Sleep and Mental Health Among Adolescents During the COVID-19 Pandemic
Article information
Abstract
Objective
This study aimed to investigate the association of sleep with mental health among Korean adolescents during the coronavirus disease (COVID-19) pandemic.
Methods
Using data from the 16th Korea Youth Risk Behavior Web-Based Survey (2020) of 46,475 adolescents, we examined sleep duration and satisfaction and examined mental health for depressive symptoms, anxiety, and suicidal ideation. The data were analyzed using complex sample descriptive statistics and a multiple logistic regression model.
Results
In 2020, the average sleep duration was 6.3 hours, and the sleep satisfaction rate was 30.8%. Depressive symptom and suicidal ideation rates were 24.2 and 10.3, respectively. These values are slightly better than those previously reported, before COVID-19. However, poor sleep was still associated with mental health. The likelihood of mental health problems was higher among those who slept for six hours or less than for those who slept for eight hours or more (p<0.05). Additionally, the results showed that the lower the sleep satisfaction, the higher the likelihood of mental health problems (p<0.05).
Conclusion
Even after the COVID-19 outbreak, poor sleep associated with mental health problems remained as high as before the outbreak of COVID-19.
INTRODUCTION
On March 11, 2020, the World Health Organization declared that the coronavirus disease (COVID-19) outbreak was a pandemic [1]. Many countries were forced to shut down most of public life, including schools [2]. COVID-19 has affected the lives of adolescents in various ways in Korea, just as in other countries. The Korean government implemented social distancing measures such as school closure to prevent the spread of COVID-19 [3], as well as restrictions on recreational spaces and activities that limited the options for physical activity, time spent outside the home, and respite care [4].
Sleep duration and satisfaction in adolescents deteriorated substantially during lockdown. Thus, COVID-19 has changed adolescents’ sleep patterns [5]. Remote learning during COVID-19 resulted in later bedtimes and wake times for adolescents [6]. In addition, adolescents had increased difficulties in initiating and maintaining sleep, and experienced an increase in delayed sleep/wake behaviors during the pandemic [7].
Insufficient sleep duration is negatively associated with perceived mental health [8]. Insufficient sleep affects cognition, mood, and judgment, and causes sleepiness, microsleep, tiredness, and fatigue [9]. Insufficient sleep duration is common in adolescents and has been associated with increases in poor school performance and poor mental health, including mood swings, anxiety, and suicidality [10]. Low sleep satisfaction increases irritability and negative emotions [11]. Furthermore, adolescents with lower sleep satisfaction tend to demonstrate high levels of psychosocial distress, manifesting as increased anxiety, tension, depression, and general health problems [12].
The rapid rise in the number of infected cases and deaths, disruption of daily routines, home confinement, fear of infection, and social distancing from peers and friends have reduced mental health among adolescents [13]. At the same time, however, these social distancing measures have led to less academic pressure and less peer conflict and bullying [14]. Moreover, physical exercise, access to entertainment, positive familial relationships, and social support were associated with better mental health outcomes. [4] Spending time at home can, thus, have both positive and negative influences on the mental health of adolescents [15].
Poor mental health in adolescents is a common and serious issue and is associated with serious dysfunction in adult life [16]. Overall, the global onset of mental health problems occurs before age 14 in one-third of individuals, and before age 18 in almost half (48.4%) the population [17]. Furthermore, poor mental health accounts for 13% of the global burden of mental health problems in 10–19 year olds [18].
Depressive symptoms and anxiety are widespread among adolescents today [19]. In 2020, an estimated 27.0% of the Korean population aged 11–19 years had experienced depressive symptoms [20]. In 2020, 26.1% of Korean adolescents (11–19 years) had experienced anxiety [21]. Anxiety is often chronic and recurring [22]. Anxiety impairs functioning and hampers general health, resulting in financial, interpersonal, and educational difficulties [23].
Globally, suicide is the fourth leading cause of death among 15–19-year-olds. [18] Korea has the highest suicide rate among the Organization for Economic Cooperation and Development member countries [24]. Suicide is the leading cause of death among Korean adolescents. According to Statistics Korea, the suicide rate among adolescents increased from 8.7 per 100,000 people in 2018 to 9.4 per 100,000 people in 2019 [25,26]. Suicide is strongly associated with suicidal ideation and attempts [27].
Sleep (sleep duration and satisfaction) and mental health (depressive symptoms, anxiety, and suicidal ideation) are considered to be associated in adolescence [28-30]. Although the association between sleep and mental health has been extensively studied [12,31], the COVID-19 pandemic’s effect on this relationship remains unclear in Korea.
Considering these factors, it is likely that there have been many changes in the life patterns and mental health of adolescents since the COVID-19 outbreak. Therefore, we used post-COVID-19 data to determine the association between sleep and mental health in Korean adolescents. This study hypothesized that low sleep satisfaction is associated with increased depressive symptoms, anxiety, and suicidal ideation in adolescents during the COVID-19 pandemic.
METHODS
Study population and data
This study used data from the 16th Korea Youth Risk Behavior Web-Based Survey (KYRBS), which was conducted from August 3 to November 13, 2020 by the Korea Disease Control and Prevention Agency (KDCA). The KYRBS’ purpose is to identify health behaviors under present conditions, report health indicators to plan and appraise health promotion for adolescents and compare health indicators of adolescents from different countries. The KYRBS received the KDCA approval (2014-06EXP-02-P-A) in 2014. Ethics approval for the KYRBS is waived by the KDCA’s Institutional Review Board in accordance with the Bioethics and Safety Act of 2015. Everyone who participates in the KYRBS provides informed consent. The KYRBS complies with the Declaration of Helsinki.
The KYRBS is an anonymous, self-administered, structured questionnaire with a complex research design, which includes multistage sampling, stratification, and clustering. The stratified cluster random sampling method was used for sampling; the primary sample unit was a school and the secondary sample unit was a class. For the primary sampling, a sample school was selected as the permanent random number sampling method for each cluster. For the secondary sampling, one class was randomly extracted for each grade from the selected sample school. All students in the class selected as the sample class were surveyed, and exceptional children and students with dyslexia who were unable to participate in the survey on their own were excluded from the sample. The KYRBS uses an online survey system that does not allow respondents to proceed to the next section of the questionnaire unless all questions in the current section are answered. Responses with logical errors and outliers are processed as missing values. The questionnaire contains approximately 120 items across 15 categories, including demographic characteristics and health-associated behaviors. Students in grades 7–12 were the target population in our study.
Measurements
Dependent variables
The dependent variables were mental health indicators, including depressive symptoms, anxiety, and suicidal ideation. Depressive symptoms were assessed in the KYRBS through the question, “Have you experienced sadness or hopelessness enough to stop your daily routine for two weeks in the past 12 months?” A single item depressive symptoms measure like the mentioned question had relatively high levels of specificity in detecting non-cases, but poor sensitivity [32].
Anxiety was measured using a seven-item generalized anxiety disorder scale (GAD-7). The GAD-7 is a newly added measure on the KYRBS to assess anxiety. It has high internal consistency, good reliability, and convergent validity [33], and has been shown to have acceptable reliability for detecting clinically significant anxiety symptoms in Korean adolescents [34]. The Cronbach’s alpha for each of the seven items of the GAD-7 was 0.90. A maximum alpha value of 0.90 has been recommended [35]. GAD-7 scores ≥10 represent moderate anxiety, and scores ≥15 represent severe anxiety, with good sensitivity [36]. Furthermore, in this study, the cutoff score was ≥10 on GAD-7, as this threshold provides a consistent reflection of anxiety levels. The mean±standard deviation of the anxiety scores were 3.9±4.4. However, based on the cut of score, 4,913 (10.6%) were defined as being anxious.
Suicidal ideation was assessed by the question, “Have you seriously considered suicide in the past 12 months?” Depressive symptoms and suicidal ideation were categorized based on whether respondents answered these questions with yes or no.
Independent variable (variable of interest)
The variable of interest was sleep, including sleep duration and sleep satisfaction. Sleep duration was assessed through the question “During the last 7 days, what time did you usually wake up and go to bed?” Sleep duration was calculated by subtracting the bedtime from the waking time on weekdays and was categorized as <6 h, ≥6 h and <8 h, or ≥8 h. Sleep satisfaction was assessed by the question “During the last 7 days, how satisfied have you felt with the duration of your sleep, in terms of fatigue recovery?” The answers ranged from very sufficient, sufficient, just enough, not enough, and not enough at all. In this study, we reclassified very sufficient and sufficient as sufficient, and not enough and not enough at all as not enough.
Covariates
The covariates were sex (male/female), school (middle/high), residential area (metropolitan/urban/rural), subjective household economic status (high/middle/low), co-residence with parents (yes/no), subjective academic performance (high/ middle/low), subjective health status (high/middle/low), alcohol consumption (yes/no), and smoking status (yes/no).
Statistical analyses
The independent variable and covariates were compared using the chi-squared test to determine their associations with mental health. Multiple logistic regression analysis was performed to evaluate the association between sleep and mental health. The results were reported as odds ratios (ORs) and confidence intervals (CIs). Differences were considered statistically significant if the p-values were <0.05. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
RESULTS
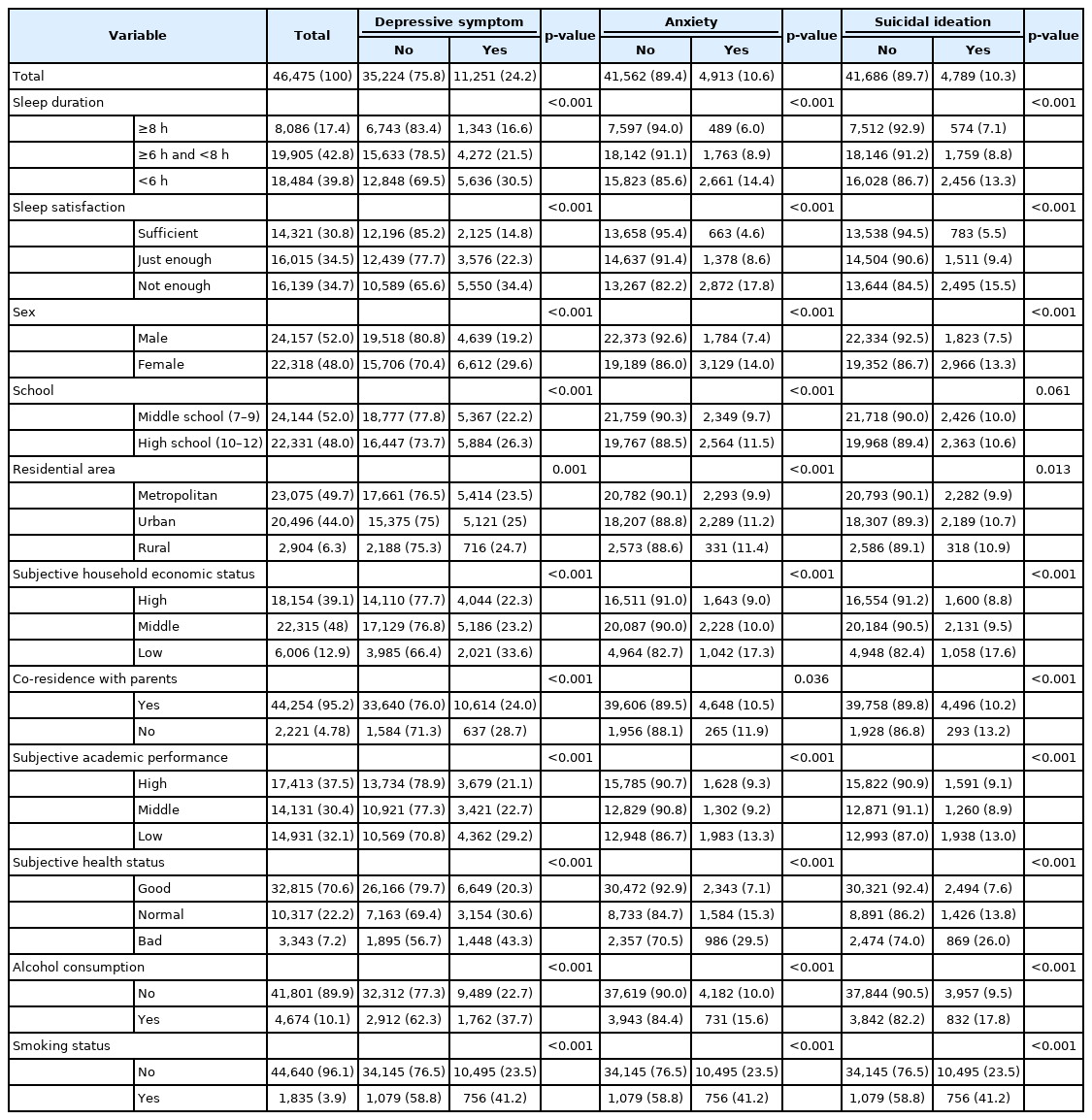
Data of 46,475 adolescents were analyzed. Among the participants, 8,086 (17.4%), 19,905 (42.8%), and 18,484 (39.8%), students slept for ≥8 h, ≥6 h and <8 h, and <6 h on average during the week, respectively. Furthermore, 14,321 students (30.8%), 16,015 (34.5%), and 16,139 (34.7%) students reported sufficient sleep, just enough sleep, and not enough sleep satisfaction, respectively. Regarding mental health-related variables, 11,251 (24.2%), 4,913 (10.6%), and 4,789 (10.3%) participants reported experiencing depressive symptoms in the past 12 months, anxiety during the last two weeks, and seriously considering suicide in the past 12 months, respectively.
Adolescents who reported insufficient sleep duration had poor mental health. Regarding depressive symptoms, 1,343 (16.6%), 4,272 (21.5%), and 5,636 (30.5%) participants slept for ≥8 h, ≥6 h and <8 h, and <6 h, respectively. Regarding anxiety, 489 (6.0%), 1,763 (8.9%), and 2,661 (14.4%) participants slept for ≥8 h, ≥6 h and <8 h, <6 h, respectively. Similarly, regarding suicidal ideation, 574 (7.1%), 1,759 (8.8%), and 2,456 (13.3%) participants slept for ≥8 h, ≥6 h and <8 h, and <6 h, respectively. Thus, the lower the sleep satisfaction, the higher the risk of mental health problems. Depressive symptoms were reported by 2,125 (14.8%), 3,576 (22.3%), and 5,550 (34.4%) participants with sufficient, just enough, and not enough sleep satisfaction, respectively. A total of 663 (4.6%), 1,378 (8.6%), and 2,872 (17.8%) participants with sufficient, just enough, and not enough sleep satisfaction, respectively, reported anxiety. Suicidal ideation was reported by 783 (5.5%), 1,511 (9.4%), and 2,495 (15.5%) participants who were satisfied with sleep, had just enough sleep satisfaction, and did not feel satisfied enough, respectively (Table 1).
Adolescents with poor mental health (depressive symptoms, anxiety, suicidal ideation) were more among females, those who lived in urban or rural areas, and did not co-reside with parents; moreover, they had low subjective household economic status, low subjective health status, and drank alcohol and smoked as compared to those without poor mental health. More had depressive symptoms and anxiety among high school students, but the outcome of suicidal ideation was not significant. Subjective academic status was similar between the two groups.
Table 2 shows the association between sleep (sleep duration and sleep satisfaction) and mental health (depressive symptoms, anxiety, and suicidal ideation) after adjusting for the effects of covariates through the multiple logistic regression analysis results. Poor sleep significantly increased the odds of poor mental health. The likelihood of depressive symptoms was higher among those who slept for an insufficient duration than for those who slept for 8 hours or more (≥6 h and <8 h: OR=1.11, 95% CI=1.03–1.19; <6 h: OR=1.30, 95% CI=1.20– 1.41). Similar results were found for anxiety (≥6 h and <8 h: OR=1.15, 95% CI=1.03–1.28; <6 h: OR=1.36, 95% CI=1.21– 1.53) and suicidal ideation (<6 h: OR=1.24, 95% CI=1.11–1.38). Furthermore, the lower the sleep satisfaction, the higher the likelihood of depressive symptoms (just enough sleep satisfaction: OR=1.41, 95% CI=1.32–1.50; not enough sleep satisfaction: OR=2.20, 95% CI=2.06–2.34). Similar results were reported for anxiety (just enough sleep satisfaction: OR=1.59, 95% CI=1.44–1.76; not enough sleep satisfaction: OR=2.96, 95% CI=2.69–3.26) and suicidal ideation (just enough sleep satisfaction: OR=1.52, 95% CI=1.39–1.67; not enough sleep satisfaction: OR=2.18, 95% CI=1.99–2.39).
Regarding covariates, mental health in Korean adolescents was associated with sex, school, subjective health status, alcohol consumption, and smoking status and partially associated with residential area, subjective household economic status, co-residence with parents, and subjective academic performance.
DISCUSSION
To the best of our knowledge, this is the first study to identify an association between sleep (sleep duration and satisfaction) and mental health (depressive symptoms, anxiety, suicidal ideation) among adolescents in Korea after the COVID-19 outbreak. Furthermore, this study used a large sample of the 2020 KYRBS data, which was a national survey based on a sample of Korean adolescents. As hypothesized, poor sleep was associated with an increased probability of poor mental health. Our results show that adolescents who did not sleep long enough or who had lower sleep satisfaction had poor mental health. In addition, our study found associations of mental health with sex, school, subjective health status, alcohol consumption, and smoking status; however, mixed results were found for associations of mental health with residential area, subjective household economic status, co-residence with parents, and subjective academic performance.
Our findings are consistent with those reported by prior research [37,38]. Alvaro, Roberts, and Harris found that anxiety and depressive symptoms were associated with sleep duration among adolescents, suggesting that those who sleep less than the recommended hours are at higher risk for experiencing these mental health problems [39]. Guo et al. [40] found that mental health was associated with sleep satisfaction. Many prior studies suggest that both insufficient and excessive sleep may be associated with poor mental health [41,42]. However, we did not find any associations between excessive sleep and the measured outcomes. In our study, only 8,086 (17.4%) participants slept more than the recommended sleep duration level (>8 h). This may be because adolescents who sleep longer are more likely to meet the recommended sleep duration [12].
Furthermore, the covariates were consistent with those in previous studies [18,19,40]. However, although mental health problems are known to increase as age increases [17], our study found that high school students have lower mental health problems than middle school students. Puberty changes and the situation of middle school students facing adaptation with new status and expectations at the same time are related to unstable development of self-esteem [43], and these changes are likely to have served as a mechanism to amplify mental health problems in middle school students. Since the development of selfesteem shows a gradual increase during adolescence [44] mental health problems may be lower in high school students than in middle school students. Adolescents with middle subjective household economic status showed lower risk of depression than adolescents with high subjective economic status. This is different from the results of previous studies that showed that depression increases as the economic level decreases [40]. However, previous studies were conducted before COVID-19, and the KYRBS gathers self-reported data; there may be problems with its validity. Therefore, it is suggested that further research is needed.
In our study, the average sleep duration was 6.3 hours, and the sleep satisfaction rate was 30.8% in 2020. Additionally, depressive symptom and suicidal ideation rates were 24.2 and 10.3, respectively, in 2020. These values are slightly better than those previously reported before COVID-19. For example, the average sleep duration of adolescents was 6.3 hours on average and the sleep satisfaction rate of adolescents was 21.4% in 2019 [45]. Furthermore, the depressive symptoms and suicidal ideation rates of adolescents were 28.2% and 13.1%, respectively, in 2019 [45]. Adolescents mainly feel stressed and depressed because of external factors such as academic grades, studies, and relationships with peers [46]. The COVID-19 outbreak has led to the emergence of alternative teaching methods, such as digital classes, resulting in decreased anxiety, depression, and suicidal ideation among adolescents [47]. This is because social distancing has decreased academic pressure and peer conflict, and allowed greater flexibility and more opportunities for obtaining sufficient sleep, as less time is spent commuting to school [5,14]. Nevertheless, Korean adolescents still have poor mental health, and most do not meet the recommended sleep duration [48,49]. This can be attributed to the academic stress caused by excessive homework given to Korean adolescents engaging in extracurricular activities and competitive educational environments [49]. Additionally, this can be ascribed to increased screen time because of online lectures, and reduced daily structure and physical activity because of social distancing [50,51].
We found that there was still an association between poor sleep and mental health problems in adolescents after the COVID-19 outbreak. Therefore, for adolescents to maintain the recommended sleep duration and increase sleep satisfaction, public health approaches such as reducing academic stress and the use of electronic devices are needed [28,50]. Sleep hygiene education may be considered as a public health approach that may help improve sleep among adolescents [52]. It involves promoting good sleep habits in all aspects of life [53]. This encourages adolescents to build an exercise routine, reduce stress, and manage their sleep and nap times [54].
However, there were some limitations in our study. First, this study’s data were obtained from a cross-sectional survey; thus, the findings indicate only statistical associations and not causality. Second, as the data were self-reported online, survey respondents may have understated or overstated their responses. Third, although this study was based on a national survey, its results might have been influenced by selection or recall bias. For example, the survey did not include adolescents who had dropped out of school or faced expulsion. Fourth, the measures of depressive symptoms and suicidal ideation were not validated. Fifth, this study did not evaluate the severity of depressive symptoms, anxiety, and suicidal ideation. In the case of anxiety and suicidal ideation, the severity could not be confirmed because the survey itself asked only yes/no. The severity of anxiety can be evaluated; however, in this study, it was evaluated only as anxiety, following a prior study [36].
In conclusion, the findings show that, following the COVID-19 pandemic, poor sleep is associated with poor mental health, much as before the pandemic. Our results suggest a public health approach such as sleep hygiene education to help adolescents meet the recommended sleep duration and improve sleep satisfaction.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: all authors. Formal analysis: Do Hee Kim, Bomgyeol Kim. Methodology: Tae Hyun Kim, Sang Gyu Lee. Validation: Tae Hyun Kim, Sang Gyu Lee. Writing—original draft: Do Hee Kim. Writing—review and editing: Tae Hyun Kim, Sang Gyu Lee.
Funding Statement
None