Psychometric Analysis of the Obsessive–Compulsive Spectrum Self-Report and Social Anxiety Spectrum Self-Report in the Korean Population
Article information
Abstract
Objective
The present study aimed to assess the psychometric properties of the Korean versions of the Obsessive–Compulsive Spectrum Self Report (OBS-SR) and the Social Anxiety Spectrum Self Report (SHY-SR) questionnaires, along with determining their optimal cut-off points in a Korean population.
Methods
The study included outpatients with obsessive-compulsive disorder (OCD) (n=86), or social anxiety disorder (SAD) (n=52), those with major depressive disorder (MDD) (n=27), and 33 healthy controls. Participants were administered the Korean versions of the OBS-SR and SHY-SR questionnaires. Clinical symptoms were also assessed with several self-rating scales.
Results
The Korean versions of the OBS-SR and SHY-SR demonstrated good internal consistency, test-retest reliability, and convergent validity. Both questionnaires effectively differentiated between individuals with OCD or SAD and normal controls or those with MDD. Receiver-operating characteristic analyses of the OBS-SR and SHY-SR yielded area under the curve values of 0.89 and 0.96 for Diagnostic and Statistical Manual of Mental Disorders, Forth Edition diagnosis, respectively, and showed optimal threshold values of 50 and 44.
Conclusion
The Korean versions of OBS-SR and SHY-SR demonstrate good reliability and validity in assessing manifestations of obsessive-compulsive and social anxiety psychopathology in Korean populations.
INTRODUCTION
Despite notable advancements in the assessment of psychiatric disorders over the past several decades, the ongoing debate between the categorical and dimensional approaches to psychiatric classification remains a contentious issue [1-3]. While the categorical system seeks to establish distinct boundaries and discrete disease entities, such as those outlined in [4], it tends to overlook subtle or subthreshold conditions. The categorical approach is challenged by its limited ability to clearly demarcate clinical conditions from one another, potentially neglecting the practical significance of subthreshold changes and normality. In contrast, the dimensional system adopts a continuity perspective, considering these subtler states. Therefore, there has been a growing interest in dimensional approaches and spectrum models as a valuable complement to the categorical approach [5]. The spectrum model [6] offers a flexible and comprehensive framework for comprehending complex clinical conditions and describing intricate symptoms, including those associated with obsessive-compulsive tendencies and social anxiety.
Obsessive–compulsive phenomena or obsessional tendencies may manifest either as a discrete obsessive-compulsive disorder (OCD) or as part of other psychiatric syndromes, such as schizophrenia or specific personality traits [7]. Defining precise boundaries between normal or subclinical states and pathological obsession/compulsion presents several challenges [8-10]. Similarly, symptoms regarding social anxiety disorder (SAD) encompass various dimensions, including social anxiety, shyness, behavioral inhibition, and avoidant personality traits, making it challenging to categorically distinguish them as discrete diagnoses such as SAD [11,12]. These conditions have been conceptualized within the spectrum and dimension framework of SADs [13,14].
Aligned with the spectrum concept, several instruments based on the spectrum model have been developed, including the Obsessive–Compulsive Spectrum Self-Report (OBS-SR), tailored to gauge a diverse array of obsessive–compulsive phenomenology and the Social Anxiety Spectrum Self-Report (SHY-SR) [15] designed to assess social anxiety manifestations [15]. These spectral questionnaires assess a wider range of symptoms than those typically characterized by the Diagnostic and Statistical Manual of Mental Disorders (DSM) [4], including temperamental and personality traits. The questionnaires were developed based on a spectrum approach that focuses on soft signs, subthreshold syndromes, and temperamental and personality traits as part of the clinical and subsyndromal manifestations of obsessive–compulsive and social anxiety psychopathology [15,16].
The present study aimed to assess the psychometric properties of the Korean versions of the OBS-SR and SHY-SR questionnaires in clinical and non-clinical groups. In particular, we examined whether these questionnaires could accurately identify quantitative distinctions between groups of individuals with OCD or SAD and those without these conditions, including individuals with major depressive disorder (MDD). In addition, we sought to determine their optimal cut-off points for screening OCD or SAD in a Korean population.
METHODS
Participants
The participants comprised three clinical samples: OCD, SAD, and MDD, as well as non-clinical sample of healthy adults. In the OBS-SR study, the participants included 86 patients with OCD without a current or lifetime history of MDD, 25 patients with MDD without a current or lifetime history of OCD, and 33 healthy controls. In the SHY-SR study, the participants included 52 patients with SAD without a current or lifetime history of MDD, 27 patients with MDD without a current or lifetime history of SAD, and 32 healthy controls. A trained psychiatrist assessed all the patients using the patient version of the Structured Clinical Interview for DSM-IV (SCID) [17]. Healthy controls were recruited from the local community and assessed for any current or past DSM-IV Axis I disorder using the SCID non-patient version. Patients with a neurological or significant medical illness, a history of electroconvulsive therapy, and current or past substance abuse or dependence were excluded. Patients with OCD were administered the OBS-SR and the Maudsley Obsessional Compulsive Inventory (MOCI), whereas those with SAD were administered the SHY-SR and Liebowitz social anxiety scale-self report (LSAS-SR). As control groups, patients with MDD and healthy controls completed both of the OBS-SR and SHY-SR. A subsample of 48 patients with OCD and 34 patients with SAD completed the OBS-SR and SHY-SR again after approximately 4 weeks to explore the test–retest reliability of the two scales. The Institutional Review Board of Severance Hospital approved the study protocol (4-2005-0077), and written informed consent was obtained from all participants prior to their involvement in the study.
Measures
OBS-SR
The OBS-SR (183 items) is a self-report questionnaire that measures seven domains of obsessive–compulsive psychopathology [15]. These domains are as follows: 1) childhood/adolescence experiences (23 items), which measure early obsessive– compulsive traits such as excessive worry, perfectionism, and the need for control, 2) doubt (13 items): this domain measures insecurity and uncertainty, such as frequent second guesses and indecisiveness, 3) hypercontrol (55 items): this domain measures the tendency to be cautious, responsible, and emotionally controlled, as observed in behaviors such as excessive checking or avoidance of risky situations, 4) attitudes toward time (9 items): this domain measures the use of time, such as compulsive slowness and difficulty in making decisions, 5) perfectionism (18 items): this domain measures the inclination to be orderly, precise, and symmetrical, with a preference for things to be done exactly the way they are expected, 6) repetition and automation (12 items): this domain measures the tendency to repeat behaviors or thoughts repeatedly, 7) specific themes (53 items): this domain measures obsessive–compulsive traits related to specific topics, such as contamination, cleaning, sexuality, religion, and existentialism. The OBS-SR is answered with either “yes” or “no” for each item, and the total score is determined by summing the number of items endorsed as “yes.”
SHY-SR
The SHY-SR is a 168-item self-report questionnaire measuring the lifetime spectrum of social anxiety [15]. The questionnaire focuses on four general domains: 1) childhood and adolescence social anxiety features (12 items): this domain assesses fear and phobia-related avoidance of social activities during childhood and adolescence, such as school and sports, 2) interpersonal sensitivity (29 items): this domain explores the extent to which a person is sensitive to criticism, rejection, close observation, discomfort in being the center of attention, low self-confidence, feelings of inferiority, a low ability to impose oneself on others, and difficulties in interpersonal relations, 3) behavioral inhibition and somatic symptoms (23 items): this domain emphasizes specific social behaviors and somatic symptoms related to social anxiety, such as blushing, sweating, trembling, and nausea, 4) specific phobias (98 items): this domain identifies situations that may provoke social anxiety, avoidance, and anticipatory anxiety, such as public speaking, eating in front of others, and using public bathrooms. For each item, respondents were asked to make a dichotomous choice between yes and no. The domain and total scores were calculated by counting the number of items to which the respondent answered yes. The questionnaire has an appendix (six items) on psychoactive substances (tobacco, alcohol, benzodiazepines, cannabis, street drugs, and other drugs), a common complication of SAD, but it was not included in the total score.
Korean Versions of the OBS-SR and SHY-SR
A Korean psychiatrist fluent in both English and Korean translated the OBS-SR and SHY-SR scales from English to Korean after obtaining copyright permission from the original author, Dr. Dell’Osso. Two bilingual Korean psychiatrists reviewed the preliminary translations. We administered the translated questionnaire to five individuals from diverse sociodemographic backgrounds and asked them whether they had encountered any perplexing or challenging questions. Subsequently, a bilingual psychiatrist who had no prior exposure to the original OBS-SR and SHY-SR translated the Korean version into English. Finally, the English translation of the items and their original English versions were compared. In cases where discrepancies emerged between the back-translated and original items, the initial translator provided a secondary Korean translation after reviewing the original and back-translations. The second translation was considered satisfactory.
MOCI
The MOCI [18] is a self-rating instrument with 30 dichotomous items designed to measure obsession and compulsion symptoms. It comprises four subscales: checking, washing, doubting and slowness. The MOCI has good reliability and validity [19] and has been validated in a Korean population [20].
LSAS-SR
The LSAS-SR [21] comprises 24 items that assess social anxiety. It included four subscales: performance fear, performance avoidance, social fear, and social avoidance. For each item, the respondents rated how fearful and avoidant they were during the past week on a scale of 0 to 3. This scale has good reliability and validity [22] and it has been validated in a Korean population [23].
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 26.0 for Windows (IBM Corp., Armonk, NY, USA). Demographic variables and scores of the scales were compared among the groups using analysis of variance with the least significant difference post-hoc pairwise test or the chi-square test. The Kuder–Richardson coefficients, a specific type of Cronbach’s alpha [24] for dichotomous items, and corrected domain-total correlations were used to verify the internal consistency and reliability of the OBS-SR and SHY-SR. Internal consistency was considered good at alpha >0.7 [25] and corrected domain-total correlation coefficient >0.4 [26]. We evaluated the test–retest reliability using the intraclass correlation coefficient (ICC) along with a 95% confidence interval. This assessment was performed on the total OBS-SR and SHY-SR scores at both the baseline and the 4-week mark, utilizing data obtained from a subset of patients with OCD and SAD. The ICC values >0.7 indicated good reliability [27]. Pearson’s correlation coefficients were calculated between the domains of each scale to assess the validity of the OBS-SR and SHY-SR internal structures. To establish convergent validity, we analyzed the Pearson’s correlations between the domains of the OBS-SR and SHY-SR and the established scales for OCD and SAD, including MOCI for OCD and LSAS-SR for SAD, in patients with OCD and SAD, respectively. The significance of correlations was considered acceptable when p<0.01. In addition, correlations were considered negligible if the correlation coefficient was <0.3, moderate if it was between 0.3 and 0.5, or strong if it was >0.5 [28]. To assess known-group validity, an analysis of variance was conducted to compare the mean scores on the OBS-SR or SHY-SR domains between the OCD or SAD, MDD, and normal control groups. Receiver-operating characteristic (ROC) curves were used to determine the optimal cut-off points for the OBS-SR and SHY-SR and to assess their ability to discriminate between participants with and without OCD and SAD, respectively. The optimal cut-off points for the OBS-SR and SHY-SR were determined using the highest Youden Index, indicating maximization of sensitivity and specificity (the sum of sensitivity and specificity minus one) [29]. The sensitivity and specificity of the scales were calculated using these cut-off points. An area under the curve (AUC) value of ≥0.70 is considered to be indicative of good discriminative capacity and diagnostic accuracy [30].
RESULTS
Table 1 presents the demographic characteristics of the participants in the OBS-SR and SHY-SR studies, respectively. The frequency distribution of the total OBS-SR and SHY-SR scores in the patient and normal groups is shown in Figures 1 and 2. Means for the domains and total scores of the questionnaires are provided in Supplementary Table 1 (in the online-only Data Supplement).

Demographic characteristics of the overall sample; patients with OCD or SAD, patients with MDD, and normal controls
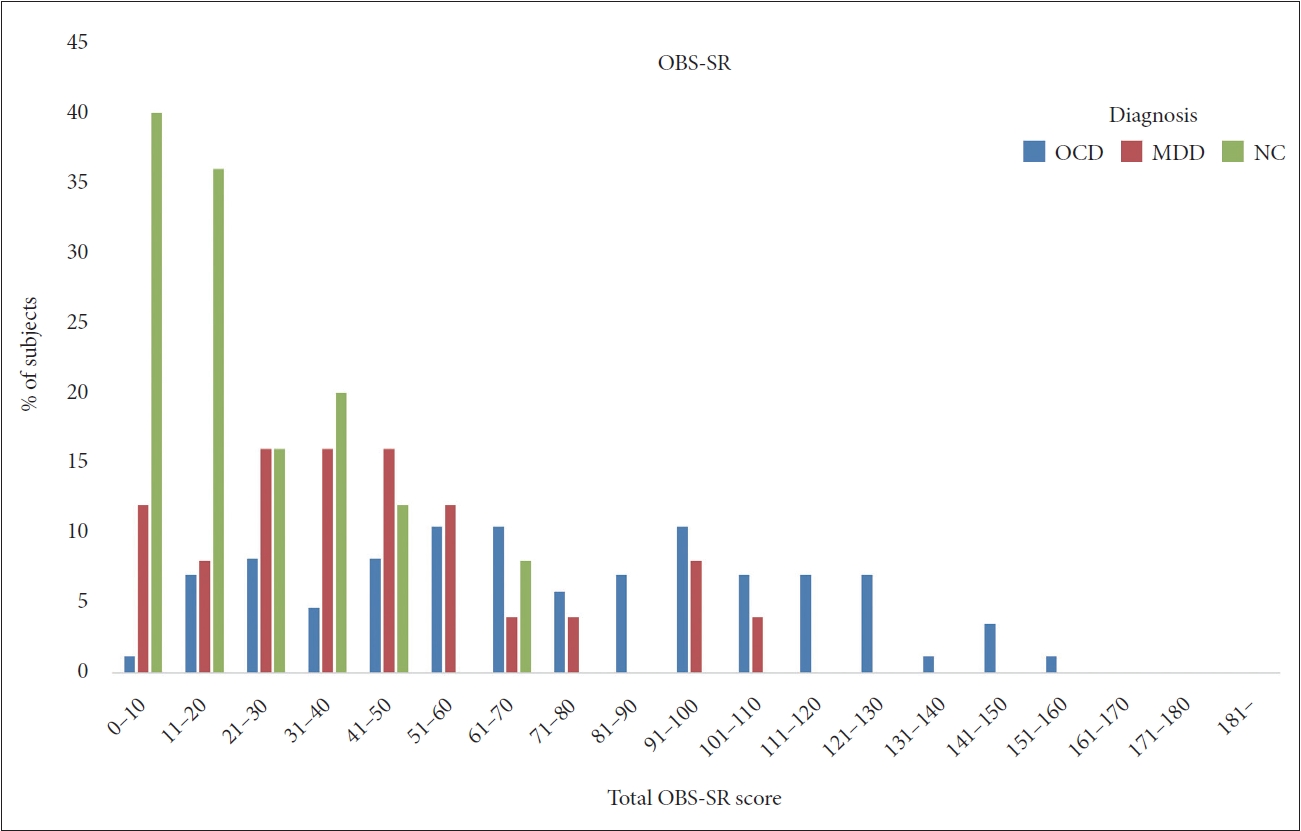
Frequency distribution of total OBS-SR scores among groups with OCD, MDD, and NC. OCD, obsessive–compulsive disorder; MDD, major depressive disorder; NC, normal controls; OBS-SR, Obsessive–Compulsive Spectrum Self-Report.
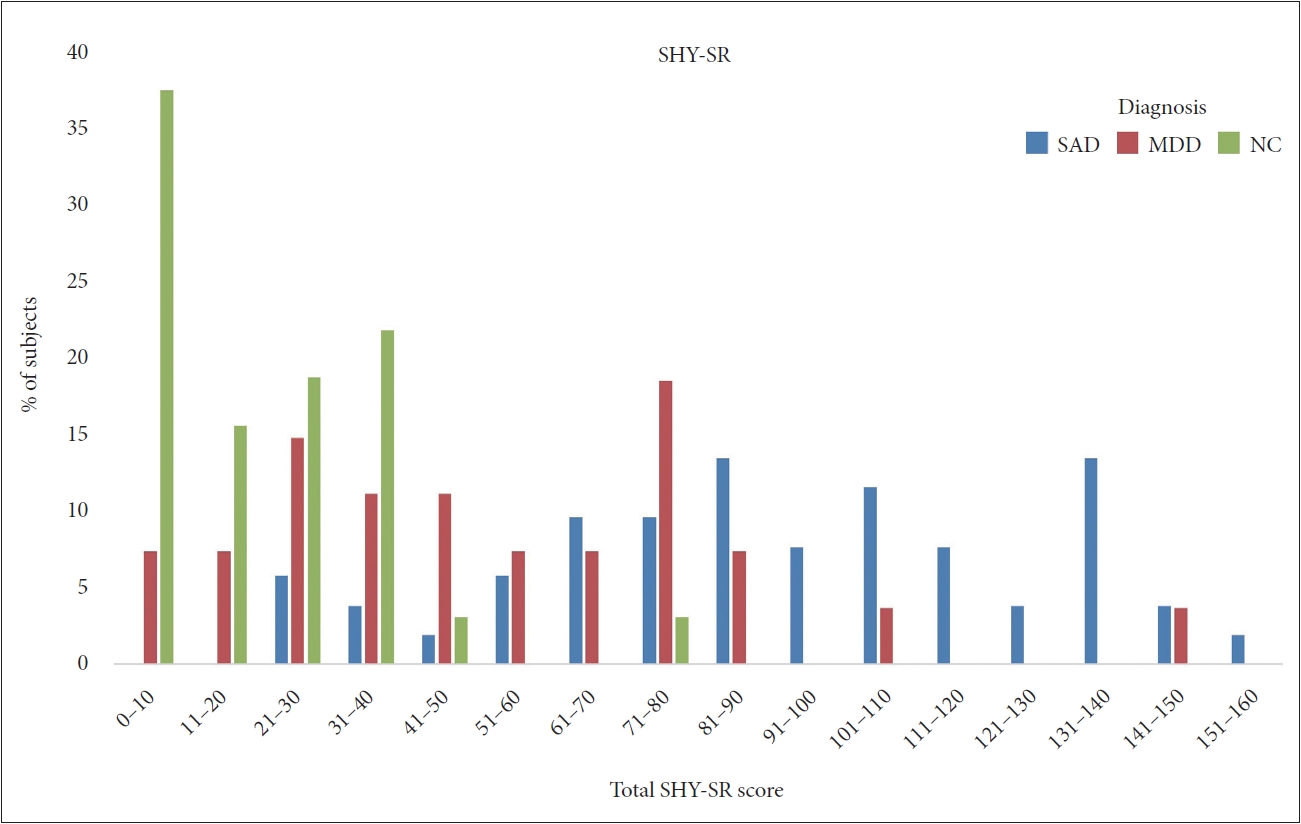
Frequency distribution of total SHY-SR scores among groups with SAD, MDD, and NC. SAD, social anxiety disorder; MDD, major depressive disorder; NC, normal controls; SHY-SR, Social Anxiety Spectrum Self-Report.
Reliability
The Kuder–Richardson coefficients for each domain, total score, and corrected domain-total correlation in the whole sample were corrected for domain-total correlation for the OBS-SR and SHY-SR and are listed in Table 2, respectively. The reliability coefficients of all OBS-SR domains and the total scale and the corrected domain-total correlation coefficients of all OBS-SR domains were 0.745–0.982 and 0.720–0.900, respectively. The test–retest reliability indices of the OBS-SR total and domain scores, as assessed using ICCs, ranged from 0.838 to 0.941. The reliability coefficients of all SHY-SR domains and the total scale ranged from 0.899 to 0.988. The corrected domain-total correlation coefficients of all SHY-SR domains ranged from 0.762 to 0.899. The ICC for the overall and specific domain scores of the SHY-SR ranged from 0.773 to 0.915 [31].
Validity of the internal structure
The Pearson correlation coefficients between the OBS-SR and SHY-SR domain scores and the total scores were statistically significant and positive, with r values >0.5. The results are shown in Table 3, respectively.
Convergent validity
Pearson’s correlation coefficients for each domain and the total scores of the OBS-SR with the subscales and total scores of the MOCI are listed in Table 4. All but two correlation coefficients were statistically significant and positively correlated, with an r-value of at least 0.3. The correlation coefficients between attitude toward the time domain of the OBS-SR and the doubting subscale of the MOCI and the specific theme domain of the OBS-SR and the doubting subscale of the MOCI were <0.3.
In the SHY-SR study, Pearson’s correlation coefficients for each domain and the total scores of the SHY-SR with the subscales and total scores of the LSAS-SR are listed in Table 4. All correlation coefficients were statistically significant, and positive correlations with r ranged from 0.350 to 0.719.
Known-group validity
Comparisons of the domains and total scores of the OBSSR for patients with OCD with those for patients with MDD and healthy controls are presented in Supplementary Table 1 (in the online-only Data Supplement). All domain and total OBS-SR scores of patients with OCD were significantly higher than those of patients with MDD or normal controls. As shown in Supplementary Table 1 (in the online-only Data Supplement), there were significant differences in mean scores for each domain and the total SHY-SR scores among patients with SAD, patients with MDD, and normal controls. Patients with SAD had significantly higher scores in all domains and total SHY-SR scores compared to both patients with MDD and normal controls. Furthermore, patients with MDD had significantly higher scores in all SHY-SR domains compared to normal controls.
ROC analyses for criterion validity
The ROC analyses of the OBS-SR yielded an AUC of 0.894 (standard error [SE]=0.029) when compared to OCD diagnosed by a psychiatrist based on the DSM-IV. An OBS-SR cut-off score of 50 had the most appropriate sensitivity and specificity for the diagnosis of OCD. Sensitivity and specificity were 0.709 and 0.939, respectively (Figure 3).

ROC curves for the OBS-SR. AUC=0.894, p<0.001, 95% CI [0.825, 0.943], SE=0.029. ROC, receiver operating characteristic; OBS-SR, Obsessive–Compulsive Spectrum Self-Report; OBS_total, Total OBS-SR score; AUC, area under the curve; SE, standard error; CI, confidence interval.
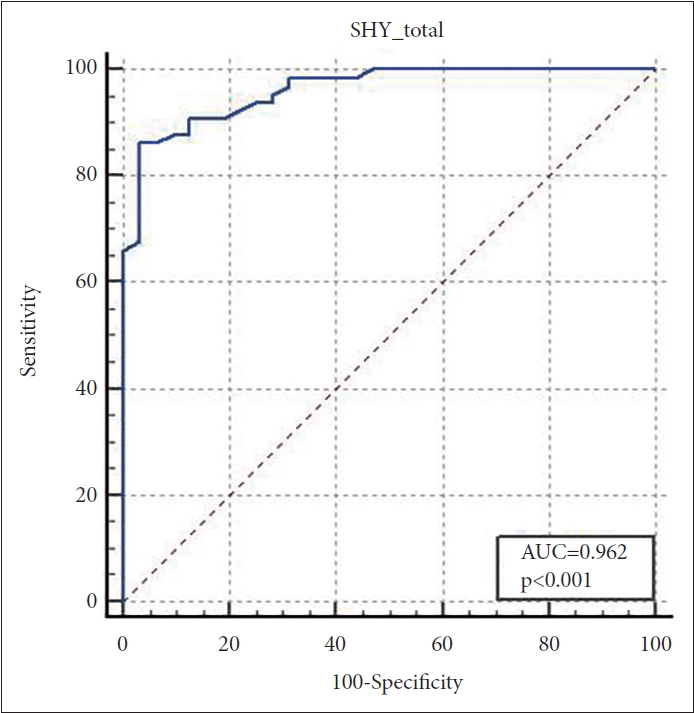
On the other hand, the ROC analysis of the SHY-SR yielded an area under the curve of 0.962 (SE=0.017) for the SAD diagnosis based on the DSM-IV. A SHY-SR cut-off score of 44 indicated a sensitivity of 0.862 and a specificity of 0.969 (Figure 4).
DISCUSSION
The present study investigated the psychometric properties of the Korean versions of the OBS-SR and SHY-SR in clinical and non-clinical samples. The OBS-SR is designed to assess the core symptoms of OCD as well as atypical presentations, personality traits, and other clinical features associated with these disorders [15,32]. The SHY-SR is a self-administered questionnaire that measures the full range of symptoms associated with social anxiety, including interpersonal sensitivity characterized by mild shyness to inhibition and to severe SAD [15]. The present results showed that the Korean versions of both scales could effectively measure OCD and SAD and had good reliability, validity, and internal consistency while maintaining the robust psychometric properties observed in the original versions of the scales. The findings confirm that the Korean adaptations of the OBS-SR and SHY-SR are acceptable tools for assessing a broad spectrum of obsessive–compulsive and social anxiety symptoms in Korean patients with OCD or SAD in clinical settings, as well as in non-clinical individuals.
Internal consistency reliability for two scales based on the Kuder–Richardson coefficients for each domain, total score, and corrected domain-total correlation in this study was high (greater than 0.7). In the OBS-SR, the lowest coefficient was for attitudes toward the time domain (0.74). The coefficients of this domain were also the lowest in a standardization study of the Spanish versions of the OBS-SR and SHY-SR [33] and a recent validation study of the short version of the OBS [32] (0.61 and 0.76, respectively). In addition, a corrected domain-total correlation analysis was conducted on the OBS-SR and SHY-SR in this study, revealing that each item and the total scores of both scales exhibited correlations exceeding 0.4. This indicates a satisfactory alignment between individual items and overall scores. Moreover, the ICC for test–retest reliability of both scales exceeded 0.7, affirming the temporal stability of the scales.
With respect to convergent validity of the OBS-SR and SHY-SR, significant positive correlations were observed in relation to other extensively used scales for OCD (MOCI) and SAD (LSAS-SR). In the present patients with OCD, all domains and total OBS-SR scores significantly correlated with subscales and total MOCI scores. Nonetheless, the correlation coefficient between the attitude toward the time domain of the OBSSR and the doubting subscale of the MOCI was <0.3, suggesting a negligible correlation. All other domains and total scores of the OBS-SR and SHY-SR were correlated with the MOCI subscale and total score and the LSAS-SR subscale and total score at a moderate level (r>0.3), respectively. A previous Spanish validation study reported moderate correlation coefficients between the OBS-SR and MOCI [33]. Overall, the correlation coefficients in our study were higher than those reported in the Spanish study [33]. For example, the correlation coefficient between the total scores of the OBS-SR and MOCI in the Spanish study was 0.530, whereas it was 0.751 in the present study. In contrast to our findings, a Spanish study found that the washing subscale of the MOCI did not correlate with any domains or total scores of the OBS-SR [33]. This may be due to the difference in composition and sample size included in the analysis for convergent validity. The Spanish study included the sample groups with OCD, MDD, and normal controls, whereas our study comprised patients with OCD [33]. In addition, in the Spanish study, the overall sample size for the analysis of the convergent validity of the OBS-SR was 67, whereas it was 144 in the present study. Unlike MOCI, the OBS-SR evaluates a broad obsessive–compulsive spectrum phenomenology rather than only evaluating key obsessive–compulsive symptoms. Therefore, the correlation coefficient between OBS-SR and MOCI was not very high. Regarding the SHY-SR, the convergent validity findings in our study were consistent with those of a Spanish validation study [33]. This earlier study reported a significant correlation between all domains and total scores of the SHY-SR and all subscales and total scores of the LSAS-SR at levels exceeding moderation. Nonetheless, disparities in sample composition and size existed between the two studies (our study: only SAD [n=52] vs. the Spanish study: SAD [n=20], MDD [n=20], and normal controls [n=25]).
In addition, the Korean versions of the OBS-SR and SHYSR showed excellent known-group validity. Each domain and the total OBS-SR scores in patients with OCD were significantly higher than those in patients with MDD and healthy controls. Further, most of the results remained significant even when the confounding effect of the sex distribution between OCD and MDD was controlled. However, the difference between patients with OCD and MDD changed to the trend significance level (analysis of covariance [ANCOVA], F=3.005, df=2, p=0.054, data not presented) only in the specific theme domain of the OBS-SR. Patients with SAD had significantly higher domain and overall SHY-SR scores than patients with MDD and healthy controls. Most of these results remained significant even when controlling for confounding variables resulting from the difference in sex distribution between patients with SAD and MDD, suggesting that the scale can effectively discriminate between individuals afflicted with SAD and those who do not have the condition. However, the statistical significance of the difference between patients with SAD and MDD disappeared (ANCOVA, F=2.293, p=0.108, data not presented) only in the domain of childhood and adolescence social anxiety features. Moreover, each domain and the total score of patients with MDD were significantly higher than those of healthy controls. Some dimensions of SAD, notably the presence of child social anxiety symptoms, may manifest frequently throughout the lifespan among individuals with MDD. Furthermore, as shown in Figures 1 and 2, some individuals in both the MDD and control groups exhibited several symptoms of OCD or SAD, although their scores were significantly lower than those of patients with OCD or SAD. These findings support the spectral and dimensional framework, suggesting that OCD or SAD symptoms should be considered from a dimensional and transdiagnostic perspective.
Concerning criterion validity, ROC curve analysis showed that the AUC values for the Korean version OBS-SR and SHY-SR were significantly higher than 0.70 against the reference criterion of the DSM diagnosis by a psychiatrist. This suggests that the OBS-SR and SHY-SR have excellent discrimination ability and diagnostic accuracy for detecting OCD and SAD in clinical settings, respectively. The optimal cut-off points for the OBS-SR and SHY-SR were 50 (sensitivity of 71% and specificity of 94%) and 44 (sensitivity of 86% and specificity of 97%), respectively. In a Spanish study, the optimal cut-off point for OBS-SR was 39 with an AUC of 0.955 and that of SHY-SR was 59. The OBS-SR and SHY-SR could be used as effective tools to support an accurate diagnosis, provided that the appropriate cut-off value is applied, taking into account ethnic and cultural differences.
This study had several limitations. First, the sample size was relatively small, and the number of healthy controls used for the ROC analyses was approximately 30. Therefore, the cutoff scores of the OBS-SR and SHY-SR in this study were preliminary and should be used with caution. Second, the divergent validity of the scales used in this study was not assessed. Future studies should confirm whether these do not correlate strongly with other measures of different constructs. Third, the convergent validity of the OBS-SR and SHY-SR was assessed only in patients with OCD and SAD, respectively. Further convergent validity studies are needed in heterogeneous groups, including those with OCD or SAD, normal controls, and other psychiatric conditions. Finally, differences in the sex distributions and unequal sample sizes among the three groups involved in the OBS-SR and SHY-SR studies were observed, which may have affected the known-group validity results. Notably, most of the results from the known-group validity analyses remained largely unchanged even after controlling for the influence of sex distribution. Nevertheless, future studies tailored to specific sex distributions are required.
In conclusion, the Korean versions of the OBS-SR and SHY-SR can be used to assess OCD and SAD with good reliability and validity and can quantitatively detect differences between individuals afflicted with OCD or SAD and those who do not have these conditions in Korean population. In addition, they are applicable for assessing a broad spectrum of obsessive– compulsive and social anxiety symptoms, respectively, including full-blown disorders and subthreshold or atypical presentations.
Supplementary materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2023.0338.
Means of the domains and total scores, ANOVAs, and significant pairwise comparisons (LSD test)
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Se Joo Kim. Data curation: Jee In Kang, Se Joo Kim. Formal analysis: Se Joo Kim. Investigation: Jee In Kang, Se Joo Kim. Methodology: Jee In Kang, Se Joo Kim. Validation: Se Joo Kim. Writing—original draft: Jee In Kang. Writing—review & editing: Jee In Kang, Se Joo Kim.
Funding Statement
This work was supported by National Research Foundation of Korea (NRF) grants funded by the Korean government (2021M3E5D9025022 and RS-2023-00209077).
Acknowledgements
None