The Impact of Prolonged Duration of Untreated Illness on Clinical Correlates in Chronic Schizophrenia: Exploring the Relationship With Suicide Risk
Article information
Abstract
Objective
Studies on duration of untreated psychosis are common in patients with schizophrenia, but few studies have investigated the relationship between duration of untreated illness (DUI) and suicide, especially in patients with chronic schizophrenia. Therefore, we intended to investigate the relationship between DUI and suicide and clinical correlates in patients with chronic schizophrenia.
Methods
A total of 1,555 Chinese patients with chronic schizophrenia were enrolled in this study. DUI was measured in years, reflecting the prolonged untreated periods observed in this population. Clinical correlates were assessed, including symptoms, cognitive functioning, and body mass index. Suicidal ideation and attempts were also examined. Statistical analyses, including multivariate models, were employed to investigate the associations between DUI and clinical correlates while controlling for potential confounders.
Results
The study revealed a significant proportion (23.3%) of patients with chronic schizophrenia in China received their first treatment after a 4-year delay, with the longest untreated duration reaching 39 years. Patients with longer DUI exhibited more severe negative symptoms, lower immediate memory scores, a higher likelihood of being overweight, and surprisingly, a reduced likelihood of suicidal ideation and attempts. Each additional year of untreated illness was associated with a 3% decrease in the risk of suicidal ideation and attempts.
Conclusion
The findings underscore the prevalence of extended untreated periods in Chinese patients with chronic schizophrenia and highlight the impact of DUI on negative symptoms, cognitive function, and body weight. Intriguingly, a longer DUI was associated with a lower risk of suicidal ideation and attempts.
INTRODUCTION
Schizophrenia, a chronic and severe mental disorder, affects more than 20 million individuals worldwide [1,2]. In China, the prevalence of schizophrenia is 0.6% [3]. This condition is characterized by distortions in cognition, perception, affect, language, sense of self, and behavior [1,4,5]. Among the various forms of this disorder, chronic schizophrenia presents distinctive challenges due to its persistent course and enduring impact on patients’ lives [4,6].
A critical aspect of managing chronic schizophrenia lies in comprehending the duration of untreated illness (DUI), defined as the interval from the first noticeable symptoms to the initiation of antipsychotic treatment [7]. DUI has been linked to a range of outcomes in schizophrenia, encompassing symptom severity, functional impairment, and quality of life [8]. In many cases, schizophrenia treatment yields less favorable results than anticipated, underscoring the significance of early detection and intervention [9]. Studies have demonstrated that the likelihood of recovery from schizophrenia within 6 months is less than 1% [10]. Furthermore, almost half of patients discontinue antipsychotic treatment within 6 months [11,12]. Therefore, to improve the outcome of schizophrenia, it is imperative to identify the factors that influence prognosis and investigate ways to address them. To date, these factors have encompassed treatment appropriateness, schizophrenia severity, and, notably, the issue of DUI [9,12].
Previously, a more prevalent focus has been on the duration of untreated psychosis (DUP) in schizophrenia, defined as the interval from the first noticeable psychotic symptoms, including hallucinatory delusions, to the initiation of antipsychotic treatment [7,13]. However, there are two primary challenges with the DUP. Firstly, the difficulty in identifying psychotic symptoms hampers an accurate calculation of DUP [9]. Patients and caregivers often lack the expertise to recognize mental illness symptoms precisely [14]. In addition, hallucinations and delusions manifest in diverse and multifaceted ways [15], making the DUP challenging to estimate. Secondly, the 6-month course of schizophrenia encompasses any combination of active, prodromal, and residual symptoms, according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [16]. However, DUP predominantly revolves around hallucinations and delusions and excludes any prodromal phase symptoms of schizophrenia [17]. Therefore, it may be more precise to ascertain schizophrenia’s duration through DUI rather than DUP [18].
Suicide in schizophrenia has been extensively researched [19-21]. A study in the United States, comprising 668,836 patients with schizophrenia, found a total suicide rate of 74.00 per 100,000 person-years, 4.5 times higher than the rate in the general population [19]. In addition, the suicide rate for schizophrenia can be as high as 13% [20]. It is noteworthy that depression and insomnia, when present in individuals grappling with schizophrenia, exacerbate the risk of suicide [20,21], possibly due to stigma effects [22], particularly social discrimination [23]. However, the prior research on the association between DUI and suicide in schizophrenia has yielded inconsistent findings. Some studies suggest that a longer DUI is associated with an increased risk of suicide [24-26], while others fail to discern any such correlation [27]. For example, a study from rural China found a positive association between DUP and suicide; however, this relationship dissipated after a 14-year follow-up period [27]. In addition, one study illuminated that among individuals with first-episode schizophrenia, a history of suicide attempts was inversely related to the DUP [28]. These conflicting findings highlight the imperative need for further exploration in this domain.
Several factors underscore the urgency of investigating the etiology and repercussions of DUI, primarily due to its modifiable nature [29]. Reduction of DUI holds the potential to exert a positive influence on the prognosis and long-term trajectory of the pertinent psychiatric condition [30]. However, there is still a lack of research on the relationship between DUI and suicide in schizophrenia. It is important to explore this issue, as it may serve two pivotal purposes: 1) augmenting the understanding of the relationship between DUI and suicidality alongside clinical features, thereby prompting vigilant monitoring by psychiatrists, and 2) motivating individuals who have schizophrenia to seek timely treatment. Therefore, the primary objective of this study was to investigate the relationship between DUI and suicide while concurrently exploring its clinical correlates within a large sample of patients with chronic schizophrenia.
METHODS
Participants
The study adhered to the principles outlined in the Declaration of Helsinki and received approval from the Institutional Review Board of the Institute of Psychology, Chinese Academy of Sciences (approval number: H18031). Prior to their participation, each patient received a comprehensive explanation of the research, and their informed written consent was obtained.
A total of 1,555 patients diagnosed with chronic schizophrenia were recruited from 17 psychiatric hospitals across China between October 2018 and January 2020. Inclusion criteria consisted of 1) age within the range of 18–70 years and Han nationality, 2) confirmation of a schizophrenia diagnosis, established by two experienced psychiatrists utilizing the Structured Clinical Interview (SCID) for DSM-IV, 3) maintenance on a stable dose of antipsychotic medications for at least 6 months before enrollment, 4) ability to actively participate in psychopathological assessments and furnish written informed consent.
Exclusion criteria comprised participants who presented with 1) comorbid severe physical and neurological conditions or mental retardation, 2) pregnancy or breastfeeding, 3) significant fluctuations in psychotic symptoms during the preceding 2 weeks.
Notably, in most Chinese psychiatric hospitals, the male-to-female ratio among inpatients with schizophrenia approximates 2:1, attributable to a complex interplay of societal, familial, and individual factors. This study maintained the male-to-female ratio at two to one, aligning with this representative pattern of chronic schizophrenia inpatients in China. defined as the interval from the first noticeable symptoms to the initiation of antipsychotic treatment.
DUI
The DUI (years) was defined as the interval between the patient’s first noticeable symptoms and the initiation of the first pharmacological treatment [18,31]. We ascertained first noticeable symptoms such as unusual fears, hallucinations, delusions, and social withdrawal by interviewing the patient and primary caregiver. In addition, we confirmed the course of the patient’s illness by reviewing case histories, such as the records of the initial consultation [32]. In this investigation, patients were categorized into three groups based on the 25% and 75% quartile of DUI: <1 year, 1–3 years, and ≥4 years.
Clinical measurements
Demographic and clinical data, including sex, age, education, and medical history encompassing diabetes, hypertension, and cardiovascular diseases, were collected via self-administered questionnaires. Height and weight measurements were undertaken by nursing personnel, and the body mass index (BMI) was computed by dividing the weight in kilograms by the square of height in meters. Following the Chinese BMI classification [33], underweight was defined as <18.5 kg/m2, normal weight as 18.5 to <24 kg/m2, overweight as 24 to <28 kg/m2, and obesity as ≥28 kg/m2.
The assessment of suicidal ideation and suicide risk was executed using the Beck Scale for Suicide Ideation (SSI) [34], and suicidal events were categorized and assessed with the Colombian Classification Algorithm for Suicide Assessment (C-CASA) [35]. According to C-CASA, suicide was defined as having a genuine intention to commit suicidal behavior but without success [36]. Subjects who had previously attempted suicide at any point were categorized as suicide attempters. Details concerning the exact date, method, and frequency of suicide attempts were meticulously recorded.
The severity of subjective insomnia in the past week was evaluated utilizing the Insomnia Severity Index (ISI) [37]. The ISI comprises 7 items, each scored from 0 to 4, with higher scores indicating more severe insomnia. The reliability and validity of the Chinese version of ISI have been established [38].
Two trained psychiatrists employed Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/P) for participant screening. Basic information, demographic factors, and medical conditions were gathered through a self-designed survey supplemented by data from medical records. Schizophrenia symptomatology was assessed using the Positive and Negative Syndrome Scale (PANSS) [39], with all study personnel undergoing PANSS-related training, and the inter-rater reliability coefficient (ICC) among observers exceeding the critical threshold of 0.8 [40].
Cognitive functioning was assessed individually using the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS, Form A) [41]. Twelve subtests were administered to derive five index scores and a total RBANS score. The five indices encompassed immediate memory, attention, language, visuospatial/constructional, and delayed memory. Previously established by our research group, the Chinese-translated and validated version of RBANS was exclusively utilized [42]. Before the commencement of the study, two researchers received training in RBANS administration.
Between 6 and 8 Am, fasting blood samples were collected by nursing staff, and analysis was initiated before 11 Am on the same day. Plasma samples were examined for biochemical markers, encompassing low-density lipoprotein cholesterol, total cholesterol, triglycerides, blood glucose, and high-density lipoprotein cholesterol.
Statistical analysis
All continuous variables exhibited non-normal distributions, even following log transformation, via the Shapiro–Wilk method. Continuous variables were compared using the Mann–Whitney U test. In contrast, categorical variables were assessed with the chi-square test to analyze demographic characteristics concerning DUI and to investigate unadjusted associations between various clinical correlates and DUI.
Subsequently, multivariate linear models were employed for continuous variables, multivariate logistic models for binary variables, and multinomial logistic models for categorical variables. These models aimed to explore the relationships between DUI and clinically significant correlates that displayed significance at p<0.2 in bivariate analyses [43], adjusting for age, sex, education, marital status, and living arrangement. The multivariate model also estimated the association between clinical correlates and continuous DUI in years.
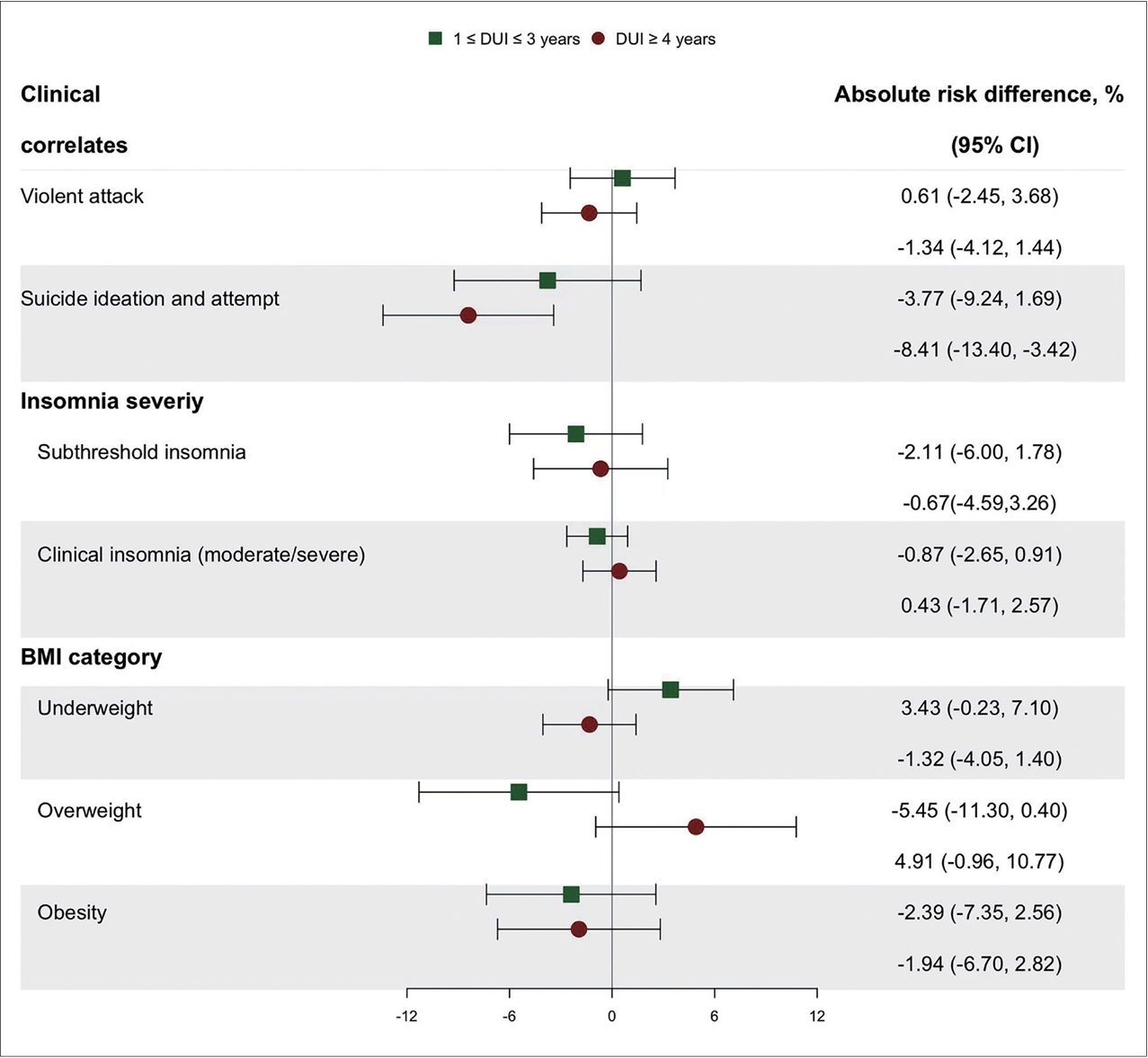
The absolute risk difference was computed for binary or categorical variables to enhance clinical interpretability. For instance, taking the variable of violent attacks as an example, we subtracted the conditional predicted probability of experiencing violent attacks with DUI set to a specific value from that with DUI set equal to the reference level. At the same time, all covariates were held at their reference levels [44]. All statistical analyses were conducted using Stata version 17.0 (StataCorp LLC., College Station, TX, USA).
RESULTS
Among the 1,555 participants, 884 (56.8%) initiated their first treatment within 1 year of symptom onset, while 363 (23.3%) did so 4 years or more after onset (Table 1). The mean DUI for chronic schizophrenia was 3.12±6.23 years, from 0 years (less than 1 month) to 39 years. Notably, older participants were less inclined to seek timely treatment (p<0.001), whereas those living with family members were more likely to seek timely treatment (p<0.05).
In bivariate analyses (Table 2), individuals with longer periods of untreated illness exhibited higher scores in the negative PANSS subscale and a higher likelihood of being overweight (all p<0.05). Strikingly, those with longer untreated periods were less likely to experience suicidal ideation and attempts (p=0.005). Of particular interest, in terms of cognitive function, individuals with untreated periods lasting 1–3 years demonstrated higher total RBANS and immediate memory scores (p<0.05). Even after Bonferroni correction, the significance persisted for immediate memory scores (p Bonferroni<0.05/5=0.01).
There was no significant difference in the likelihood of having all investigated clinical correlates (except for suicidal ideation and attempts) among participants who had not received treatment for ≥4 years compared with those treated within 1 year, with an odds ratio of 0.61 (95% CI 0.44–0.83) for suicidal ideation and attempts (Table 3). Furthermore, no significant differences were identified in the likelihood of having all assessed clinical correlates between subjects treated within 1 year and those treated beyond 1 year. The results derived from the multivariate model unveiled that for each additional year of untreated time, patients were 3% less likely to experience suicidal ideation and attempts (95% CI 0.94–0.99).
As shown in Figure 1, only the risk of suicidal ideation and attempts was decreased for those who had been untreated for the longest period, with an absolute risk difference of 8.41% (95% CI 3.42–13.40).
DISCUSSION
This study represents the first large-scale investigation of the relationship between DUI and suicide in chronic schizophrenia in China. Our main findings are: 1) a significant proportion (23.3%) of Chinese patients with chronic schizophrenia received their first treatment 4 years after onset. The longest untreated period in this study was 39 years, 2) participants who had been untreated for longer had higher negative PANSS subscale scores, lower immediate memory scores, a higher likelihood of being overweight, and a lower likelihood of suicidal ideation and suicide attempts, 3) patients with each additional year of untreated time were 3% less likely to have suicidal ideation and attempts.
Long DUI phenomenon of schizophrenia in China
Our study highlights a significant proportion (23.3%) of Chinese patients with chronic schizophrenia who did not receive their initial treatment until 4 years after the onset of symptoms, consistent with previous studies. Undeniably, schizophrenia in China has a long, untreated duration [45,46]. The lack of timely treatment for schizophrenia patients is a complex problem in China [27]. Research from the National Institutes of Health-funded Michael Phillips found many untreated schizophrenia patients over 60 in China [47]; in rural China, untreated psychosis is even as high as 22.9 years [45]. This prolonged DUI underscores the delayed treatment and management of schizophrenia patients in China, ultimately predicting an unfavorable long-term prognosis [48].
Several factors contribute to the delayed treatment of schizophrenia patients in China. Firstly, economic disparities play a pivotal role [49], with underprivileged regions exhibiting lower rates of hospitalization and treatment for schizophrenia patients, resulting in elevated suicide rates and premature mortality [50]. Secondly, stigma associated with mental illness can deter patients from seeking timely treatment [51,52], while social isolation of individuals with mental disorders can hinder access to practical assistance [53]. Thirdly, the scarcity of mental health services in China has historically prevented individuals with mental illnesses from receiving immediate treatment [54,55], given the lack of mental health hospitals and support facilities [54,56]. Finally, the difficulty of early identification of mental illness plays a vital role in long DUI [57,58]. For instance, the prodromal symptoms of schizophrenia are difficult to identify [57], further perpetuating the untreated period.
DUI and clinical correlates in chronic schizophrenia
Our main finding is that the longer the DUI, the worse the clinical characteristics of schizophrenic patients, including higher PANSS negative scale scores, lower immediate memory scores, and a higher likelihood of being overweight. These results align with previous research indicating that an extended duration of schizophrenia is correlated with more severe negative symptoms [46]. Negative symptoms encompass emotional apathy, blunted affect, and reduced volitional activity [4,59,60]. Contributing to profound social and occupational impairment, suicide risk, and mental disability [20]. Hence, expediting the reduction of DUI is paramount for enhancing social functioning.
Cognitive impairment in schizophrenia has garnered increasing attention [4,61], with prior research identifying impairments in processing speed, verbal memory, and working memory among individuals with schizophrenia [61]. In addition, impairment of cognitive functioning will lead to psychiatric disability and severe social burden [61-63]. Our study reveals that a longer DUI is linked to poorer immediate memory in schizophrenia, aligning with previous findings [61]. For instance, one study found that a longer DUP independently predicted cognitive decline [64]. Furthermore, prior research has reported a negative association between DUP in schizophrenia and memory function [65,66]. These results underscore the importance of reducing the untreated period for schizophrenia patients concerning cognitive functioning [67]. However, some studies have indicated a weak [68] or no relationship between DUP in schizophrenia and cognitive function [69,70], suggesting that the link between DUI/DUP and cognitive function warrants further exploration.
The higher prevalence of overweight in schizophrenia is confirmed by previous studies [71,72]. Individuals with severe mental illness are two to three times more likely to be overweight or obese than the general population, resulting in substantial morbidity and premature mortality [71]. A possible reason for the relationship between the untreated period and body weight is mental illness’s toxic effects [73]. Previous studies have found toxic effects of mental illness, including glutamate excitotoxicity and elevated dopamine levels [74]. Secondly, symptoms of the prodromal phase of schizophrenia include reduced social activity, emotional withdrawal, and lack of intentional activity, leading to weight gain [57]. Thus, the longer the period of untreated illness, the more likely the person with schizophrenia will have an abnormal BMI and be overweight.
DUI and suicide in chronic schizophrenia
Our study’s key finding is that it contributes to understanding the relationship between DUI and suicide ideation and attempts in patients with chronic schizophrenia. Notably, a longer DUI was associated with lower suicide ideation and attempts. This finding appears counterintuitive, as one might expect that a longer period of untreated illness would lead to worse outcomes [46], especially suicide [27,29].
One possible explanation for our findings is that patients with a longer DUI may develop coping mechanisms over time that reduce their suicide risk. Long-term untreated patients with schizophrenia may develop impaired social cognition [47], potentially reducing their perception of stigma effects, shame, and suicide risk [75]. In addition, emotional withdrawal was found to be negatively associated with suicide [76]. Emotional withdrawal is typical of negative symptoms, and a positive correlation between DUI and negative symptoms in schizophrenia may contribute to the decrease in suicide risk. These hypotheses warrant further investigation.
Our study has several limitations. Firstly, the study’s focus on a Chinese population may limit the generalizability of the results to other cultural or ethnic groups. Secondly, the measurement of suicide attempts based on a self-report scale may not capture the full complexity of this behavior, and underreporting due to stigma or fear could be a concern. Thirdly, the cross-sectional design prevents the establishment of causal relationships between DUI and suicide risk, and there may be unmeasured confounding factors. Fourthly, the study’s reliance on the RBANS to measure cognitive functioning may not encompass all aspects of cognitive impairment in schizophrenia. Fifthly, we quantify the DUI in terms of years due to the prolonged untreated periods commonly observed among patients with chronic schizophrenia in China. Nevertheless, it’s worth noting that previous studies have typically measured DUI or DUP monthly, a practice that could enhance result consistency. In addition, defining DUI’s in terms of years has potential limitations. For example, DUI in terms of years does not provide precise time to respond to the details of changes in the temporal dimension of psychotic symptoms or suicidal problems. Therefore, future studies analyzing the relationship between DUI and suicide in schizophrenic patients in more refined time units are urgently needed. Sixthly, the long DUI could reflect characteristics of psychosis itself rather than a delay in treatment [8,17], which warrants further investigation. Seventhly, successful suicides can lead to exclusion from the study and therefore introduce bias because there’s a possibility that patients with longer treatment durations might be underrepresented due to successful suicide attempts. Therefore, the use of our findings requires caution. Finally, our findings are based on a Chinese population and may not be generalizable to other ethnic or cultural groups. Future research should aim to replicate our results in different people and settings and explore the mechanisms underlying the observed relationship between DUI and suicide risk. Such studies could provide valuable insights into how to support patients with chronic schizophrenia best and reduce their risk of suicide.
In conclusion, many Chinese chronic schizophrenia is not treated promptly. Long DUI in schizophrenia is associated with severe negative symptoms, low cognitive function, and a high risk of being overweight. In addition, we found that a longer DUI was associated with lower suicide ideation and attempts, which is contrary to what one might expect. Our findings underscore the need for further research into the relationship between DUI and suicide risk in schizophrenia and the factors that contribute to long DUI. Such research can inform strategies to improve the early detection and intervention of schizophrenia, ultimately leading to better outcomes for individuals with this chronic and severe mental disorder.
Notes
Availability of Data and Material
The data supporting this study’s findings are available on request from the corresponding author.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Guoshuai Luo, Xiangyang Zhang. Data curation: Ke Zhang, Chenxi Wang, Lei Gou. Formal analysis: Yaxi Li. Funding acquisition: Xiangyang Zhang. Investigation: Xiangyang Zhang. Methodology: Yaxi Li, Guoshuai Luo. Project administration: Guoshuai Luo, Xiangyang Zhang. Resources: Guoshuai Luo, Cui Li. Software: Yaxi Li. Supervision: Cui Li. Validation: Yaxi Li. Visualization: Yaxi Li. Writing—original draft: Ke Zhang, Chenxi Wang, Lei Gou. Writing—review & editing: Guoshuai Luo.
Funding Statement
This work was supported by the National Natural Science Foundation of China [81973759]. This source had no further role in this study design, in the data collection and analysis, in the writing of the report, and in the decision to submit the paper for publication. The authors acknowledged the nurses and psychiatrists that provided professional support when conducting data collection.
Acknowledgements
None