A Study on the Factors Affecting Anger in Patients With Post-traumatic Stress Disorder
Article information
Abstract
Objective
To identify the factors affecting anger in post-traumatic stress disorder (PTSD) patients who underwent Clinician-Administered PTSD Scale (CAPS) and Minnesota Multiphasic Personality Inventory-2 (MMPI-2).
Methods
We retrospectively reviewed patients who underwent CAPS and MMPI-2 at Veteran Health Service Medical Center, Seoul, Korea. Based on the CAPS score, the patients were divided into the PTSD group (n=46) and the trauma exposed without PTSD group (n=29). After checking the correlation between anger, CAPS, and MMPI-2 scales, logistic regression analysis was performed to identify the risk factors for clinically relevant symptoms.
Results
The PTSD group showed significant differences in schizophrenia-related symptoms, ideas of persecution, aggressiveness, psychoticism, and anger scales compared to the trauma-exposed without PTSD group. There was a significant correlation between anger, CAPS, and MMPI-2 except masculinity/femininity, disconstraint, and MacAndrew Alcoholism-Revised. In particular, anger has been shown to have a substantial connection with paranoia, schizophrenia-related symptoms, ideas of persecution, aberrant experiences, and psychoticism. Multiple regression analysis identified that the only significant risk factor for anger was the negative emotionality/neuroticism scale (odds ratio=1.152, p<0.001).
Conclusion
The PTSD group had increased anger compared to the trauma-exposed without PTSD group, and that negative emotions may be a risk factor for PTSD.
INTRODUCTION
According to the the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) diagnostic criteria, post-traumatic stress disorder (PTSD) is characterized by the development of characteristic symptoms following exposure to one or more traumatic events. After experiencing a traumatic event, it is defined as a disorder in which invasive symptoms, stimulus avoidance, negative changes in cognition and emotion, and changes in arousal and responsiveness associated with the traumatic event are experienced. These disorders persist for more than 1 month [1].
Anger is a frequently comorbid emotion in PTSD. The most clinically urgent aspects of PTSD are “self-destructive thoughts and behaviors,” including anger, aggression, and self-harm [2]. Individuals with a history of trauma have been shown to exhibit more severe anger, aggression, and self-harm [3,4]. Several meta-analyses suggest that the way anger is expressed, and which efforts are used to control anger may be important for PTSD patients [5]. This may be prominent in combat-related PTSD [6]. A meta-analysis revealed a close relationship between PTSD and anger in soldiers exposed to trauma [7]. Among those with PTSD, combat veterans are the most frequent exhibitors of aggressive behavior, with up to 95% of all combat veterans exhibiting symptoms of aggressive behavior [4]. In particular, Vietnamese veterans, their spouses, and clinicians continue to prioritize aggression in relation to a number of potential psychiatric problems, including anxiety, depression, and alcohol problems [8,9].
Evidence suggests that negative emotions associated with aggression are at the root of PTSD [10]. These negative emotions appear to play an important role in predicting and mediating PTSD symptoms beyond the influence of other variables [11]. In individuals exposed to trauma, negative perceptions of the self and the world were found to have the strongest correlation with anger [12]. Another study found that groups of veterans with PTSD who tended to express negative emotions toward others were more likely to react aggressively to perceived provocations [9]. Negative emotions have been found to be associated with other emotional responses common to combat-related trauma, such as guilt and shame [13]. According to a study on the relationship between negative perception and anger in combat-related PTSD soldiers [5], negative self-perception partially mediates the severity of PTSD symptoms and modulates the expression of anger. On the other hand, negative perception of the world was found to partially mediate the association between the severity of PTSD and outward expression of anger. This suggests that negative self-assessment is associated with the suppression of emotions and regulation of anger, and that high levels of distrust and anxiety about the world are associated with heightened expression of anger, especially among combat veterans [5].
In this study, the results of the Clinician-Administered PTSD Scale (CAPS) and the Minnesota Multiphasic Personality Inventory 2 (MMPI-2) tests performed in trauma exposed individuals were reviewed retrospectively to identify the MMPI-2 factors found in the PTSD group. Among them, the factors related to anger were investigated. Our hypothesis was that the anger scale is increased in PTSD patients compared to trauma exposed non-PTSD patient controls, and that this scale is associated with negative perceptions in PTSD patients. The purpose of this study is to identify the characteristics of the PTSD patient group with anger, and identify the related factors of the anger and apply them to treatment.
METHODS
Participants
This study was conducted on patients who underwent CAPS between May 2013 and April 2020, when MMPI-2 data were computed at the Veterans Health Service Medical Center (VHSMC). Among them, 67 patients without MMPI-2 values, four patients diagnosed with dementia, and one patient lacking validity in MMPI-2 were excluded. Among the diseases defined as DSM-IV or DSM-5, those with schizophrenia, delusional disorder, delirium, dementia, or a mental disorder due to a medical condition and a history of neurological abnormalities such as head trauma and convulsive disease were also excluded. Therefore, out of a total of 147 computerized individuals, 46 participants in the PTSD group and 29 participants in the trauma group without PTSD were analyzed for a total of 75 individuals (Figure 1).

Schematic overview of our patient population. PTSD, post-traumatic stress disorder; CAPS, Clinician-Administered PTSD Scale; MMPI-2, Minnesota Multiphasic Personality Inventory-2.
This study was conducted retrospectively after reviewing the medical records with approval from the Institutional Review Board of the Veterans Health Service Medical Center (VHSMC IRB No.2020-04-009). The VHSMC was established for patients with traumatic events, such as military-related and combat participation in the Vietnam War to provide treatment.
Clinical assessment
Clinician-Administered PTSD Scale
The CAPS is an in-person clinical assessment designed to evaluate eight relevant characteristics including symptoms associated with PTSD, the degree to which criterion A is met, and current functional difficulties, among others. It was developed by Blake [14], and Weathers et al. [15] applied it to a group participating in the Vietnam War, obtaining good reliability and validity. In a Korean study, the concordance between Cronbach α and the interviewee was 0.95 and 0.89, respectively, showing a high concordance rate of 82.1% with the clinical diagnosis [16]. If we look at the contents of the CAPS in detail, the items of criterion A describe the traumatic event in detail, and the items of criteria B, C, and D consist of questions about symptoms. The total severity score of CAPS was interpreted according to Weathers et al. [15]. A score of 20 or less was evaluated as having few symptoms, and a score exceeding 20 was evaluated as the presence of symptoms corresponding to PTSD [15].
Minnesota Multiphasic Personality Inventory-2
The MMPI is the most widely used personality test worldwide. In MMPI-2, questions and terms related to religion, sex, defecation, bladder, and some others were excluded from the existing MMPI. In the MMPI, 16 of the 566 items were duplicated, but MMPI-2 consisted of 567 items without duplicates. The validity of the scale has been increased compared to the MMPI, and several subscales such as the clinical subscale, the reconstructed clinical scale, the personality pathology 5-factor scale, the content scale, the content subscale, and the supplementary scale have been added in addition to the existing clinical scale. The raw score on the psychological scale is often not interpretable. The same raw score on the two scales does not imply that the two scores have the same percentile. Therefore, a standardization process for converting raw scores into standard scores based on an appropriate reference group is required, and one of the well-known methods is the T-score conversion method. This method ensured that all scales had the same mean score 50 and standard deviation 10. This increases comparability between the measures [17].
MMPI-2 anger scale
People who scored high on the MMPI-2 anger scale (ANG) scale among on the MMPI-2 were described as having difficulty controlling anger and having anecdotes of frequent anger outbursts. This is because these behaviors are included in the items on this scale. Among the MMPI-2 items, the ANG scale consists of 16 items related to anger, the Explosive Behavior (ANG1) subscale, and the Irritability (ANG2) subscale. If the T-score is 65 or higher, the following interpretation is suggested: - Often feel angry and hostile aggressive, critical, and controversial. May lose control or be physically violent. Impulsive, low tolerance for frustration, and sensitive to criticism.
MMPI-2 negative emotionality/neuroticism scale
The MMPI-2 negative emotionality/neuroticism (NEGE) scale consists of 33 items that evaluate a wide range of negative emotional experiences. High scores were associated with focusing on the negative aspects of incoming information, worrying, becoming easily self-critical, feeling guilty, and creating worst-case scenarios. If the T-score is 65 or higher, the following interpretation is possible: - Tendency to experience negative affect. Focus on negative information that could be problematic. Few or no friends. Self-critical, prone to feeling guilty. Tends to be overly concerned and anxious about the present and the future. Reporting sad or depressed feelings. Not optimistic or achievement oriented.
MMPI-2 MacAndrew Alcoholism-Revised
The MMPI-2 MacAndrew Alcoholism (MAC) scale was developed by comparing the MMPI items of male patients undergoing treatment for alcoholism and psychiatric disorders and male patients whose main problem was not alcoholism. It consists of 49 questions, and if the raw score is 29 or higher (T score 68), the individual is highly likely to have a substance abuse problem. If the raw score is 23 or less, it is interpreted that the possibility of having a substance abuse problem is low. Studies have shown that people who score high on the MAC-R display personality traits of extraversion and risk-seeking behaviors [18].
Combat Exposure Scale-Korea
Regarding combat-related trauma, Combat Exposure Scale (CES) is the most widely used self-report scale developed by Keane et al. [19]. The CES is a self-reported questionnaire that evaluates the degree of exposure to combat and consists of seven items. Each item measured exposure to a variety of combat-related situations. Accordingly, Kim et al. [20] translated the combat exposure scale into Korean, which is widely used in combat-related PTSD research and has been recognized for its high validity and reliability. After verifying its validity and reliability, we developed a Korean version of the CES that can be used to evaluate the intensity of combat-related trauma in clinical practice [20].
Statistical analysis
Fisher’s exact tests for categorical variables and independent t-tests for continuous variables were used to compare educational years, age at CAPS, MMPI-2 of Subscales (Clinical Scale, Restructured Clinical scales, Personality Psychopathology-Five scales [PSY-5], Content scales, ANG, Supplementary Scale, MAC-R), and CES-K between individuals with and without PTSD. To confirm the correlation between anger, CAPS, and MMPI-2 scales, Pearson’s correlation was calculated in the PTSD group. Binary multiple logistic regression analysis with stepwise variable selection was performed to evaluate factors related to anger. Variables that showed a significant correlation with anger were included in the logistic regression analysis. With the aim of eliminating multicollinearity, paranoia (T_Pa), schizophrenia (T_Sc), ideas of persecution (T_RC6), aberrant experiences (T_RC8), and schizophrenia (T_Sc) among psychoticism (T_PSYC) were included in the model. p was set at 0.05. In the PTSD group comparison and correlation analysis, the significance level was set at p<0.05, with false discovery rate corrected for multiple comparisons [21]. All statistical analyses were performed using SPSS version 21.0.0.0 (IBM Corp., Armonk, NY, USA) and R version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org).
RESULTS
Table 1 presents the characteristics of each patient group. The subjects consisted of 70 males and 5 females. Of the 75 patients, 51 had military-related trauma and 24 had other trauma types. Among military-related traumas, 29 were combat-related. In total, 54 people were subjected to the CES-K, of which 22 were combat-related trauma types. Eleven personnel rated CES-K as 0, indicating absence of combat-related trauma. The PTSD group included four females, each with two sexual assaults, one family death, and one traffic accident-related trauma. One female in the trauma exposed without PTSD group experienced trauma related to a traffic accident. The average age of the trauma exposed without PTSD group was 66.45±12.08, and the PTSD group was 57.43±18.77, with an average age of 60.92.
Independent t-test
The PTSD group and the trauma exposed without PTSD group were compared through an independent t-test. Educational years, age at CAPS, Clinical Scale of MMPI-2, Restructured Clinical scales, PSY-5, Content scale, ANG, Supplementary Scale, MAC-R, and CES-K were checked for differences between the two groups (Table 1).
There were no statistically significant differences in age, years of education, and CES-K at the time of CAPS implementation. When comparing the clinical scales of MMPI-2, T_Pa and T_Sc scales were significantly higher in the PTSD group than in the trauma exposed without PTSD group. Among the Restructured Clinical scales in the PTSD group, RC6 and RC8 scales showed statistically significant increases when compared to the trauma exposed without PTSD group. In addition, among the PSY-5 scales in the PTSD group, the aggressiveness (T_AGGR), T_PSYC, and T_NEGE scales showed a statistically significant difference compared with the control group. The ANG content scale showed a significant increase in the PTSD group.
Correlation analysis
Table 2 presents the correlation analysis between the CAPS, ANG, and MMPI-2 scales based on patients with PTSD. It showed correlation with anger in all other scales except masculinity/femininity (T_Mf), disconstraint (T_DISC), and T_MAC-R in the Content scale, Reconstructed Clinical scale, and the PSY-5 Scale. In particular, there were significant correlations (all p<0.01) between T_Pa, T_Sc, T_RC6, T_RC8, and T_PSYC and ANG. Each of these scores had significant differences between the groups in independent t-testing. Figure 2 shows scatter plots and R-values of the correlation analysis for CAPS, anger and significant MMPI-2 clinical scales of PTSD patients in logistic regression analysis of PTSD patients.
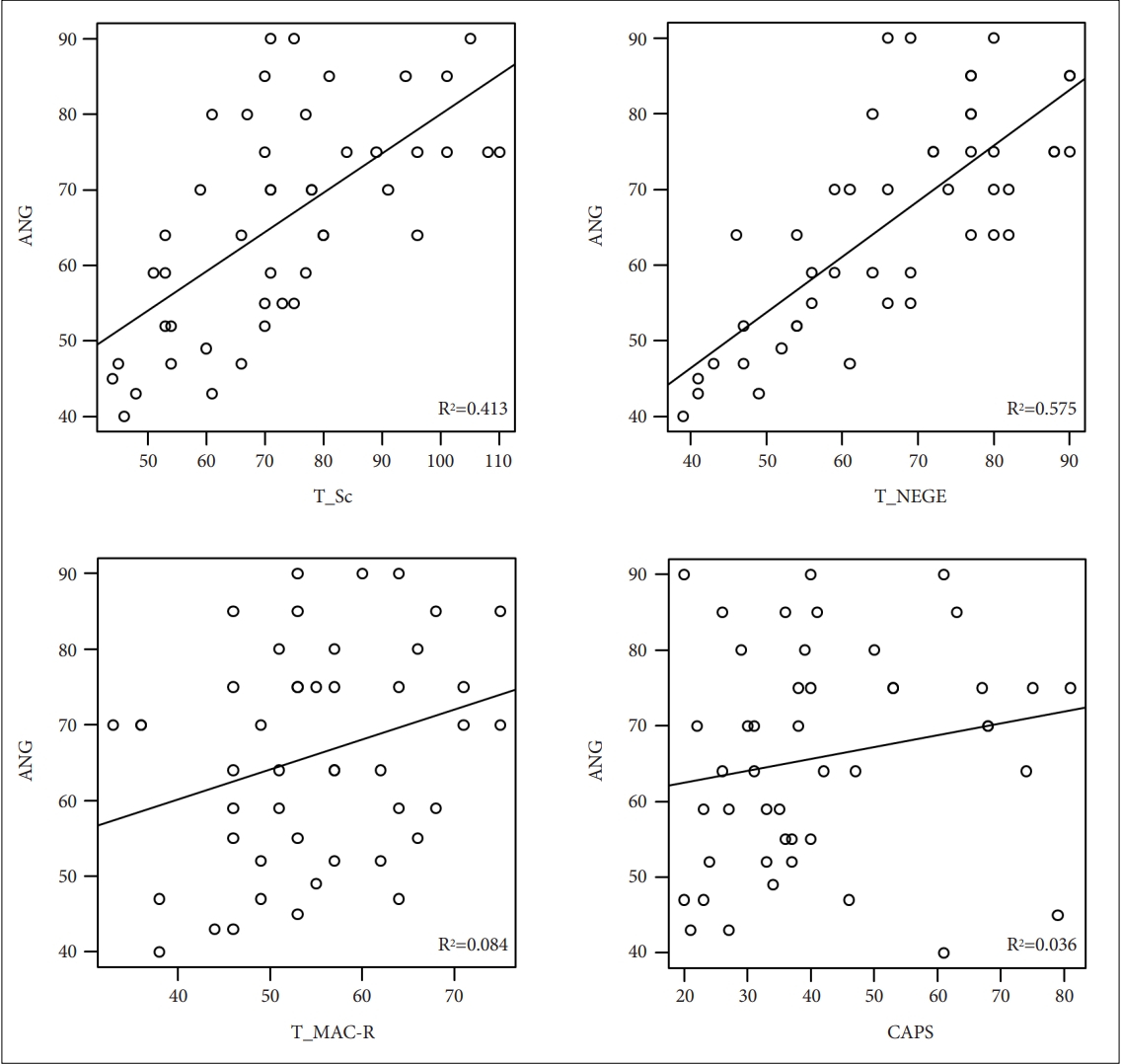
Scatter plots and R-values of the correlation analysis for CAPS, anger and MMPI-2 clinical scales of PTSD patients. CAPS, Clinician-Administered PTSD Scale; MMPI-2, Minnesota Multiphasic Personality Inventory-2; PTSD, post-traumatic stress disorder; ANG, MMPI-2 anger scale; T_Sc, schizophrenia; T_MAC-R, MacAndrew Alcoholism-Revised; T_NEGE, MMPI-2 negative emotionality/neuroticism scale.
Logistic regression analysis
Logistic regression analysis was performed to analyze the effect of MMPI-2 factors on anger affected by the CAPS score of patients with PTSD. Among the variables, T_Pa, T_Sc, T_RC6, T_RC8, and T_PSYC, which showed significant results in the independent t-test, selected T_Sc for the multicollinearity problem. Multiple regression analysis was performed to confirm the risk factors for anger along with other variables without multicollinearity. Among them, T_NEGE was selected as a variable because its p-value was 0.045 in the independent t-test and it had a significant correlation with anger in the correlation analysis. Table 3 shows T_Sc (odds ratio [OR]=1.103, p=0.001) and T_NEGE (OR=1.157, p<0.001) in univariate logistic regression, indicating significant results. In multiple logistic regression, T_NEGE (OR=1.152, p<0.001) was the only statistically significant result.
DISCUSSION
In this study, we attempted to confirm the characteristics and differences of each group regarding anger using MMPI-2. The PTSD group showed significant differences in ANG, T_Sc, T_RC6, T_AGGR, and T_PSYC when compared to trauma exposed patients without PTSD. ANG, T_Pa, T_Sc, T_RC6, T_RC8, and T_PSYC showed strong correlations with anger, while T_Sc and T_NEGE were risk factors for anger in univariate logistic regression. In multiple logistic regression, T_NEGE was the only significant predictor.
This study was conducted at a veteran’s hospital in Korea, which is a hospital that mainly provides health care services to people of national merit and their families. The average age of the subjects was 60.92 years, most of them were elderly patients, and more than 40 years had elapsed since their exposure to trauma. When comparing the two groups, there was a significant difference in the mean age between the trauma exposed without PTSD group and the PTSD group at the age of CAPS and was adjusted as a variable during multiple regression analysis. In the population of this study, the number of military-related trauma patients was 51 out of 75, which is related to military-related PTSD. The total lifetime incidence of PTSD is 9%–15%, and the lifetime prevalence is approximately 8%. A higher prevalence may be seen in military personnel with high occupational risk of trauma, such as veterans, police, and firefighters, or survivors of rape, combat, or genocide. In particular, the prevalence increases to approximately 58% in high-risk populations such as war veterans, and there is a report that about 30% of Vietnamese war veterans experience PTSD [22-25].
When the PTSD group and the trauma without PTSD group were compared using the t-test, there was a significant difference in anger as measured through the CAPS. This is consistent with the results of other studies showing that anger is a prominent feature in the PTSD patient group [6]. According to Dunmore et al. [26]’s cognitive model, this may be related to the assumption that traumatized individuals are more susceptible to anger responses when trauma-related assessments violate individual rules and injustices. In PTSD, frequent symptoms of aggression, impulsivity, depression, and suicidal ideation may occur due to serotonin dysregulation [27]. Specifically, serotonin has numerous roles in the central nervous system, including regulation of sleep, aggression, appetite, cardiovascular and respiratory activity, motor output, anxiety, mood, neuroendocrine secretion, and analgesia [27]. In one study, functional mutations in the tryptophan hydroxylase-2 gene, which affects serotonin synthesis, were said to be related to the personality traits of negative emotions [28]. PTSD is known to be caused by damage to the functional network between the cerebral cortex and limbic system [29]. In previous brain imaging studies, abnormalities have been found in circuits between the amygdala, medial prefrontal cortex, insula, anterior cingulate cortex, and hippocampus, which are mainly related to fear perception and response [29]. Damage to amygdalar control due to overactivation of the amygdala and underactivation of the medial prefrontal cortex as major factors in PTSD pathophysiology have been consistently reported [29]. These findings can provide biological evidence of anger that occurs when PTSD patients are exposed to negative stimuli.
As a cause of PTSD, cognitive-behavioral factors are just as important as the severity of the trauma and changes in the pretraumatic experience [26]. In this study, negative perceptions were different among the PTSD patients, which is similar to the previous studies in which PTSD patients had negative beliefs about their perception of themselves, their world or their future [30,31]. This is also consistent with previous studies, meaning that positive responses are not perceived in patients with PTSD and negative perceptions are maintained [26,32]. It is also consistent with the findings of the paper, which found that negative perceptions of fear, guilt, shame, sadness, and disgust were associated with traumatic memory in a non-military sample [33,34]. Therefore, we have identified cognitive-behavioral factors, and by solving them, we can think about the need to solve the core symptoms of PTSD by improving negative perceptions. Cognitive processing therapy (CPT) may be used to improve these negative perceptions. In another study, 50% of 60 patients with chronic military-related PTSD showed improvement in PTSD symptoms after CPT treatment [35]. Additionally, eye movement desensitization and reprocessing (EMDR) promotes the reconstruction of traumatic memories. It alleviates PTSD symptoms by reducing the intensity of traumatic memories mediated by the hippocampus and associated negative emotions processed by the amygdala [36]. This study confirmed that PTSD can be improved through the improvement of negative emotions that affect anger.
When correlation analysis was performed with anger and other MMPI-2 factors, it was confirmed that T_MAC-R was not significantly correlated with ANG, but was close to a significant value (p=0.054). Among individuals with PTSD, alcohol abuse or dependence is the most common comorbidity in males and the third most common diagnosis in females, after depression and other anxiety disorders. The estimated prevalence of alcohol use disorder in individuals with PTSD is higher than that in the general population [24]. Veterans, especially those with combat experience, are one of the groups at high risk of developing PTSD and increased alcohol use [37].
In the results of this study, T_Pa showed a significant difference between the two groups and a significant correlation with CAPS and ANG. According to Freeman et al. [38], exaggerated or unfounded thoughts that others are trying to harm them can be considered paranoid [39]. Several cross-sectional studies have investigated the association between victimization, PTSD symptoms, and fatal accidents [40,41]. Analysis of the National Epidemiological Survey showed that paranoid thinking and PTSD had a very strong association, with mild paranoia having an odds ratio of 3.5 and strong paranoia with an odds ratio of 27 [42].
Although this study is meaningful in that it evaluated anger-associated factors in PTSD patients with MMPI-2, it has several limitations. First, the sample mainly consisted of elderly patients with PTSD who had undergone long-term psychiatric treatment. Second, out of 75 subjects, 51 were military-related trauma types and 24 were other trauma types. A total of 27 people participated in the Vietnam War, 13 out of 46 PTSD and 14 out of 29 trauma exposed without PTSD. Additionally, only five females were included, and it is difficult to generalize the results to patients with non-military—related PTSD and females. Third, there is a limitation in sample size given the small number of patients considered in our analyses. Therefore, additional studies are needed to validate the measured values using a larger clinical sample including PTSD. Fourth, we have not fully considered potential confounding factors such as duration of illness, current pharmacotherapy, combat exposure levels, the quality of social and family support. The duration of illness in patients who participated in the Vietnam War is estimated to be about 40 years, but trauma events occurred long time ago and there was no accurate record, it was difficult to investigate the exact duration of illness. Several confounding factors that were not evaluated in this study, should be considered in future studies. A small number of studies have shown that the correlation between anger and PTSD becomes stronger over time after the event [6,43,44]. The risk of anger and PTSD was higher in groups experiencing more trauma, such as soldiers who engage in direct combat [45]. Wilks et al. [46] suggested that social support is an important variable that has a significant impact on anger of veterans. Another study found that low levels of social support were significantly associated with negative mood changes in patients with PTSD [47]. Several confounding factors, that were not evaluated in this study, should be considered in future studies. Finally, there is a limitation in not using a separate scale other than MMPI-2 to measure the anger of the target group.
In conclusion, in the anger-presenting PTSD group, negative emotionality was an important feature of PTSD. Through these results, it is necessary to understand and deal with anger in the PTSD group. In addition, it is necessary to improve the emotional regulation ability of the PTSD group, which provides a basis for considering CPT and EMDR as treatment goals for the improvement of negative emotions.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Hayun Choi. Data curation: Sungsuk Je, Seon Namgung. Formal analysis: Sungsuk Je, Hayun Choi. Funding acquisition: Hayun Choi. Investigation: Sungsuk Je. Methodology: Sungsuk Je, Hayun Choi. Project Administration: Sungsuk Je, Hayun Choi. Resources: Hayun Choi, Kiwon Kim, Hyung Seok So, Jin Hee Choi, Seung-Hoon Lee. Software: Sungsuk Je, Hayun Choi. Supervision: Hayun Choi. Validation: Sungsuk Je. Visualization: Sungsuk Je, Hayun Choi. Writing—original draft: Sungsuk Je. Writing—review & editing: Hayun Choi.
Funding Statement
This study was supported by a VHS Medical Center Research Grant from the Republic of Korea (Grant number: VHSMC 20008).
Acknowledgements
We would like to express our deepest gratitude to Researcher Young Lee (Veterans Medical Research Institute), who made valuable contributions to the statistical analyses.



