No Effect of Serotoninergic Gene Variants on Response to Interpersonal Counseling and Antidepressants in Major Depression
Article information
Abstract
Objective
Gene variants within the serotonin pathway have been associated with major depressive disorder (MDD) treatment outcomes, however a possible different modulation on pharmacological or psychological treatments has never been investigated.
Methods
One hundred sixty MDD patients were partially randomized to either inter-personal counseling (IPC) or antidepressants. The primary outcome was remission at week 8. Five serotonergic polymorphisms were investigated (COMT rs4680, HTR1A rs6295, HTR2A rs2224721, HTR2A rs7997012 and SLC6A4 rs421417).
Results
IPC (n=43) and antidepressant (n=117) treated patients did not show any difference in remission rates at week 8 (corrected for baseline severity, age and center). None of the studied gene variants impacted on response and remission rates at week 8 neither in the IPC nor in the antidepressant group. An analysis of the whole sample showed a trend of association between rs7997012 AA genotype and a better treatment outcome.
Conclusion
Our study confirms that IPC is an effective psychological intervention comparable to antidepressants in mild-moderate MDD. Polymorphisms related to the serotonin system did not exert a major effect on clinical outcomes in none of the treatment groups.
INTRODUCTION
Major depressive disorder (MDD) is the most common psychiatric disorder (life-time prevalence: 12.8%), and it is responsible for the great burden linked to non-fatal health outcomes.1 After the introduction of antidepressant drugs in the '50, no substantial improvement in MDD clinical management was achieved, given the still unsatisfactory response and remission rates [47 and 33%, respectively, in the large Sequenced Treatment Alternatives to Relieve Depression (STAR*D) cohort].2 Nowadays, together with the introduction of innovative antidepressant molecules, the identification of reliable predictors of treatment response for the each subject is expected in order to provide a substantial improvement of MDD prognosis.
Among treatment options, selective serotonin reuptake inhibitors (SSRIs) are the first line treatment and psychological interventions such as inter-personal counseling (IPC) have been suggested to have comparative efficacy and effectiveness when compared to antidepressants (response rates are from 30% to 50% regardless the choice of pharmacotherapy or psychotherapy),3 particularly in moderate MDD. Combined treatment may provide a small advantage (with effect size estimated from 0.25 to 0.35), even if it does not seem to persist during medium-long follow-up and not to be significant in mild MDD.4 However no clear guideline is available to choose the best treatment in each patient, even if some clinical predictors of IPC vs. antidepressant pharmacotherapy efficacy have been proposed.5 Thus, further evidence is needed to better clarify the efficacy of brief psychotherapies vs pharmacological treatments and to identify reliable predictors of clinical outcomes.
Among predictors of treatment response, genetic factors are estimated to contribute for a substantial degree to the interindividual variability.6 Given that monoamines are pivotal in antidepressant response,7 genes related to the serotoninergic system are considered among the most promising candidates. Particularly, serotonin receptors, serotonin transporter and enzymes responsible for the metabolism of monoamines are involved in the regulation of the serotoninergic neurotransmission in the CNS.
The serotonin 2A receptor (coded by HTR2A gene) is expressed in all neocortical areas, in putative interneurons, hippocampus and prefrontal cortex.8 It is down-regulated by different classes of antidepressants in parallel with the improvement of clinical symptoms9 and some interesting polymorphisms were reported within HTR2A. Particularly, rs7997012 was strongly associated with citalopram response in the STAR*D study,10,11 even if other studies obtained inconsistent findings (negative results12-16 in the opposite direction17 or association only when considering the interaction with gender18). Rs2224721 harbored by the same gene was associated with the risk of bipolar disorder19 and was one of the two best predictors of escitalopram response in the GENDEP (Genome-based Therapeutic Drugs for Depression) sample,14 suggesting it as a promising target for further investigation.
A role of the HTR1A gene in antidepressant response has also been postulated because several antidepressants desensitize raphe 5-HT1A autoreceptors, leading to an enhancement of the 5-HT neurotransmission. Moreover there is evidence that the blockade of 5-HT1A autoreceptors may accelerate antidepressant effect.6 The most promising SNP within the gene is the rs6295 (1019C/G), since the G allele was associated with an up regulation of the expression of the receptor20,21 leading to the hypothesis that it may contrast the therapeutic effect of antidepressants through a higher number of inhibitory 5-HT1A autoreceptors. This hypothesis is supported by several pharmacogenetic studies,22-28 while some negative reports exist.16,29-32 Interestingly, an interaction with gender was reported for rs629533 as well as for rs7997012.
The serotonin transporter gene (SLC6A4) is probably the leading candidate as predictor of antidepressant response, since it codes for one of the main target of antidepressant drugs. Polymorphic variants within the promoter have gained particular attention, since their supposed effect on gene expression regulation.6 Research efforts were mainly directed towards the study of the insertion/deletion variant (5-HTTLPR), and to a less extent, rs25531, but the need to provide a better coverage of the region recently emerged. Rs4251417 harbored by this genomic region was found in linkage disequilibrium with 5-HTTLPR34 and its possible role in antidepressant response has not been investigated yet.
Finally, the catechol-O-methyltransferase (COMT) gene codes for an intracellular enzyme with a key role in the inactivation of monoamines. Rs4680 (Val108/158Met) is a functional polymorphism which Val/Val genotype catabolizes dopamine at up four times the rate of Met/Met homozygote.35 Given the close interactions between the serotonergic and dopaminergic systems, dopamine availability in some areas of the CNS such as the frontal cortex and the nucleus accumbens was reported to modulate antidepressant response.6 Pharmacogenetic findings about rs4680 mainly confirmed it plays a role in antidepressant response,36-41 while which genotype/allele is associated with poorer outcome still remains unclear.6 A sexually dimorphic effect was reported also for this polymorphism.40
The mechanisms behind the antidepressant efficacy of psychotherapy in MDD are less known. The main hypothesis is a direct effect on cognitive processes such as dysfunctional attitudes and negative automatic thoughts,42 but the knowledge about the molecular processes involved is poor. Anyway, improvement of cognitive measures is not different between patients treated with pharmacotherapy and psychotherapy,43 suggesting that ultimately common mechanisms mediate the efficacy of both therapeutic approaches. This is also supported by the evidence of monoamines balance modification during psychotherapy, involving in particular serotonin transporter activity.44,45
Given the reported unsolved issues, the present paper aims to study the role of HTR2A rs7997012 and rs2224721, HTR1A rs6295, SLC6A4 rs4251417 and COMT rs4680 on antidepressant efficacy in a sample of 160 MDD Italian patients, treated with IPC or antidepressants. No previous study investigated the possible effect of these polymorphism on IPC response.
METHODS
Sample
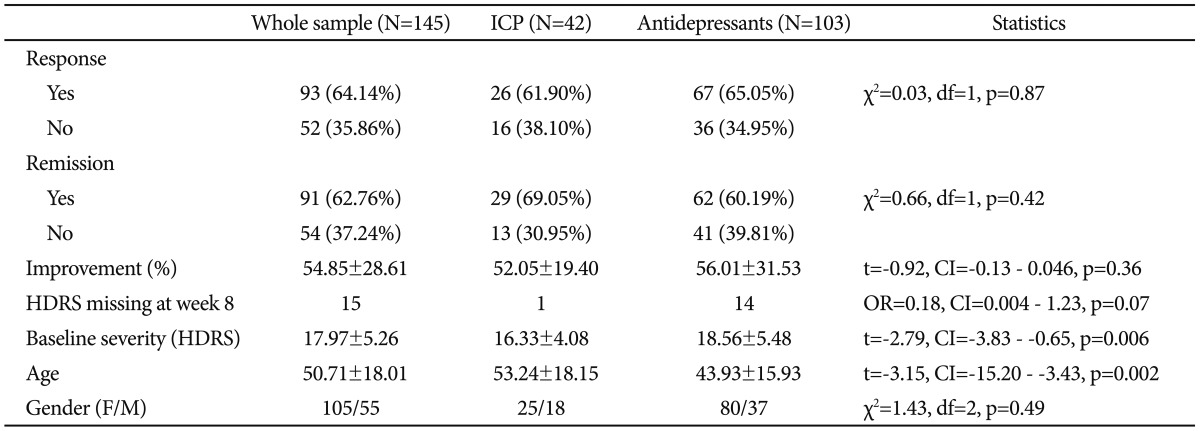
Patients aged 18 years or older with diagnosis of MDD (according to DSM-IV TR criteria), with a score ≥13 on Hamilton Depression Rating Scale (HDRS, 21-item version, in accordance to STAR*D criteria2), were eligible for inclusion. Any other psychiatric disorder as primary diagnosis (bipolar disorder included), comorbidity for substance abuse, cognitive impairment (Mini Mental State Evaluation <28), poor ability to participate to evaluations and current pregnancy or feeding were exclusion criteria. After a baseline assessment, eligible patients were partially randomized to a brief structured psychological intervention (IPC) or to antidepressant treatment (mainly SSRIs)(Table 1).46 Patients were collected in three centers: 35 were collected at the Neuroscience Department, Turin University, 41 at the Department of Health Sciences, Section of Psychiatry, University of Pavia and 84 at the Department of Biomedical and NeuroMotor Sciences, Bologna University. All patients collected at the Institute of Psychiatry, Bologna University were treated with antidepressants and not randomized.
Patients were carefully informed about all study procedures before signing written informed consent. Ethical approval was obtained from local research ethic committees.
Interpersonal counseling (IPC)
IPC is a brief manualized psychological intervention, derived from Interpersonal Psychotherapy (IPT). IPC has been adapted and tested on patients with depressive disorders, in association with pharmacological treatment or alone.47-50 It consisted of six thirty-minute sessions, with the initial session being longer, and is focused on patients' current psychological problems and social functioning and specifically on four interpersonal problem areas: prolonged grief, interpersonal disputes, role transitions and interpersonal deficits;51 patients are helped to identify effective strategies in order to deal with their interpersonal problems. To ensure the intervention's consistency, therapists attended a 3-day teaching seminar on IPC techniques and monthly group supervisions with videotaped sessions.
Evaluations
All patients were evaluated with both structured and unstructured interviews to obtain lifetime diagnoses assigned by two independent experienced psychiatrists, on the basis also of medical records, according to DSM-IV TR criteria. Current and lifetime Axis I and II diagnoses were assessed by Mini International Neuropsychiatric Interview (MINI) and structured clinical interview for DSM-IV TR Axis II Personality disorders. Cognitive impairment was assessed by Mini Mental State Examination (MMSE) in patients older than 60. Depressive symptoms were assessed at baseline and after 8 weeks through HDRS. Interrater evaluations were satisfactory (k>0.8).
Outcomes
The primary outcome was remission at week 8, defined according to standard criteria (HDRS score ≤7). The secondary outcomes were response (at least 50% reduction in HDRS score) and HDRS percent improvement at week 8.
Genotyping
Genomic DNA was purified from whole blood using the QIAamp DNA Blood Midi Kit (Qiagen, CA, USA), according to the manufacturer's protocol. Rs7997012 and rs2224721 (HTR2A, chr 5q11.2-q13), rs6295 (HTR1A, chr 5q11.2-q13), rs4251417 (SLC6A4, chr 17q11.2) and rs4680 (COMT, chr 22q11.21) were genotyped by High Resolution Melting (HRM)-PCR. All the experiments were performed by the Rotor Gene Q instrument (Qiagen, CA, USA), using the Type-it HRM PCR Kit (Qiagen, CA, USA). The following primers were used for PCR amplifications:
F-5'-GAACGCTGAGTTGATGTAAT-3' and R-5'-CCACCTTCCAAGAATCCT-3' (rs7997012), F-5'-ACCCAATCACTAAATCCT-3' and R-5'-GGAAACTAGACCAGTAAAG-3' (rs2224721), F-5'-GCGAGAACGGAGGTAGCTTT-3' and R-5'-GGTCAGTCTCCCAATTATTGCT-3' (rs6295), F-5'-CTGAGGACTCCTGAGAAC-3' and R-5'-CAGAGAGGGTAGAAAATGTG-3' (rs4251417), F-5'-CAGCGGATGGTGGATTTC-3' and R-5'-TTCCAGGTCTGACAACGG-3' (rs4680), all designed by Beacon Designer v. 7.9 (PREMIER Biosoft, CA, USA). After an initial step of enzyme activation at 95℃ for 5 min, PCRs were carried out by 40 cycles as follows: denaturation at 95℃ for 10 sec and annealing at 60℃ for 30 sec (56℃ for rs2224721). The HRM analysis was performed with a temperature resolution of 0.1℃ and a temperature range between 70℃ and 85℃. Data collection and genotype calls were obtained by the Rotor-Gene 6000 series software v. 1.7 (Qiagen, CA, USA) using as reference genotypes DNA samples sequenced by the ABI Prism® 310 Genetic Analyzer (Applied Biosystems, CA, USA).
Statistical analysis
Chi-squared test, Fisher's exact test and student's t test were used as appropriate for comparing baseline characteristics among treatment groups (Table 2). The effect of genotypes and alleles on response and remission rates was estimated through Pearson's chi-squared tests. In order to account for the confounding effect of recruitment site and baseline HDRS impact on response and remission in the IPC group (Table 2), one-way ANOVA was used within a linear regression model to study the effect of genotypes and alleles on clinical outcomes adjusting for the reported variables. Given that a gender-dimorphic effect has been previously reported for three of the studied polymorphisms (see Introduction), the possible interaction allele x gender was also tested. Only results obtained in the completers group (Table 2) were reported since the presence of only two time points of evaluation did not allow a reliable application of the last observation carried forward (LOCF) method. Analysis were carried out both in the two treatment arms separately and in the whole sample, since similar mechanisms are supposed to mediate the antidepressant effect of both treatments.44,45 The level of significance was conservatively set to 0.05. R software was used for the analysis (cran.r-project.org/). Genotype frequencies were evaluated for Hardy-Weinberg equilibrium using Haploview 4.2. Our sample setting alpha value to 0.05 two tailed provides a power of 0.80 to observe for the whole sample a difference between two variants with effect size d=0.26, which corresponds to a difference of (at least) 1.5 points in the final HDRS and to an explained variance of 2.2%.
RESULTS
The studied polymorphisms did not show any deviation from Hardy-Weinberg equilibrium (COMT rs4680: p=0.14; HTR1A rs6295: p=0.25; HTR2A rs2224721: p=1; HTR2A rs7997012: p=0.62; SLC6A4 rs4251417: p=0.98).
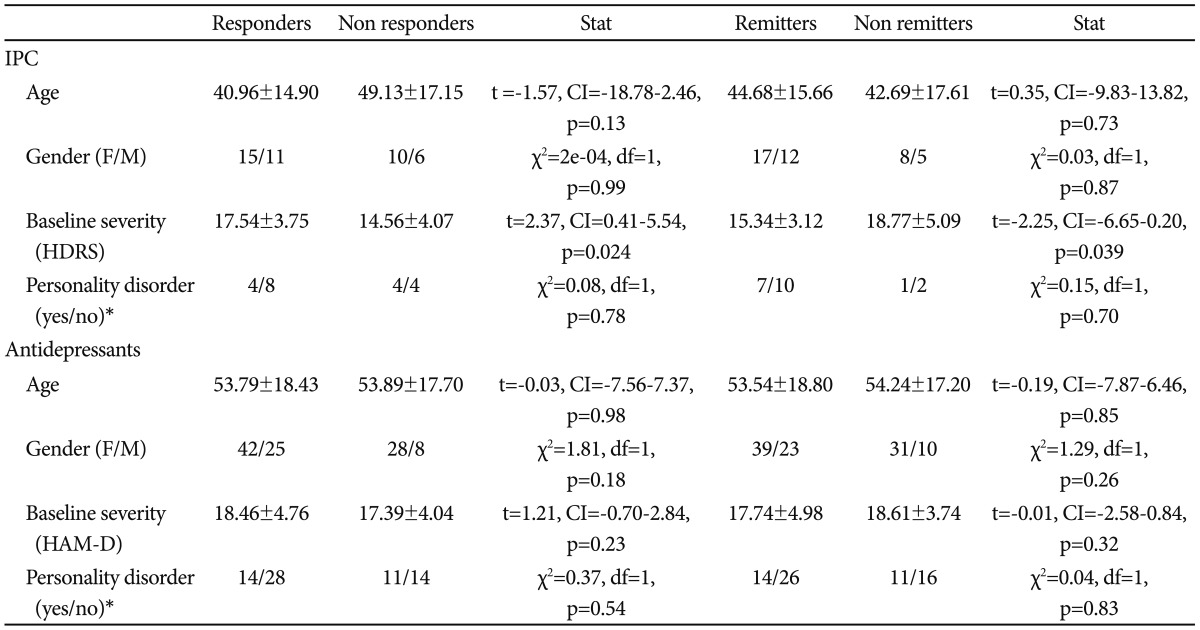
Clinical-demographic characteristics of the sample were reported in Table 1 for the whole sample and in Table 2 for each treatment group. For 15 patients (9.38%) HDRS was not available at week 8 (Table 2), but this group did not show any difference in age (47.93±18.17; t=-0.60, CI=-13.85 - 7.75, p=0.56), gender (F/M:10/5; chi2=1.04, df=1, p=0.31) and baseline severity (21.47±9.52; t=1.56, CI=-1.44 - 9.18, p=0.14) when compared to the 8 week-completers. Moreover, no different risk of drop-out was found between the ICP and antidepressant group, though a trend of better retention was detected in the IPC group (Table 2). No difference was also observed in response and remission rates and percent of improvement at week 8 between the two treatment groups (Table 2), also adjusting for age, baseline severity and center (response: F=0.19, df=1, p=0.66; remission: F=1.15, df=1, p=0.29; % improvement: F=0.59, df=1, p=0.44). In the IPC group the remission rate was slightly higher than the response rate, and this was explained by a lower baseline severity in this treatment arm than the pharmacotherapy arm. Nevertheless, the difference was not so pronounced to be clinically relevant and all regression models were adjusted for baseline severity. Age, gender and presence of a personality disorder did not show any effect on outcomes in both treatment groups (Table 3). On the other hand, response and remission rates were influenced by baseline severity in the IPC group (Table 3).
Distribution of clinical variables according to response and remission status, for each treatment group
Serotonin-related polymorphisms
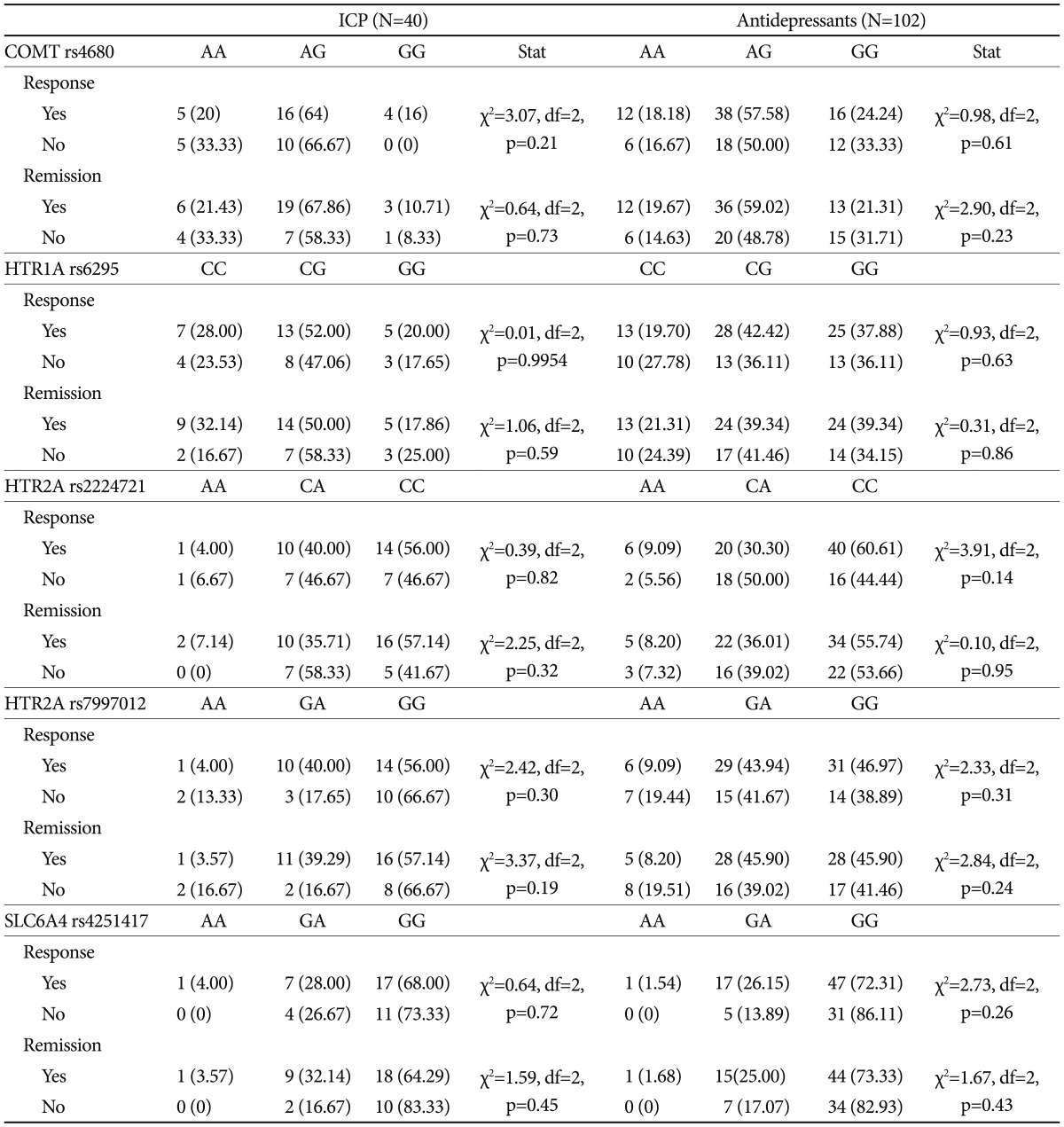
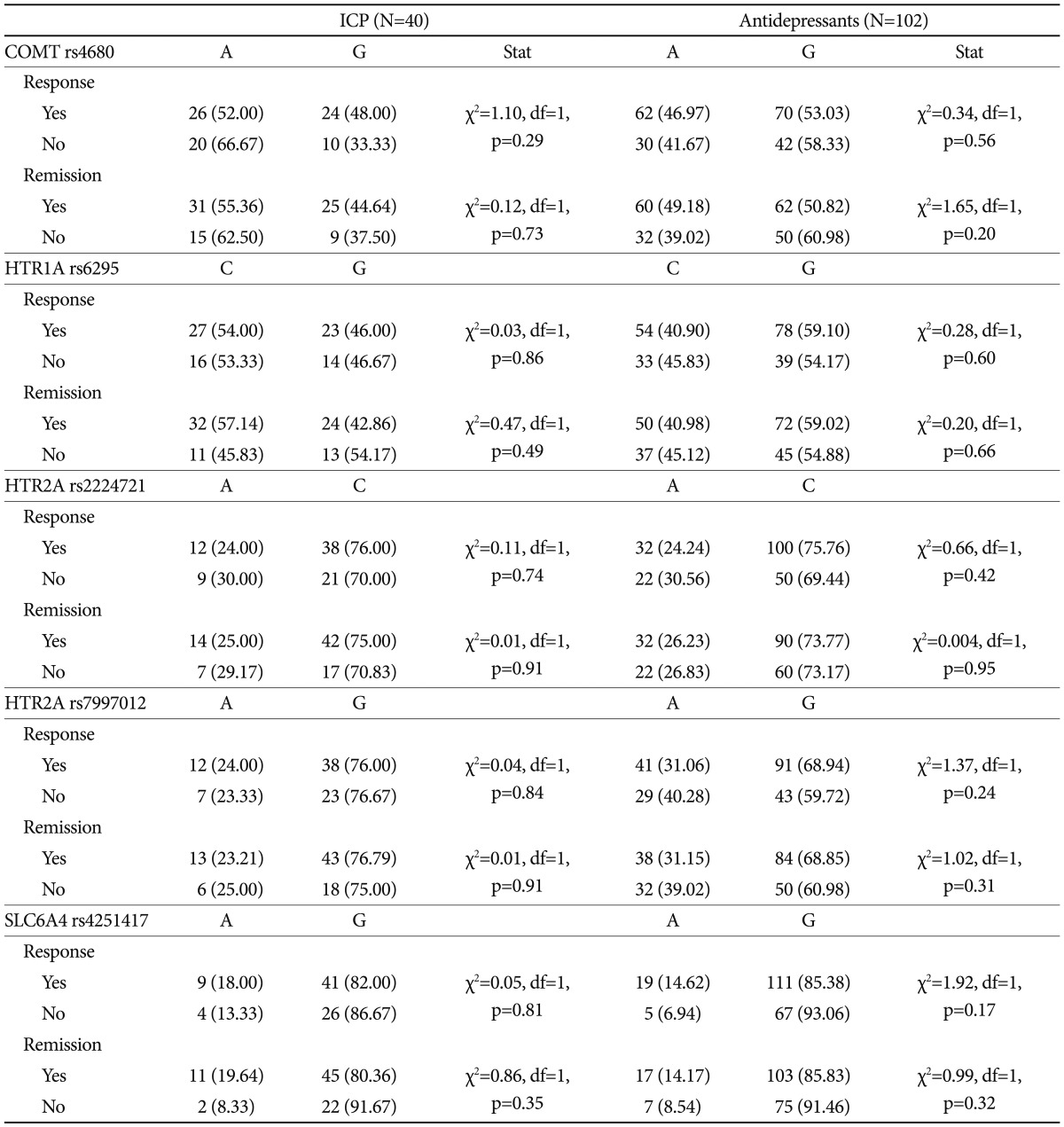
None of the investigated polymorphisms showed to affect response and remission rates neither in the IPC nor in the antidepressant treated group (Table 3 and 4). One-way ANOVA confirmed no effect of genetic variants on clinical outcomes after adjusting for center and baseline severity in the IPC group (data not shown). On the other hand, in the whole sample a trend of association between rs7997012 (HTR2A) and remission was observed (χ2=5.78, df=2, p=0.056), confirmed by one-way ANOVA adjusted for baseline severity and centre (F=2.93, df=2, p=0.057). Subjects carrying the AA genotype showed lower 8-week improvement of the HDRS score (38.74±33.89) compared to those carrying the GA genotype (58.13±27.91) and the GG genotype (55.67±27.33).
No major gender-stratification effect was detected. However, HTR2A rs2224721 showed a trend of interaction with gender: in the IPC group males carrying the A allele showed lower HDRS improvement than those carrying the C allele, while this difference was not observed in females (F=6.38, df=1, p=0.01). Indeed, the HDRS improvement (%) at week 8 was 42.64±17.02 in males carrying the A allele, while it was 52.27±11.81 in carriers of the C allele. In females instead, the improvement was similar for both alleles (C: 51.95±21.15; A: 55.85±27.73). A trend in the same direction was found in the antidepressant treated group (F=3.96, df=1, p=0.048) as well as in the whole sample (F=2.79, df=1, p=0.096).
DISCUSSION
The present study investigated the efficacy of a brief structured psychological intervention, IPC, versus the more widely used antidepressant drug treatment, together with the effect of five serotonin-related polymorphisms on clinical outcomes in both treatment groups as well as in the whole sample. No differences in response, remission rates and percent of improvement at week 8 were found between the two treatment arms (Table 2), also adjusting for age, baseline severity and center. Our findings support the efficacy of IPC in the treatment of mild-moderate MDD, suggesting it is a useful alternative to antidepressants. The choice of IPC may be particularly useful in patients with higher risk of drug-related adverse events, like the elderly (because of polypharmacy and chronic diseases), pregnant women and in post-partum MDD, as confirmed by the marginally higher number of discontinuations in the antidepressant group. Only in the IPC arm, responders showed higher HDRS scores at baseline, while the opposite picture was seen for remitters (Table 3). Also previous studies reported contradictory results about the association between baseline severity score and antidepressant treatment outcome, which do not allow a clear interpretation.52 Anyway, baseline severity scores per se are probably not a predictor of clinical outcome, but possibly only in particular groups of patients (e.g., presence of dysfunctional personality traits53) or depending from the type of treatment.54
None of the investigated serotonin-related variants was found associated with clinical outcomes, either in the antidepressant or in the IPC group (Table 4 and 5) also adjusting results for confounding variables (site of recruitment and baseline severity-IPC group). The polymorphisms of interest were investigated also in the whole sample, since similar mechanisms of action are supposed to lay behind the clinical efficacy of both antidepressant drugs and psychotherapy.44,45 In the whole sample a trend of lower remission was found in subjects carrying the AA genotype of rs7997012, as well as lower percent HDRS improvement at week 8 was observed in this group (38.74±33.89 vs. 58.13±27.91 of the GA and 55.67±27.33 of the GG genotypes).
The studied polymorphisms were carefully selected in accordance with the known biological function and previous pharmacogenetic findings. The role of COMT rs4680 and HTR1A rs6295 has been repeatedly studied, but with inconsistent results, particularly in regard to the identification of the risk allele.6 On the other hand, HTR2A rs2224721 and SLC6A4 rs4251417 are new candidates, since the former was one of the best pharmacogenetic findings of the GENDEP study14 but confirmations are lacking, while the latter has not been studied yet as predictor of antidepressant efficacy despite of its key position. Despite our overall negative findings, a trend of association with HTR2A variants was detected, supporting the quite replicated evidence which suggest a role of the gene in antidepressant effect.10-12 Indeed, HTR2A rs7997012 A allele was a confirmed predictor of citalopram response in the STAR*D study,10,11 while in the GENDEP study an association in the opposite direction was reported,12 in line with our results; finally, some smaller studies reported negative findings.13-16 The other interesting result involving HTR2A is a detrimental effect of rs2224721 A allele only in males, who showed a lower HDRS improvement compared to males carrying the C allele. The finding supports the hypothesis of a gender-stratification effect affecting the association between genetic variants and antidepressant outcome, as several lines of evidence previously suggested.55
Nevertheless, the overall negative findings provided by the present study further suggest that the role of these polymorphisms in antidepressant efficacy is probably modest, i.e., the explained variance in response is probably low considering only one polymorphism at a time. For example, rs2224721 explained only about the 1.1% of the variance in response to escitalopram in the GENDEP study, despite it was one of the SNPs with higher evidence of association14 and in our study we could not detect explained variances lower than 2.2%. Indeed, the small sample size is the major limitation of the present study, and also the multicenter nature may introduce biases, but we used all standard methods to avoid center effects, and consequently no center stratification effect was observed. The lack of a combined treatment arm may be seen as a limitation, but the available evidence suggest no clear benefit of combined treatment over monotherapy in mild-moderate MDD,4 thus no further useful information could be derived from this analysis. As for strengths, despite the relative small sample size, the present study is the first to investigate the role of serotonin-related genetic variants in both psychotherapy and antidepressant treated MDD patients. Serotoninergic genes indeed are a priori optimal candidates for both types of treatment, since the emerging evidence of similar underlying neurobiological basis.44,45,56 Some differences in baseline clinical characteristics were observed between the antidepressant and IPC treated groups (Table 2), this also explains the apparently opposite effects of baseline severity on outcome for IPC, but all regression models comparing the two groups were adjusted for the effect of these confounding variables.
Our results suggest no major role of rs7997012 and rs2224 721 (HTR2A), rs6295 (HTR1A), rs4251417 (SLC6A4) and rs4680 (COMT) in both IPC and antidepressant efficacy. Considering both treatment arms, a trend of worse outcome was detected in carriers of the rs7997012 AA genotype (HTR2A gene), while in all treatment groups as well as the combined sample males carrying the A allele of rs2224721 (HTR2A gene) showed a trend of worse outcome, that was not observed in females. The present study also concluded that IPC, a brief structured psychological intervention, shows similar efficacy to antidepressant drugs in mild-moderate MDD, confirming its clinical usefulness when pharmacological treatments are contraindicated, refused or not tolerated.
Acknowledgments
The study was sponsored by MIUR (2008XWR4SB).