Psychiatric Symptoms in Temporal Lobe Epilepsy with Left Mesial Hippocampal Sclerosis
Article information
Abstract
A 16-year-old woman was referred to us for depression and persistent suicidal and homicidal ideation. From 2010, the patient visited a neurologist due to recurrent grand mal epilepsy, auditory and visual hallucinations, episodic memory loss, and persistent depression. Upon admission, it was revealed through clinical history taking that she had suffered from chronic bullying from same-sex peers and sexual abuse, twice, from an adult male in the neighborhood when she was 10 years old. A brain magnetic resonance imaging study showed left mesial hippocampal sclerosis. The patient exhibited improvement of her psychiatric symptoms after treatment with a combination of fluoxetine (30 mg) and aripiprazole (10 mg). Children and adolescents with epilepsy experience conflicts in the family, challenges at school, stigma, and psychosocial limitations or deprivations due to their comorbid psychiatric symptoms and hence, psychiatric evaluation and early intervention is important when treating these patients.
INTRODUCTION
The prevalence of psychiatric disorders is higher in people with epilepsy than in the general population. In patients with epilepsy, depression occurs in about 30%, anxiety disorders in 10-25%, and psychosis in 2-7%.1 Thus, these patients are more likely to have psychiatric diseases,2 and are more than three times as likely to commit suicide as the general population.2,3 About 5% of the adolescents in the community have Major De-pressive Disorder (MDD) and another 3.3% have dysthymia.3 Evidence showed that MDD is associated with smaller hippocampal volumes.4,5,6 A previous study found that subjects with depression and a history of childhood abuse had an 18% smaller mean left hippocampal volume than those never abused, and a 15% decrease in comparison with healthy subjects.7 In identifying teenagers with suicidal tendencies, factors such as a family history of suicide, alcohol and drug abuse, previous suicide attempts, and self-destructive behavior may be valuable. The most significant psychiatric risk factor associated with adolescent suicide is MDD.8 Homicide-suicide perpetrators are also often found to suffer from mental illness, with depression being the most common disorder.9 In young people with epilepsy, depression and other psychiatric disorders are common but often remain undiagnosed and untreated. Until now, no previous studies have reported a relationship between hippocampal lesions and homicidal or suicidal ideation. Here, we report the case of a 16-year-old woman with temporal lobe epilepsy showing persistent suicidal and homicidal ideation and depressed mood and discuss the efficacy of psychiatric intervention for temporal lobe epilepsy.
CASE
In August 2013, a 16-year-old woman was referred to us for depression, persistent suicidal and homicidal ideation, episodic memory loss, and personality changes. The patient often forgot what she did, talked about, or when she took a meal. From 2010, the patient visited a neurologist due to recurrent grand mal epilepsy, auditory and visual hallucinations, episodic memory loss, and persistent depression. She underwent electroencephalogram (EEG) assessment, which presented slow or sharp waves and spikes. After taking antiepileptic drugs, the symptoms of epilepsy, hallucinations, and episodic memory loss improved and resolved the epileptic waves on EEG, but her depression symptoms became aggravated. Suicidal and homicidal ideations toward her family and schoolmates continued. She showed personality changes such as becoming impatient and isolating herself extremely from peers. In October 2013, although she had psychological counseling for depression, symptoms of repeated self-injurious behaviors and suicidal and homicidal ideations were not improved. In January 2013, neurologists treated her with lamotrigine (up to 200 mg), but her symptoms did not improve. In August 2013, she was admitted for further evaluation and treatment.
Upon admission, clinical history taking revealed that she had suffered from chronic bullying and victimization from same-sex peers, and had been sexually abuse, twice, by an adult male from her neighborhood when she was 10 years old. On mental state examination (MSE), she endorsed present suicidal and homicidal ideation, depressed mood, repeated nightmares, and flashbacks about bullying or sexual abuse. Routine blood tests, including complete blood count, serum electrolyte, creatinine, glucose, and vitamin B12, vitamin E, and folate, autoimmune serologies, and electrocardiogram (ECG), chest X-ray, and EEG showed no aberrant findings. However, brain magnetic resonance imaging (MRI) study detected left mesial hippocampal sclerosis (Figure 1).
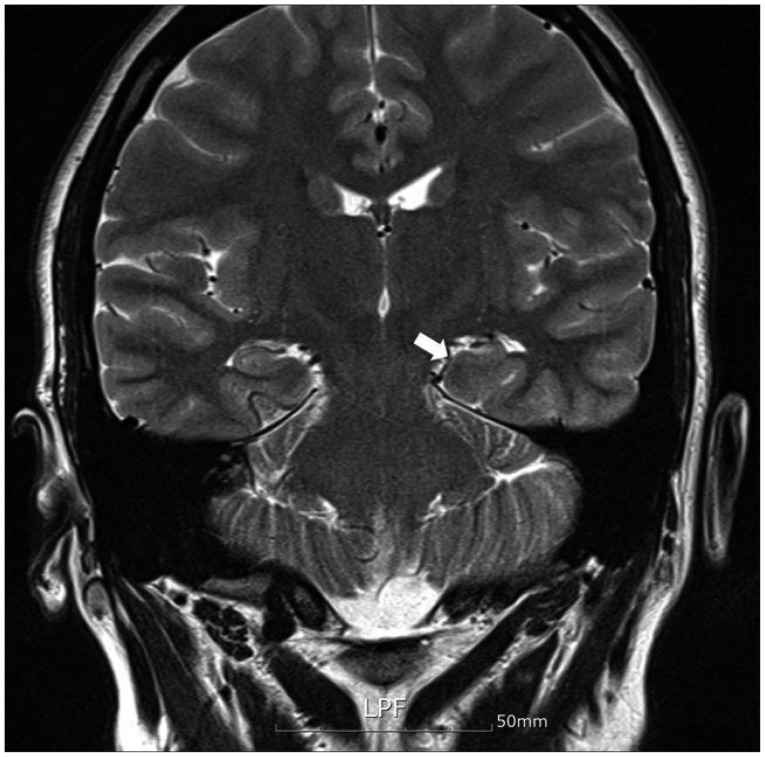
Brain magnetic resonance image (MRI) showing the decrease in size of the left hippocampus with loss of gray-white differentiation. This observation is consistent with mesial temporal sclerosis.
On the 2nd day, fluoxetine was administered starting from 10 mg up to 40 mg. On the 21th day, she showed frequent episodic memory loss at the highest dose. Considering the adverse effect of selective serotonin reuptake inhibitors (SSRIs) such as a decreased seizure threshold, fluoxetine was decreased to 30 mg. Aripiprazole was administered starting from 2 mg up to 10 mg, to augment the SSRI activity. On the 28th day, she underwent follow-up neuropsychological assessments, which showed improvements in depression, suicidal ideation, and homicidal ideation. She also showed a decrease of episodic me-mory loss as improvement in depressive symptoms. Upon discharge, the 35th day from admission, most symptoms had significantly improved on follow-up neuropsychological scales (Table 1). After discharge, she regularly visited us as an outpatient and neither depressive symptoms nor suicidal and homicidal ideation appeared again during this period.
DISCUSSION
In this case report, we present the case of a 16-year-old woman with temporal lobe epilepsy showing persistent suicidal and homicidal ideation, and depressed mood, which improved after taking fluoxetine with aripiprazole augmentation.
The patient presented with temporal lobe epilepsy with left mesial hippocampal sclerosis and psychiatric symptoms including sustained depression, and repetitive suicidal and homicidal ideations. Hippocampal sclerosis describes a pattern of neuronal loss and gliosis involving the medial temporal structures most often encountered in patients with epilepsy.10 Evidence has emerged in the past decade that MDD is associated with small hippocampal volumes.4,5,6 A previous study reported that children and adolescents with temporal lobe epilepsy had moderate to severe depressive symptoms early in the course of their disease, with an impact on their global functional activities.11 A previous study found that people with epilepsy were four times more likely to be hospitalized than people without epilepsy, and 30% had attempted suicide.12 Of the suicides committed by people with epilepsy, 81% to 100% occur among those with a co-morbid psychiatric disorder, most commonly depression.13 Antiepileptic drugs (AEDs), especially barbiturates, are frequently involved in suicides and attempts.14 In 2008, the U.S. Food and Drug Administration (US FDA) issued an alert to healthcare professionals about an increased risk of suicidal thoughts and increased suicidality in people taking AEDs. The overall odds ratio (OR) for spontaneously reported suicidal behavior or ideation among those taking active drugs was 1.8 (95% CI: 1.24-2.66).15 In this case, after the patient took AEDs, her psychiatric symptoms, depression, and suicidal ideation were aggravated, which suggested an association between AEDs and psychiatric symptoms.
In addition, she experienced chronic bullying and physical abuse during childhood and sexual abuse twice at age 10. Childhood sexual abuse is a significant early stressor that may predispose individuals to depression and self-destructive behaviors in adulthood. Previous research found reduced hippocampal volume in victims of psychological trauma with severe sexual or physical abuse in childhood.16 Previous suicide attempts, suicidal ideation, and homicidal ideation were also associated with adolescent suicide.8 Thus, we considered the association between her psychiatric symptoms, chronic bullying, repeated physical and sexual abuse, and her temporal lobe epilepsy.
The patient showed improvement of psychiatric symptoms in combination treatment with fluoxetine and aripiprazole. Fluoxetine is the only SSRI approved by the FDA for the treatment of depression in patients younger than 18 years of age.17 Previous research suggested that reduced serotonin receptor 5-HT1A binding may be related to the increased incidence of depression in patients with epilepsy, due to the reduction of serotonergic neurotransmission in hippocampal epileptic foci.18 Thus, SSRIs may be considered for the treatment of depression in adolescents with epilepsy. Antipsychotics are used not only in the treatment of psychotic disorder such as schizophrenia, but also as adjuncts for depressive disorder. Augmentation with atypical antipsychotic agents was significantly more effective than placebo for response and remission.19 Aripiprazole received FDA approval for adjunctive therapy in patients with MDD. The product label of aripiprazole recommends a starting dosage of 2-5 mg/day, with a target range of 5-15 mg/day.20 In a previous study, the mean dose at the end of double-blind treatment was 11.8 mg/day, suggesting that the effective dose for patients with major depressive disorder is lower than that recommended for schizophrenia and bipolar disorder.21 There was a previous case of a 13-year-old boy on aripiprazole and fluoxetine for depression with persecutory delusions, auditory hallucinations, and a suicide attempt.22 In this case, we suggest that the combination of fluoxetine and aripiprazole has therapeutic effects in children and adolescents with temporal lobe epilepsy.
In conclusion, psychiatric symptoms such as depression and suicidal and homicidal ideas are more common in patients with temporal lobe epilepsy. Unfortunately, however, they are often undiagnosed and untreated. Children and adolescents with epilepsy experience acute and chronic stressors such as family conflicts, difficulty in school performance, stigma, and psychosocial limitation or deprivations due to comorbid psychiatric symptoms. Thus, we consider that psychiatric evaluation and early intervention are important for children and adolescents with epilepsy. In the future, longitudinal and prospective studies for the biological underpinnings and treatment of psychiatric symptoms comorbid with temporal lobe epilepsy are needed.
Acknowledgments
This study was supported by research fund from Chosun University in 2013.
