The Factors Affecting Longitudinal Course of Posttraumatic Stress Disorder Symptoms in Sexual Assault Victims
Article information
Abstract
Objective
This study aimed to identify the factors affecting posttraumatic stress disorder (PTSD) symptom remission prospectively through a 1-year follow-up of sexual assault (SA) victims.
Methods
A total 65 female SA victims who visited the crisis intervention center were included. Self-administered questionnaires regarding PTSD symptoms and PTSD related prognostic factors were conducted at both recruitment (T1) and 1 year after recruitment (T2). The multivariate analyses were used to determine the significant predictors of PTSD remission/non-remission state 1 year after SA.
Results
In logistic regression analysis, both anxiety and secondary victimization were identified as significant factors explaining the results on PTSD remission/non-remission state at T2 (Beck’s Anxiety Inventory [BAI], p=0.003; Secondary Victimization Questionnaire, p=0.024). In a linear mixed analysis, both depression and anxiety were found to be significant variables leading to changes in Posttraumatic Diagnostic Scale for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition from T1 to T2 (BAI, p<0.001; Center for Epidemiological Studies Depression Scale, p<0.001).
Conclusion
Depression, anxiety symptoms, and secondary victimization after SA were associated with PTSD symptom non-remission 1 year after SA.
INTRODUCTION
Sexual assault (SA) is an increasingly important social issue in South Korea due to its increasing incidence and the recognition of psychiatric sequelae in survivors [1]. SA is known to be associated with an increased risk of general mental health problems and is closely related to psychiatric disorders, including posttraumatic stress disorder (PTSD), depression, and anxiety disorders [2-4]. In addition, social stigmatization from close relationship as well as secondary victimization during medical and legal procedures after SA, have aggravating effects on the psychological trauma of SA survivors.
Studies of trauma have shown that SA is among the most devastating types of traumatic event. One study comparing symptom severity among different types of trauma showed that the symptoms of PTSD related to SA were more severe than in other types of trauma, such as physical trauma or the unexpected death of a loved one [5]. In addition, psychiatric sequelae of SA are more persistent than those of other types of trauma. A meta-analysis of PTSD trajectories showed that the type of trauma was a significant predictor of PTSD remission [6], and in epidemiological research on PTSD, SA was identified as a strong predictor of a chronic course of PTSD [7]. Moreover, in contrast to nonsexual trauma with alleviation of initial PTSD symptoms over time, the symptoms of sexual trauma do not show alleviation, and may even become aggravated over time. In a study of the longitudinal PTSD symptom trajectory, while the median prevalence trended downward for populations exposed to non-SA-related trauma, the median prevalence in the SA group increased steadily from 11.8% to 23.3% over a period of 12 months, and reached up to 37.1% in some studies [8].
Nevertheless, not all survivors of SA develop PTSD. Some show no symptoms of PTSD, while others show symptoms of PTSD in the early stages after trauma, which resolve later. Studies of the longitudinal course of PTSD have shown that most survivors who develop PTSD after trauma experience decreases in symptom severity in subsequent months. In fact, according to both diagnostic algorithms and clinical guidelines, a typical response to trauma is acute elevation of posttraumatic stress symptoms followed by some degree of natural recovery in the first few months following the trauma [9]. However, some show little change in symptoms over time and even progress to chronic PTSD [8,10].
Therefore, a better understanding of the variables associated with a greater risk of chronic PTSD is important not only for understanding PTSD chronicity, but also for providing timely preventive psychiatric interventions. To identify predictors of chronic PTSD and to screen out those who are at risk of PTSD in the early stage after trauma, there have been many attempts. Previous studies have identified a number of variables that can predict remission of PTSD, and the variables were classified into pretraumatic, intratraumatic, and posttraumatic factors. Pretraumatic factors include female sex, premorbid depressive symptoms, experience of childhood abuse, and underlying psychiatric disorders. Intratraumatic factors, defined as trauma-related factors, include the severity of trauma and subsequent dissociation symptoms [11-14]. With regard to posttraumatic factors, comorbid depressive symptoms, anxiety symptoms, and feelings of shame after trauma have been studied, and all these factors were known to be associated with chronic PTSD. Particularly, the relations between the chronicity of PTSD and social reactions to survivors after trauma, from positive support to negative stigmatization, have been examined [15-18].
However, it is unclear which factors lead to chronic PTSD, particularly in relation to SA. Although there have been many studies on SA-related PTSD, most focused on factors associated with the onset rather than the chronicity of PTSD [19]. Further, there has been some confusion between factors associated with onset and chronicity due to both variability in the observation periods and non-unified definitions of chronicity. In addition, most studies on the longitudinal course of PTSD symptoms were retrospective in nature.
This study was performed to examine which factors contribute to chronic PTSD in SA victims. We prospectively evaluated the PTSD symptom severity in SA victims from the time of the trauma to 1 year later. Based on the literature, we postulated that adverse childhood experiences, dissociation, depressive/anxiety symptoms, severity of initial PTSD symptoms, social support, and secondary victimization contribute to chronic PTSD in SA victims.
METHODS
Participants and procedures
The study population consisted of 141 female SA victims who visited the Seoul Sunflower Center, which provides counseling, medical, investigative, and legal supports for victims of SA and domestic violence. Women at least 18 years of age who visited the center within 3 months after the assault occurred were considered eligible for inclusion in the SA victim group. The exclusion criteria were intellectual disability, autism spectrum disorder, brain damage, convulsive disorder, history of alcohol or drug abuse, and pregnancy.
Victims were then asked to complete self-administered questionnaires regarding PTSD symptoms and related psychopathology (see Measures), when they first visited the center for SA (T1=baseline). They were then asked again to complete self-administered questionnaires on PTSD symptoms 1 year after the enrollment (T2). The duration of the study was set to 1 year based on a previous report showing moderate declines in PTSD prevalence and symptom severity over the first 3–6 months after trauma [9].
This study was approved by the Institutional Review Board (IRB) for Human Subjects of Seoul National University Hospital (IRB No. 1506-073-680). Eligible women who visited the center were informed about the study, and written informed consent was obtained from them.
Measures
Based on previous research, we included the following variables potentially associated with chronicity of PTSD due to SA in this study: adverse childhood experiences, dissociation, depression, anxiety, severity of initial PTSD symptoms, and secondary victimization [7,11,13-15,17,18,20-29]. The secondary victimization was subdivided into formal and informal forms of support.
PTSD
PTSD symptoms were assessed with the Posttraumatic Diagnostic Scale for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (PDS-5), a 24-item self-administered questionnaire that assesses PTSD symptoms using a Likert-type scale with scores ranging from 0, not at all to 4, extremely. This tool assesses the severity of symptoms (score 0–80; cutoff ≥28), with subscores for re-experiencing (0–20), avoidance (0–8), negative alterations in cognition and mood (0–24), and arousal (0–28). In addition, the last two questions assess the duration and frequency of PTSD symptoms.
In this study, we assessed the PTSD symptom severity of SA victims using a partial PDS-5 score items 1–20 excluding the last two questions on duration and frequency of PTSD symptoms. Based on a previous study [30], the cutoff of PDS-5 was set at 28 point. In addition, to validate the significance of change in PTSD symptom severity from T1 to T2, we defined a decrease in PDS-5 score by ≥30% between T1 and T2 as indicating PTSD symptom remission [31-33].
Adverse childhood experiences
We assessed the history of adverse childhood experiences, lifetime exposure to 13 types of traumatic experience using the Revised Adverse Childhood Experiences, which screens for 13 potentially traumatic events in the respondent’s lifetime, clustered into three types: maltreatment; household dysfunction during childhood; and an additional question on peer victimization, peer isolation, and low socioeconomic status. The tool consists of 20 questions, all of which are scored on a 5-point Likert scale [34] with a Cronbach’s α of 0.713 [35]. We used the sum of the score to evaluate the severity of adverse childhood experiences.
Dissociation
Dissociation related to SA was assessed with the Dissociative Experiences Scale-II (DES-II) [36], which consists of 28 questions divided into four subcategories: depersonalization-derealization, amnestic syndrome, absorption and dissociative activity, and pseudopsychotic symptoms. The frequency of the symptoms is evaluated as a percentage, and scored from 0 to 10 by dividing the percentage by 10 (i.e., 10%=1 point…100%=10 points). The Korean version of the DES-II, Korean Dissociative Experiences Scale-II was used in this study, and the Cronbach’s α was 0.948 [37].
Depression
We assessed the severity of depression using the Center for Epidemiological Studies Depression Scale (CES-D) developed by Radloff [38], which includes 20 questions about the level of depressive symptoms to assess symptom frequency and severity rated on a 4-point Likert scale from 0 to 3 with a cutoff score of 16. The Korean version was developed in 2001 by Jeon et al. [39], and the Cronbach’s α was shown to be high (α=0.86). We used the total CES-D score to assess depression severity.
Anxiety
The levels of physical, emotional, and cognitive symptoms related to anxiety were assessed using Beck’s Anxiety Inventory (BAI) consisting of 21 items, 18 of which are rated on a 4-point Likert scale that assesses the level of distress caused by symptoms. The rating scale ranges from 0, not at all to 3, severe, and the cutoff score is 22 [40]. The Korean version was developed in 1997 [41] and the Cronbach’s α was shown to be 0.86. We used the total score of the Korean version of the BAI to assess anxiety severity.
Secondary victimization from administrative and medical procedures
We defined formal and informal forms of secondary victimization as those occurring in the process of medical/legal investigations and the responses from close relations, family and friends, respectively.
Secondary victimization from administrative and medical procedures was assessed using the Secondary Victimization Questionnaire (SVQ), a 25-item screening tool for secondary victimization from administrative, legal, and medical procedures after sexual trauma. It consists of two types of questions to assess the presence of secondary victimization and affective response of participants. All questions are rated on a 5-point Likert scale, and the Cronbach’s α is 0.73–0.76 varying between question subgroups [42].
Secondary victimization from family, friends, and acquaintances
The Secondary Response Questionnaire (SRQ) was developed to assess reactions of family, friends, and acquaintances toward SA victims. This tool consists of 26 items, clustered into five categories: treat differently, distraction, take control, victim blame, and egocentric [43]. The Korean version was introduced in 2014 [44], and Cronbach’s α was shown to be 0.76–0.96. The total score on the SRQ was used to assess the level of secondary victimization in everyday life in the present study.
Statistical analysis
Statistical analyses were performed using IBM SPSS version 22 (IBM Corp., Armonk, NY, USA). In all analyses, p<0.05 was taken to indicate statistical significance.
We used multivariate analyses (linear mixed model and logistic regressions model) to determine the significant predictors of PTSD remission.
First, we used binary logistic regression analysis to determine the variables associated with PTSD symptom remission state. In this model, remission state at T2 (PTSD remission vs. PTSD non-remission) was used as a dependent variable, and all demographics and T1 psychiatric scales were considered as independent variables. The odds ratios (ORs) and 95% confidence intervals were calculated.
Second, we used a linear mixed model to examine the time and group effects on PTSD symptoms. Linear mixed analysis is superior to other statistical methods because incomplete/missing data can be incorporated into the analysis. We divided the SA victim group into three subgroups—no symptoms group (SA victim without PTSD symptoms at T1), remission group (SA victim with PTSD symptoms at T1 but remission at T2), and non-remission group (SA victims with PTSD symptoms at both T1 and T2)—and verified the effects of subgroup on PTSD score change. This model was used to evaluate the subgroup, time, and subgroup×time interaction as well as baseline demographics and psychiatric status at T1.
RESULTS
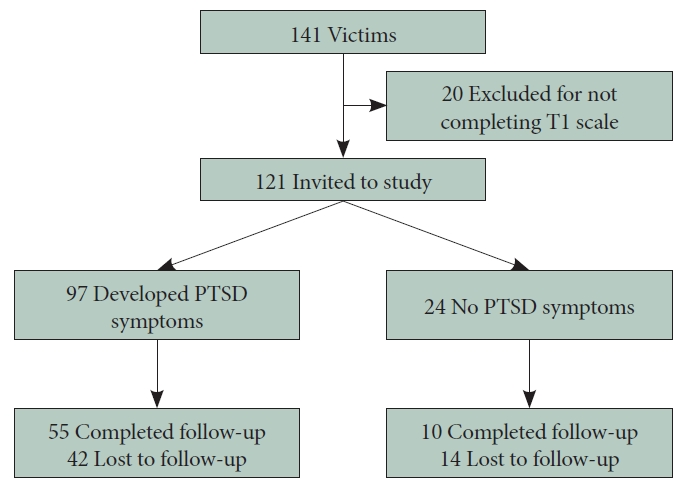
Among 141 participants, 20 individuals were excluded from the study due to non-completion of baseline questionnaires, and total 121 SA victims were included in the study. Throughout the study, 56 of 121 subjects in the victims group were lost to follow-up at T2 (Figure 1).
Descriptive statistics
Descriptive statistics for sociodemographic characteristics and the psychological symptom severity at baseline are presented in Table 1.
In a comparison of these characteristics between those who attended the measurement at T2 and those who did not, there were no significant differences in all of the characteristics (Table 2).
Factors associated with PTSD remission in multivariate analyses
Binary logistic regression analysis of PTSD remission state at T2
The first multivariate analysis was performed using a binary logistic regression model to determine the ORs for victims with and without PTSD remission. We conducted an analysis on 55 victims who participated at both T1 and T2 and exhibited PTSD symptoms based on PDS-5 scores at T1. The Hosmer-Lemeshow test was used to determine the goodness of fit of the model, with p>0.05 taken to indicate that the model showed a good fit to the data.
To obtain the optimal logistic regression model for PTSD remission state, a logistic backward analysis was performed (Table 3). Based on the results, both BAI (anxiety) and SVQ at baseline were incorporated into the final model and significantly associated with PTSD remission state at T2 (BAI, p=0.003; SVQ p=0.024). Participants with anxiety symptoms after SA showed a 1.214-fold greater chance of exhibiting PTSD symptoms at T2, and SVQ 1.048-fold, respectively (Table 3).
No other baseline sociodemographic and premorbid psychiatric characteristics showed associations with PTSD remission.
Linear mixed model of PTSD symptom change, PDS-5 change from T1 to T2
We performed a linear mixed analysis to verify the longitudinal effects of time (from T1 to T2) and subgroup (victim group subdivided into no symptom group, remission group, non-remission group) on PDS-5 score throughout the study. Contrary to logistic regression model, victims without PTSD symptoms group were incorporated into analysis, as well as victims with PTSD symptoms. A total of 121 were analyzed including 56 participant who did not follow up at T2.
The results showed no significant relations of demographic variables with the PDS-5 score change (Table 4). In terms of the psychiatric scales at baseline, the CES-D (depression) and BAI (anxiety) scores were found to be significant variables leading to changes in PDS-5 from T1 to T2 (BAI, p<0.001; CES-D, p<0.001) (Table 4).
Both time and the group×time interaction were shown to be significant variables for the change in PDS-5 (p<0.001, respectively). The group effect was not significant (p=0.654) (Figure 2).
DISCUSSION
The objective of this study was to determine the factors affecting the longitudinal course of PTSD related to sexual trauma. The key finding is that PTSD remission varied by the presence of depressive, anxiety symptoms, and secondary victimization.
These observations support the results of previous studies. The previous study divided SA victims into four groups according to the change in PTSD symptoms after trauma and identified the presence of depressive symptoms related to trauma as a predictor of PTSD non-remission [13]. Self-blame and depression were identified as predictors in another study of factors predicting the level of symptoms after 6 months in patients with sexual trauma-related PTSD [22]. With regard to anxiety related to PTSD, it was reported that secondary anxiety disorder after trauma could affect PTSD remission [7].
We conducted two main analyses for this study. Regarding the logistic regression analysis, we targeted people with clinically significant PTSD symptoms after SA, and found that anxiety and secondary victimization were related with the PTSD symptoms 1 year after the trauma. In the linear mixed model, the analysis included all SA victims. The main purpose of this analysis was to evaluate which factors affects PTSD symptom remission (over 30% decrease of PTSD symptom severity) and to examine the group and time effect on the PTSD symptom change. We were able to find the effect of time, the interaction between group and time on the symptoms of PTSD at T2, and we could confirm that depressive and anxiety symptoms are significant predictors for PTSD symptom severity one year from SA.
There were differences in the results of our binary logistic model and linear mixed analyses. These differences may have been due to differences in the range of subjects between the two analyses. The subjects included in our binary regression analysis were limited to SA victims with PTSD symptoms at baseline in contrast to our linear mixed analysis, which included all of the victims. Specifically, the victims with no PTSD symptoms at baseline were excluded from binary analysis. These differences in subject range may have led to the different conclusions regarding the predictive factor of the longitudinal course of PTSD. These results can be interpreted as follows. Symptom remission in SA victims who have PTSD symptoms but do not meet the PTSD diagnostic criteria is related to the severity of depression and anxiety. But only anxiety played a significant role in the SA victim group who met the PTSD diagnosis. In other words, depression and anxiety affect whether PTSD symptoms improve after SA, but depression is important in symptom remission at a subclinical level, and anxiety plays a major role not only in subclinical but also in clinical areas.
Furthermore, this study suggests that post-trauma secondary victimization can affect PTSD symptom remission. Especially in the case of SA victims, who can experience various types of secondary psychological stress from both formal and informal sources, these secondary psychological stressors can affect the persistence of PTSD symptoms.
These results are noteworthy in determining not only the effects of secondary victimization from administrative and medical procedures on SA victims, but also in identifying specific longitudinal effects on mental health, such as PTSD. Although there have been many studies related to the effects of social reactions on the expression of PTSD symptoms and future remission [12,16,18,20,45], most of these studies dealt with the effects of support received from family, friends, and acquaintances, and not the secondary victimization from administrative and medical procedures.
Strengths and limitations
This study is meaningful in that it was conducted with a population consisting of all SA victims visiting a crisis intervention center, in contrast to most previous studies that were performed with patients who visited the hospital with PTSD symptoms after SA [7,11,16,17,20,21,42,45]. Therefore, prior studies might have excluded not only SA victims who did not develop PTSD symptoms, but also those who did not receive hospital treatment, thus leading to selection bias. In addition, this study is prospective designed, so the possibility of false reports or recollections of SA could be excluded in contrast to previous studies. In previous studies, SA was identified retrospectively based on patients’ reports using questionnaires, leading to recollection bias [11].
However, this study also had some limitations. First, 42 of the 97 SA victims who showed initial PTSD symptoms and 14 of the 24 who showed no PTSD symptoms were lost to follow-up at T2. The lack of data on the actual characteristics of the subjects who were lost to follow-up and the presence or absence of symptoms at T2 could result in problems in interpreting the results. This frequent loss to follow-up has been noted in previous studies related to SA. Dworkin et al. [29] reviewed and synthesized the results of longitudinal studies of PTSD related to SA, and reported that 45.5% of SA victims did not participate in 1-year follow-up in longitudinal studies to evaluate PTSD symptoms after SA. This frequent loss to follow-up may be due to the stigmatizing nature of SA.
Second, the reliability of this study was low because all of the scores were obtained by self-reporting. Although the self-reported PDS-5, the main score used in this study, is an effective screening tool for PTSD, clinician-administered PTSD scales, such as Clinician-Administered PTSD Scale for DSM-5, may be more accurate for the evaluation of PTSD symptoms.
Conclusions and directions for future research
The results of the present study showed that depression, anxiety, and secondary victimization from administrative and medical procedures were associated with PTSD symptom remission state, 1 year after SA. Identification of the factors associated with poor PTSD outcomes using a longitudinal approach could improve our ability to identify patients at risk of PTSD non-remission in advance and help to develop tailor-made preventive interventions for SA victims.
Further study is required to reduce the high dropout rate, which may be responsible for the frequent conflicting results in studies related to sexual trauma.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Jae-Won Kim. Data curation: Jae-Won Kim, Kihyun Kim. Formal analysis: Jaewon Lee, Jiyoon Shin. Funding acquisition: Jae- Won Kim. Methodology: Jae-Won Kim. Project administration: Jae-Won Kim. Resources: Jae-Won Kim. Supervision: Jiyoon Shin, Soohyun Chae, Jeeyoung Chun, Jae-Won Choi, Ju-Yeon Lee, Tae-Won Park, Kyoung Min Kim, Kihyun Kim, Jae-Won Kim. Writing—original draft: Jaewon Lee. Writing—review & editing: Jaewon Lee.
Funding Statement
This research was funded by Korea Mental Health Technology R&D Project (ID: HM15C1107). We cooperated with eight Sunflower Centers: Seoul, Gwangju (Child), Gwangju (Crisis), Northwestern Gyeonggi, Gyeongnam, Busan, Jeonbuk, and Chungnam.