positive association between perceived stress and poor sleep quality was repeatedly found in the study. And a combination of four coping styles significantly mediated the relationship between perceived stress and poor sleep quality, and only avoidance maintained its significance through all regression analyses. It is plausible that perceived stress might be linked to poor sleep quality through the use of avoidant coping skills. This result is supported by the prior study. Hoyt et al. [40] found that avoidance negatively influenced the severity of difficulty falling asleep, nocturnal awakening, and early morning awakening, whereas approach-oriented coping did not affect sleep quality. Among prostate cancer survivors, an avoidant coping strategy was related to altered diurnal rhythms of cortisol. Specifically, the group that preferred avoidant coping showed less diurnal fluctuations of cortisol secretion than the group using avoidance less often, which could indicate prolonged stress throughout the day. Approach-oriented coping, on the other hand, was not related to cortisol slope, which is consistent with the result of the prior study [41].
The total effect and indirect effect of perceived stress on poor sleep quality remained significantly in the male and female subgroups. However, avoidance coping mediated the relationship of stress and sleep quality only in females, and more use of avoidance was associated with the worse sleep quality. In the male subjects, there was a significant and positive relationship between perceived stress and poor sleep quality, but the association was not significant between avoidance and sleep quality. The longitudinal study for coping styles reported that the use of avoidance strategies decreased over the follow-up period, and this might attenuate the mediating effect of avoidance in the older male participants [42].
To our knowledge, this is the first study to elucidate the mediating effect of coping styles on the relationship between perceived stress and sleep quality. It is a strength of this study that our four coping strategies were statistically validated. However, the results of our study do have several limitations. First, its cross-sectional design prevents us from drawing any conclusive causal relationships between perceived stress and poor sleep quality. Poor sleep quality among the participants might have been a cause of their perceived stress in a reversal of our proposed model. Second, there could be concerns in generalizing our results related to the study sample. Considering the previous study by Eslaminejad et al. [43] which showed that the education level and professional status are associated with certain types of coping skills, our samples from a single organization might not reflect the mediation effect of coping between stress and sleep quality in the general population. Third, a low response rate could raise selection bias in our results. It is because those with relatively severe sleep problems were more likely to participate in the response. Therefore, cautious attention should be taken in interpreting our results and future research including a large sample from the heterogeneous group. Fourth, our analysis was performed using subjective, self-rated measurements without the support of objective data from actigraphy or polysomnography. Lastly, our analysis did not include the working schedule and working environment, which could affect the sleep quality and level of stress. It may have interrupted a more accurate approach to the relationship between the variables.
In conclusion, the results of our study indicate that the level of perceived stress is significantly associated with the degree of poor sleep quality and that the avoidance coping style negatively mediates that association. And the mediation effect of avoidance was significant only in the female subjects, not in males. However, few previous data were available to establish the mediating effects of coping styles on the association between stress and sleep quality. Therefore, further studies are still needed to determine those effects and establish proper interventions to modify the relationship between stress and sleep quality.
Notes
Availability of Data and Material
The data for the study are available from the corresponding author upon reasonable request.
Conflicts of Interest
Yoo Hyun Um, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Ho-Jun Seo, Sung Min Kim, Yoo Hyun Um, Jong-Hyun Jeong. Data curation: Sung Min Kim, Ho-Jun Seo, Tae Won Kim. Formal analysis: Sung Min Kim, Yoo Hyun Um, Ho-Jun Seo. Methodology: Sung Min Kim, Yoo Hyun Um, Ho-Jun Seo. Project administration: Sung Min Kim, Ho-Jun Seo, Seung-Chul Hong, Jong-Hyun Jeong. Resources: Ho-Jun Seo, Seung-Chul Hong, Jong-Hyun Jeong. Software: Sung Min Kim, Seung-Chul Hong. Supervision: Seung-Chul Hong, Jong-Hyun Jeong, Ho-Jun Seo. Validation: Sung Min Kim, Yoo Hyun Um. Visualization: Sung Min Kim, Tae Won Kim, Seung-Chul Hong. Writing—original draft: Sung Min Kim. Writing—review & editing: all authors.
Funding Statement
None
Acknowledgements
We would like to thank all respondents and participants involved in data collection and processing for this study.