Elevated Brain-Derived Neurotrophic Factor Levels During Depressive Mixed States
Article information
Abstract
Objective
Neurotrophin-like brain-derived neurotrophic factor (BDNF) and pro-inflammatory cytokines may modulate the pathophysiology of mood disorders. Although several studies show alterations in these biomarkers during the depressive, manic, and euthymic states of mood disorders, evidence is lacking for those in a mixed state. Therefore, this study aimed to investigate the relationship between the depressive mixed state (DMX) and peripheral neurobiological factors.
Methods
We enrolled 136 patients with major depressive episodes. Depressive symptoms were assessed using the Quick Inventory of Depressive Symptomatology Self-Report Japanese version (QIDS-SR-J). The severity of DMX was assessed using the self-administered 12-item questionnaire (DMX-12). Categorical screening as DMX-positive (n=54) was determined by a cutoff score of 13 or more in the specific eight symptoms from the DMX-12; the remaining were DMX-negative (n=82). Serum BDNF, tumor necrosis factor-α, highsensitivity C-reactive protein, and interleukin-6 levels were measured.
Results
When comparing biomarkers between the DMX-positive and DMX-negative groups, higher serum BDNF concentration in the DMX-positive group than in the DMX-negative group was the only significant finding (p=0.009). A positive correlation existed between the total score of the eight specific symptoms of DMX-12 and the BDNF concentration (r=0.190, p=0.027). After adjustment for confounders, logistic regression analysis revealed that BDNF (odds ratio [OR]=1.07, 95% confidence interval [CI]=1.00–1.14, p=0.045), bipolar diagnosis (OR=3.43, 95% CI=1.36–8.66, p=0.009), and total QIDS-SR-J score (OR=1.29, 95% CI=1.15–1.43, p<0.001) were significantly associated with DMX positivity.
Conclusion
BDNF was positively associated with DMX severity, suggesting that higher BDNF concentrations may be involved in the pathophysiology of DMX.
INTRODUCTION
A depressive mixed state (DMX) is characterized by a fullblown depressive episode with some hypomanic features. Previous research has suggested that several symptoms (e.g., overt irritability and/or psychomotor agitation) are cardinal features of DMX [1]. Because DMX is characterized by high energy and impulsivity coexisting with depression, suicide risk is very high in patients with DMX [2]. DMX worsens patients’ functioning and quality of life by increasing agitation, distress, psychotic symptoms, suicidal ideation, and hypersensitivity to antidepressant treatment [3]. Recent studies suggest that DMX is closely related to the pathophysiology of bipolar disorder (BD) during a depressive state [2,4]. Although DMX has been categorically defined [5,6] and dimensionally quantified [7] from a symptomatic perspective, its biological aspects remain underexplored. Therefore, it is important to identify objective markers associated with the biological mechanisms of DMX.
Increasing evidence suggests that the neuroendocrine and immune systems, which interact with the central nervous system, are involved in the pathophysiology of mood disorders, including BD and major depressive disorder (MDD) [8]. Cytokines can alter the mechanisms associated with serotonin and catecholamines in the brain, while these amines bidirectionally modulate cytokine-mediated responses and vice versa [9]. Previous studies have reported that MDD is associated with elevated levels of inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) [10]. Interestingly, mania has also been associated with elevated levels of inflammatory cytokines (C-reactive protein, TNF-α, and IL-6) [11].
Brain-derived neurotrophic factor (BDNF), abundant in the hippocampus, promotes neuronal cell growth, maintains intercellular junctions, regulates neurotransmitters, and facilitates neuroplasticity, such as long-term potentiation and learning [12]. According to the neurotrophic hypothesis, stress and depression are likely associated with deficiencies in neurotrophic factors, leading to neuronal atrophy and cell loss in key limbic areas and the prefrontal cortex [13,14]. Recent studies have found significant reductions in peripheral BDNF concentrations in patients with MDD compared with healthy controls. In contrast, BDNF concentrations recovered to control levels after effective treatment and symptom remission [15,16]. A recent meta-analysis of clinical data suggested that peripheral BDNF concentrations significantly decrease during both manic and depressive phases but not during the euthymic phase in patients with BD. BDNF concentrations increase after treatment for acute manic and depressive episodes [17]. These studies suggest that BDNF plays an important role in the pathophysiology and clinical course of mood disorders. However, the complex and bidirectional relationship between mood symptoms and BDNF remains unresolved. Thus, we investigated how BDNF affects DMX in patients with mood disorders.
The relationship between DMX and biomarkers has not been well understood; only a few studies on this topic exist [18,19]. This study investigated the relationship between DMX and blood biomarkers in terms of neuroinflammatory and neuroprotective factors. We collected specimens from patients with depressive episodes and investigated whether there were differences in BDNF and inflammatory cytokines between the groups with and without DMX.
METHODS
Patients
This study was conducted between June 2014 and December 2019. We recruited 136 patients (46 males and 90 females) with major depressive episodes who consecutively attended the University of the Ryukyus Hospital’s outpatient psychiatric clinic in Nishihara, Okinawa Prefecture, Japan. Two boardcertified psychiatrists confirmed the major depressive episodes according to criteria in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [6]. Of the 136 patients, 96 met the DSM-5’s diagnostic criteria for MDD, and 40 met the diagnostic criteria for BD. We excluded patients with substance-related/addictive disorders, dementia, or inflammatory diseases that could affect blood cytokine concentrations.
Clinical assessment
We assessed the patients’ depressive symptoms using the Quick Inventory of Depressive Symptomatology Self-Report Japanese version (QIDS-SR-J) and the severity of DMX using the 12-item, self-administered questionnaire for DMX (DMX-12) developed in our previous study [7]. Each item of the DMX-12 was scored on a 4-point scale (0=never, 1=only occasionally, 2=often, and 3=almost always).
Categorical screening as DMX-positive was determined by a cutoff score of <13 for the eight DMX-specific symptoms (over-reactivity, inner tension, racing thoughts, impulsivity, irritability, aggression, risk-taking behavior, and dysphoria) [20]. We used these scores to group the participants into DMX-negative (n=82) and DMX-positive (n=54) groups.
Biomarker measurements
Fasting blood samples (5 mL) were collected from the participants’ antecubital veins before the morning dose of the regular medication. The serum samples were then rapidly separated in a centrifuge at 1,590×g for 15 min and kept frozen at -30°C until assayed. Serum BDNF and TNF-α concentrations were measured by quantitative sandwich enzyme-linked immunoassay. High-sensitivity C-reactive protein (hsCRP) levels were measured by nephelometry, and IL-6 levels were measured by covalent enzyme-linked immunoassays (SRL Inc., Tokyo, Japan).
Statistical analyses
We tested the continuous variables for normal distribution using an F-test. We performed parametric tests (t-test and Pearson’s correlation) or nonparametric tests (Mann–Whitney U test and Spearman’s rank correlation) according to the deviation of the distributions. We used the chi-squared test to compare the categorical variables between the two groups. To identify the factors contributing to DMX-positive cases, we performed multiple logistic regression analyses (forward stepwise selection method) using five independent variables (age, sex, total QIDS-SR-J score, bipolar diagnosis, and BDNF). We used IBM SPSS Statistics of Windows, Version 27.0 (IBM Corp., Armonk, NY, USA) for all statistical analyses. We considered a two-tailed p<0.05 a statistically significant difference.
Subgroup analyses
Subgroup analyses were independently conducted for the patients with BD and MDD. Initially, the participants were categorized into BD (n=40) or MDD (n=96) groups. Subsequently, the means of the DMX-positive and DMX-negative groups were compared separately for each category. An independent t-test was employed for normally distributed data, whereas a Mann–Whitney U test was utilized for non-normally distributed data. We used the chi-squared test to compare the categorical variables between the two groups. Finally, a logistic regression analysis was performed using DMX positivity as the dependent variable and age, sex, total QIDS-SR-J scores, serum IL-6 concentration, and serum BDNF concentration as independent variables in the subgroups of patients with BD and MDD.
Research ethics
All patients provided written informed consent for voluntary participation in the study. We anonymized all data and used only coded and grouped data for analysis. We explained the purpose of the study, our measures to protect personal information, and the patients’ right to withdraw from the study. We conducted the study in accordance with the principles of the Declaration of Helsinki. The Ethics Committee of the University of the Ryukyus for Medical and Health Research Involving Human Subjects approved the study protocol (approval number: 658 originally and 1,682 after amendment in response to changes in Japanese clinical research law).
RESULTS
Group comparison of clinical backgrounds and biological data
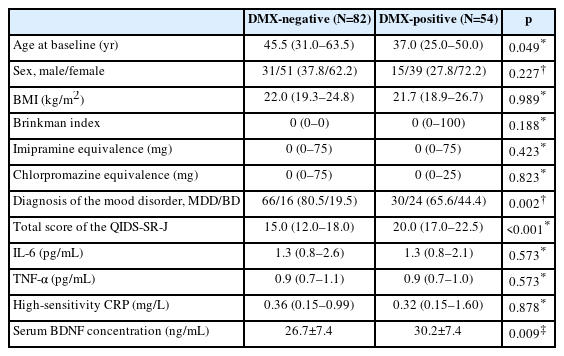
Table 1 shows the clinical background and biological data of the DMX-positive and -negative groups. Among these variables, age at baseline was lower in the DMX-positive group than in the DMX-negative group (37.0 [25.0–50.0] vs. 45.5 [31.0–63.5] years, p=0.049). The rate of bipolar diagnosis was higher in the DMX-positive group than in the DMX-negative group (44.4% vs. 19.5%, p=0.002). The total QIDS-SR-J score was higher in the DMX-positive group than in the DMX-negative group (20.0 [17.0–22.5] vs. 15.0 [12.0–18.0], p<0.001). The DMX-positive group had a higher serum BDNF concentration than the DMX-negative group (30.2±7.4 ng/mL vs. 26.7±7.4 ng/mL, p=0.009). We found no significant differences in sex, body mass index (BMI), Brinkman index, antidepressant dose (imipramine equivalence), antipsychotic dose (chlorpromazine equivalence), or serum concentrations of IL-6, TNF-α, and hsCRP between the two groups (Table 1).
Correlations between biomarkers and severity of depression or DMX
We found no significant correlations between the total QIDS-SR-J scores and serum concentrations of TNF-α (rs=0.012, p= 0.891), IL-6 (rs=0.021, p=0.081), and hsCRP (rs=0.004, p=0.964). In addition, there was no significant correlation between the total QIDS-SR-J scores and serum BDNF concentrations (r=0.038, p=0.662). When we examined the correlations between QIDS-SR-J and BDNF separately in the DMX-positive or -negative groups, the correlation was negative in the DMX-negative group (r=-0.200, p=0.071) but positive in the DMX-positive group (r=0.239, p=0.081), although these correlations were not significant (Supplementary Figure 1 in the onlineonly Data Supplement).
We found a weak but positive correlation between the total DMX-8 scores and serum BDNF concentrations (r=0.190, p=0.027), as shown in Figure 1. In contrast, we found no significant correlations between the total DMX-8 scores and serum concentrations of TNF-α (rs=0.066, p=0.445), IL-6 (rs=0.136, p=0.115), and hsCRP (rs=0.014, p=0.870).

Correlations of serum concentrations of BDNF (A), TNF-α (B), IL-6 (C), and hsCRP (D) with severity of depressive mixed state (DMX) assessed by DMX-8 scores. r: Pearson’s correlation coefficient. rs: Spearman’s correlation coefficient. p<0.05 was considered a significant correlation. BDNF, brain-derived neurotrophic factor; IL-6, interleukin-6; TNF-α, tumor necrosis factor-alpha; hsCRP, high-sensitivity C-reactive protein.
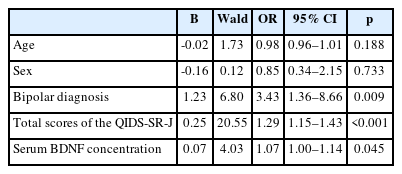
Logistic regression analysis to determine DMX risk factors
Multiple logistic regression analysis with five independent variables (age, sex, bipolar diagnosis, depression severity [total QIDS-SR-J score], and serum BDNF concentration) showed that a bipolar diagnosis (odds ratio [OR]=3.43, 95% confidence interval [CI]=1.36–8.66, p=0.009), total QIDS-SR-J score (OR=1.29, 95% CI=1.15–1.43, p<0.001), and serum BDNF concentration (OR=1.07, 95% CI=1.00–1.14, p=0.045) were significantly associated with the DMX-positive group (Table 2).
Subgroup analysis
Serum IL-6 levels were significantly lower (1.0 [0.7–1.9] pg/mL vs. 2.0 [1.2–3.0] pg/mL, p=0.036), and total QIDS-SR-J scores were significantly higher (19.9±3.6 vs. 14.1±3.7, p<0.001) in the BD with DMX-positive group compared with the BD with DMX-negative group (Supplementary Table 1 in the online-only Data Supplement). BDNF levels (30.4±7.7 ng/mL vs. 26.9±7.9 ng/mL, p=0.043) and total QIDS-SR-J scores (18.7±4.2 vs. 14.7±5.1, p<0.001) in the MDD with DMX-positive group were significantly higher than those in the MDD with DMX-negative group (Supplementary Table 2 in the online-only Data Supplement). Logistic regression analyses revealed that only the total QIDS-SR-J score was a significant factor associated with both BD and MDD subgroups (BD: OR=2.52, 95% CI=1.17–5.43, p=0.018; MDD: OR=1.22, 95% CI=1.08–1.37, p<0.001) (Supplementary Table 3 and 4 in the online-only Data Supplement).
DISCUSSION
In this study, bipolar diagnosis and severity of depression were significant predictors of DMX (Table 2). These findings were consistent with our previous studies [7,21]. Other studies also support the close association between DMX and bipolarity [2,22] or depressive severity, together with higher suicidality and more functional impairment [19,23]. Thus, bipolarity and severe depression are established risk factors for DMX.
We highlighted neuroinflammatory and neuroprotective biomarkers as plausible predictors of DMX and found that serum BDNF was a significant factor independently associated with DMX positivity. However, we found no associations between DMX and neuroinflammatory biomarkers, such as IL-6, TNF-α, or hsCRP.
Several meta-analyses of studies of BDNF in patients with MDD have provided strong evidence that serum BDNF concentrations decrease during the depressive phase but normalize following successful antidepressant treatment [24,25]. One meta-analysis [17] showed that BDNF concentrations were lower in patients with BD than in healthy controls in both manic and depressive states but not in the euthymic state. However, BDNF concentrations normalized after pharmacological treatment in the manic state. The above findings suggest that BDNF concentrations are reduced during a mood episode but reversibly normalized by successful treatment. Therefore, BDNF may serve as a state marker for both MDD and BD independent of the polarity of mood episodes.
The BDNF concentration was higher in the DMX-positive group than in the DMX-negative group (Table 1) and positively related to the severity of DMX (Figure 1), which may at least partly explain why BDNF acts as a possible determinant for the development of DMX (Table 2). Although BDNF concentrations tended to decrease with depression severity in the DMX-negative patients, the opposite occurred in DMX-positive patients (Supplementary Figure 1 in the online-only Data Supplement) despite greater depression severity (Table 1). Therefore, our overall results suggest that DMX severity is closely associated with elevated BDNF concentrations. Previous studies investigating the association between DMX and serum BDNF levels in patients with BD have shown inconsistent results regarding the comparison of BDNF levels in DMX groups and healthy controls. On the other hand, BDNF levels in BD with DMX was consistently reported to be higher than in BD with depressive episode. A previous study comparing BD with the DMX or depressive episode and healthy controls found that BDNF levels in the BD with DMX episode group were significantly lower than those in the healthy control group [19]. A meta-analysis examining BDNF levels across patients with different phases of BD and healthy controls suggested that BDNF levels in the control group were significantly higher than those in the depressive episode group and tended to be lower than those in the DMX group in BD patients, albeit with no statistical significance [26]. These findings were in line with the present study, which observed significantly elevated BDNF levels in the DMX-positive group relative to the DMX-negative group.
Although the mechanism linking BDNF with DMX is unclear, the DMX-positive group had apparently higher BDNF concentrations than the DMX-negative group despite greater depression severity (Table 1). However, there is no clear explanation for this paradoxical response. Given that DMX is a mixture of depression and mania, BDNF should be much lower due to the additional or synergistic effects of both polarities since BDNF concentrations were lowered during both depressive and manic episodes [17]. Our results suggest that the mixed state itself had potent inducing effects on BDNF secretion beyond suppressed BDNF kinetics under depressive pathophysiology or that BDNF increased as a compensatory mechanism to counteract severe depression, which might result in expression as the DMX phenotype. Thus, we can further speculate that DMX is not damage resulting from the depressive-manic mixture but a regeneration process to overcome the depressive pathophysiology. Future studies should focus on the longitudinal course of DMX from a full-blown episode to recovery in relation to intraindividual changes in BDNF concentrations to confirm this hypothesis.
Previous studies suggested that BDNF level tends to be higher in younger age groups [27,28]. In this study, the DMX-positive group was significantly younger than the DMX-negative group. Therefore, age might be associated with BDNF levels in the DMX-positive group, even though statistical significance disappeared after controlling confounding factors with multivariate analysis. Future studies with hierarchical analysis depending on age will be needed to clarify the relationship among DMX, BDNF concentrations, and age.
BDNF exists in two distinct forms: mature BDNF and proBDNF, each exhibiting unique properties. Mature BDNF is known to promote neurogenesis and neuroplasticity and suppress the production of inflammatory cytokines and displays reduced levels in conditions such as MDD. In contrast, proBDNF, associated with cell apoptosis and inflammatory responses, is observed to increase under inflammatory states and in MDD [29,30]. In the current study, our primary focus was the measurement of mature BDNF. However, given the specifications of the assay kit employed, there may have been an approximate 13% cross-reactivity with proBDNF. Consequently, it is possible that our measurements represented a combination of mature BDNF and proBDNF concentrations. A noteworthy direction for future research is to differentiate the measurements of mature BDNF and proBDNF using a more precise assay kit. This enhancement will allow a clearer understanding of how these two forms of BDNF interrelate and contribute individually to conditions such as MDD and inflammatory states.
In our study, pro-inflammatory cytokines were not significantly associated with DMX. A previous study reported that inflammatory cytokines, such as TNF-α and IL-6, were elevated in the DMX of BD [18]. However, a meta-analysis of studies of inflammatory cytokines in patients with BD showed that TNF-α but not IL-6 was elevated during DMX episodes [26]. A more recent systematic review and meta-analysis showed that the levels of hsCRP, IL-6, and TNF-α were not determinants for distinguishing the different mood phases of BD [11]. As mentioned above, the results of previous studies investigating inflammatory cytokines in a mixed-mood-disorder state have been inconsistent. Accordingly, our results suggest that inflammatory cytokines are unlikely to play an important role in DMX pathophysiology.
Our subgroup analysis showed that IL-6 in BD subjects within the DMX-positive group was significantly lower than that in the DMX-negative group. However, multivariate logistic regression analysis showed no significant association between the DMX-positive group and IL-6 levels after controlling confounding factors [31]. Although the reason for this phenomenon was unclear, previous studies reported inconsistent results regarding the relationship between BD with DMX and IL-6 levels. A previous study indicated elevated IL-6 levels in patients with BD in the DMX group, as compared to both healthy controls and the BD with major depressive episode group [18]. Conversely, another study reported no significant differences in IL-6 levels between the BD with DMX and healthy control groups [32]. Given these inconsistent findings, further studies controlling confounding factors associated with the IL-6 level, such as smoking and BMI [32], will be needed to confirm the relationship between DMX and IL-6.
This study has several limitations. First, it was conducted as a single-center design with a relatively small sample size, which could have weakened the power of the statistical analysis. Therefore, a study with a larger sample size is needed. Second, this was a cross-sectional study. Therefore, the causal relationship between DMX and BDNF remains unclear. Third, psychotropic medications such as antidepressants, antipsychotics, and lithium might have affected inflammatory cytokine or BDNF concentrations, as previously reported [17,33]. However, it was difficult to evaluate the impact of the medications on the inflammatory cytokine or BDNF concentrations because most of the patients recruited in this study received a complicated combination of medications, although there was no difference between the DMX-positive and -negative groups at doses equivalent to imipramine and chlorpromazine (Table 1). Finally, the study primarily relied on self-administered scales for assessing depression and DMX. The absence of a physician-rated scale might have introduced a degree of subjective bias to the outcomes. Therefore, future research should consider incorporating both self-reported and physician-rated scales to achieve a more comprehensive evaluation.
In conclusion, our data showed BDNF to be an independent factor associated with DMX. These findings provide evidence that neurotrophic factors might be involved in the pathophysiology of DMX. Further confirmatory studies on the involvement of neurotrophic factors in any mood episode, including DMX, should be conducted with a larger sample size to confirm the present data.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2023.0104.
Comparison of clinical characteristics and biological data in BD patients with and without depressive mixed state (DMX)
Comparison of clinical characteristics and biological data in MDD patients with and without depressive mixed state (DMX)
Logistic regression analysis of screening-positive cases for depressive mixed state in BD patients
Logistic regression analysis of screening-positive cases for depressive mixed state in MDD patients
Correlations between QIDS-SR-J scores and serum BDNF concentrations in DMX-negative (A) and DMX-positive (B) groups. BDNF, brain-derived neurotrophic factor; QIDS-SR-J, Quick Inventory of Depressive Symptomatology Self- Report Japanese version; DMX, depressive mixed state.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Naoaki Otsuka, Hotaka Shinzato, Kazuki Ota, and Kazuhiro Kurihara have no potential conflicts of interest to disclose. Yoshikazu Takaesu has received lecture fees from Takeda Pharmaceutical, Sumitomo Pharma, Otsuka Pharmaceutical, Meiji Seika Pharma, Kyowa Pharmaceutical, Eisai, MSD, and Yoshitomi Pharmaceutical outside the submitted work. Yu Zamami has received lecture fees from Takeda Pharmaceutical, Sumitomo Pharma, Otsuka Pharmaceutical, Meiji Seika Pharma, and VIATRIS outside the submitted work. Tsuyoshi Kondo has received lecture fees from Takeda Pharmaceutical, Sumitomo Pharma, Otsuka Pharmaceutical, Meiji Seika Pharma, Kyowa Pharmaceutical, Eisai, MSD, and Yoshitomi Pharmaceutical outside the submitted work.
Author Contributions
Conceptualization: Hotaka Shinzato, Tsuyoshi Kondo. Data curation: Naoaki Otsuka, Hortaka Shinzato. Formal analysis: Naoaki Otsuka, Yoshikazu Takaesu. Fund acquisition: Tsuyoshi Kondo. Investigation: Naoaki Otsuka, Yu Zamami, Kazuki Ota, Hotaka Shinzato. Methodology: Naoaki Otsuka, Yoshikazu Takaesu, Hotaka Shinzato, Tsuyoshi Kondo. Supervision: Yoshikazu Takaesu, Tsuyoshi Kondo. Validation: all authors. Writing—original draft: Naoaki Otsuka. Writing—review & editing: Naoaki Otsuka, Yoshikazu Takaesu, Tsuyoshi Kondo.
Funding Statement
This work was supported by JSPS KAKENHI [Grant Number JP17K10311, JP21K07504]. The funders had no role in study design, data collection, analysis, writing of the manuscript, and/or decision to publish.