Factors Associated with Insomnia among the Elderly in a Korean Rural Community
Article information
Abstract
Objective
Sleep disturbance is common in the elderly, which is result from multi-factorial causes encompassing socio-demographic, behavioral, and clinical factors. We aimed to identify factors associated with insomnia among the elderly in a rural community in South Korea, a country with a rapidly growing aged population.
Methods
This cross-sectional study used the data from the second wave of the Korean Social life, Health and Ageing Project, which is a cohort study of individuals living in a typical rural community in South Korea. Socio-demographic, behavioral, and clinical characteristics were obtained through face-to-face interviews. Various factors suspected to be associated with insomnia were compared between elderly participants with and without insomnia, and multiple logistic regression analyses were conducted to identify independent risk factors for insomnia.
Results
We found that 32.4% of 509 participants (72.8±7.7 years old) had insomnia. Female sex [odds ratio (OR)=2.19], low education level (OR=2.44), current smoking (OR=2.26), number of chronic diseases (OR=2.21 for 2–3 chronic diseases; OR=2.06 for 4 or more chronic diseases), and depression (OR=2.53) were independently associated with insomnia.
Conclusion
We found that sex, education, chronic disease, and depression independently increase the risk of insomnia of the elderly in a Korean rural community. To overcome the elderly's insomnia, interventions should target modifiable factors such as depression. To promote active aging, longitudinal studies of factors associated with insomnia among the elderly should be performed in different regions and communities.
INTRODUCTION
According to the World Health Organization, active aging is the process of optimizing opportunities for health, participation, and security as people age.1 One of the most important determinants of active aging is health, which includes both physical and mental health. The concept of active aging is getting attention from researchers and policy makers, who are interested in understanding modifiable factors, such as sleep, that can improve and promote the health of aging populations.
With the rapid growth of the aging population in South Korea,2 sleep problems are receiving more attention. The number of South Korean people who underwent treatment for sleep disorders was increased by 16% from 2012 to 2014.3 People over 60 years of age made up the largest portion of this treated population (45%), and their growth rate (25%) was the highest in all age group. The most commonly diagnosed sleep disorder was insomnia (67%). Despite the growing interest in sleep among older adults in Korea, specific data and strategies for preventing or treating sleep disorders are lacking. Although sleep duration decreases with age, and insomnia is common in older adults, insufficient or unsatisfactory sleep is not a normal part of aging.4
Insomnia is not only a cause of heterogeneous health conditions but also an outcome of many different factors.5 Persistent insomnia affects both physical and mental health.46 Insomnia increases risks of mortality,7 falling-down,8 depression,6 and decreases a quality of life9 in elderly individuals. Moreover, treating insomnia can lower the risk of medical disease.10 Insomnia is influenced by socio-demographic characteristics, physical and mental health status, and other sleep-related symptoms.45 In Korea, there are several studies about sleep disorders in older adults;111213141517 they focused mostly on the urban elderly. Sleep patterns, chronotype, and light exposure are different between the urban and rural population.18 In addition, due to inequalities in socio-economic status and accessibility to medical services between rural and urban areas,19 it is also important to investigate contributing factors to insomnia amongthe rural elderly.
Considering the need for health-related prevention policies for aged population, it is necessary to carry out a rural community-based study of insomnia including a diverse array of sleep-related factors. Therefore, we aimed to identify factors associated with insomnia among older adults in a Korean rural community to form a basis for promoting good sleep active aging of elderly in dividuals.
METHODS
Study population
This study used data from the Korean Social life, Health and Ageing Project (KSHAP), which is an ongoing community-based cohort study. The target population of the KSHAP is people aged 60 years or older living within one township in Korea (“Y”-myeon, Ganghwa-gun, Incheon, Korea). This township is a typical rural area in Korea, where farming is the main industry. The data collection procedure has been described in detail elsewhere.20 During the second wave of the KSHAP (September 2012–August 2013), 509 participants completed a questionnaire survey. To examine insomnia and its correlates, we used cross-sectional data from this second wave, which included more number of sleep-related variables than ones of the other waves of the KSHAP. All participants provided written informed consent. The Institutional Review Board of Yonsei University approved this study.
Measurement
Through the face-to-face interviews, we obtained information on socio-demographic, behavioral, and clinical variables. Considering that participants lived in a rural area, we also asked about difficulty in accessing medical services during the last year. The questionnaire included items about difficulty with sleep initiation or maintenance, average sleep duration during the last year, and presence of snoring. We considered insomnia as being present if the respondent reported difficulty in sleep initiation or maintenance. If the answer to the question “Have you heard that you snore?” was “yes”, then the following question was asked to identify snoring with apnea: “Have you heard from your bed partner that you stop breathing with snoring?” Because the first screening question for snoring was too inclusive, we used snoring with apnea as a variable instead of the presence of snoring.
We also collected participant histories of the following diseases: hypertension, diabetes mellitus, hyperlipidemia, arthritis, osteoporosis, cancer, stroke, myocardial infarction (or angina), tuberculosis, asthma, hepatitis B, and urination disorder (i.e., urinary incontinence for both sex and benign prostate hyperplasia for males). Interference by pain was measured with the following question from the SF-12 Health Survey version 221: “How much did pain interfere with your normal work?” We considered the answer of “not at all” and “a little bit” as negative answers and “moderately”, “quite a bit”, and “extremely” as positive answers. Depression was defined as a score of ≥10 on the Geriatric Depression Scale-Short Form (15 items).22 Cognitive impairment was defined as a score of ≤23 on the Mini-Mental State Examination.23 Subjective degree of physical activity was classified into two categories of the activity level: none to low versus moderate to high. We regarded moderate activity as in regular, even if light, exercise.
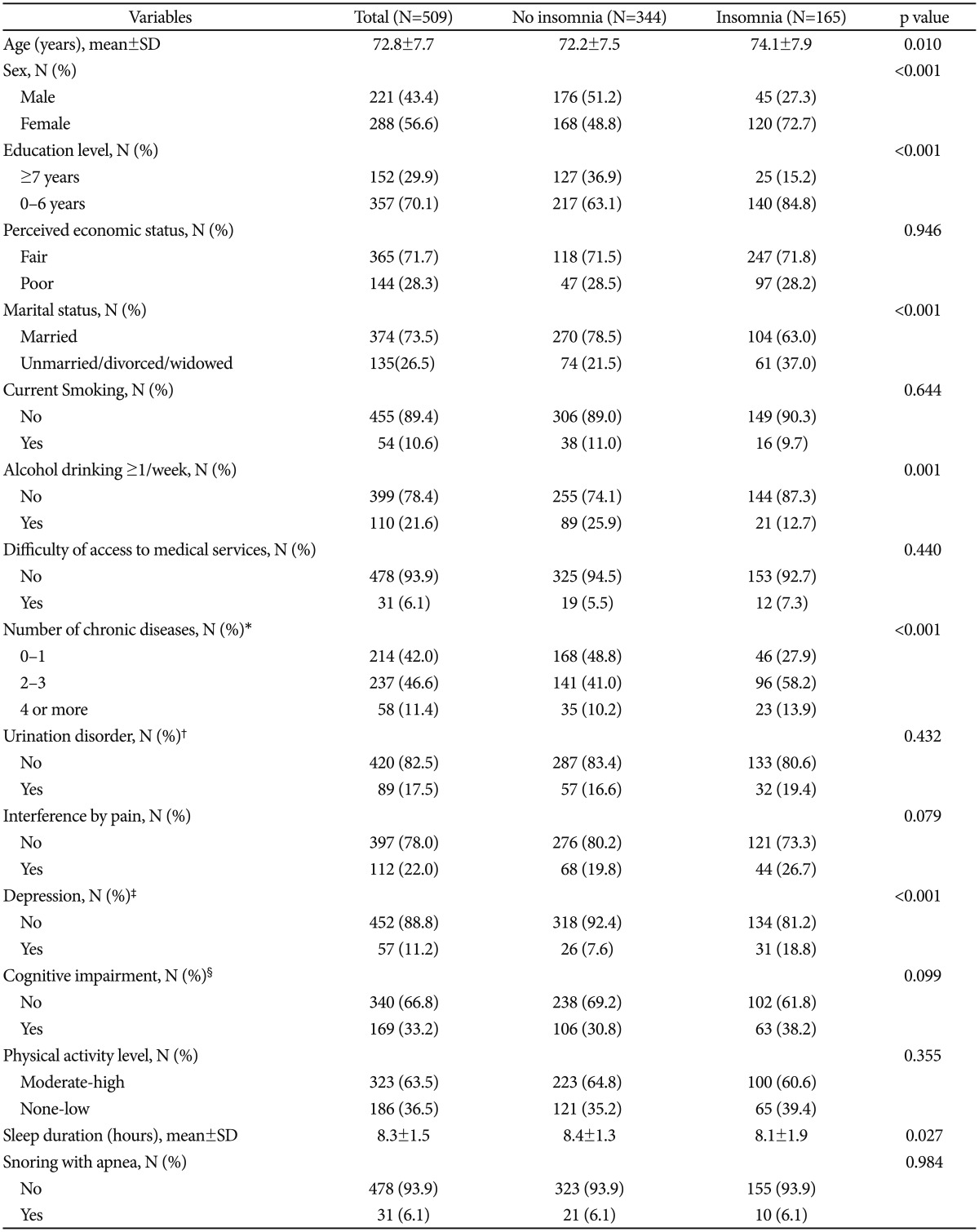
Statistical analyses
The following suspected associated factors for insomnia were compared between participants with and without insomnia using independent t-tests and chi-square tests when appropriate: age, sex, education level, perceived economic status, marital status, smoking status, alcohol intake, difficulty of access to medical services, number of chronic diseases, presence of urination disorder, interference by pain, presence of depression and cognitive impairment, and physical activity level. Sleep duration and snoring with apnea were also compared between groups. There were no missing data for any of the variables.
To examine which factors are associated with insomnia, we performed two regression analyses: first, using all variables except sleep duration and snoring with apnea (model 1), and second, using all variables including sleep duration and snoring with apnea (model 2). Even if not significantly different in the descriptive analyses, all of the above-mentioned variables were entered into the multiple logistic regression models for insomnia because we assumed that each variable could affect the other variables. Because marked sex differences were found in previous studies of our KSHAP sample,2425262728 we evaluated interaction effects between sex and all other variables by adding interaction terms into the regression model to maximize the number of independent variables.
Data analyses were conducted using SPSS for Windows version 20 (SPSS Inc., Chicago, IL, USA), and statistical significance was set at p<0.05.
RESULTS
Of the 509 participants, 32.4% (n=165) had insomnia. Table 1 shows the socio-demographic, behavioral, and clinical characteristics of the participants. Compared with participants without insomnia, those with insomnia were older and had shorter sleep durations. Elderly participants with insomnia were more likely to be female, less educated, less likely to be married, and less frequent (<1/week) alcohol drinkers. Participants with insomnia also had a greater number of chronic diseases and higher prevalence of depression.
To identify factors associated with insomnia, all variables were examined by multiple logistic regression analyses (Table 2). In model 1, which excluded sleep duration and snoring with apnea, the following variables were positively associated with insomnia: female sex, low education level, current smoking, two or more chronic diseases, and depression. In model 2, which controlled for sleep duration and snoring with apnea, all of these factors, except for smoking, remained significantly associated with insomnia. Shorter sleep duration was also associated with insomnia in model 2.
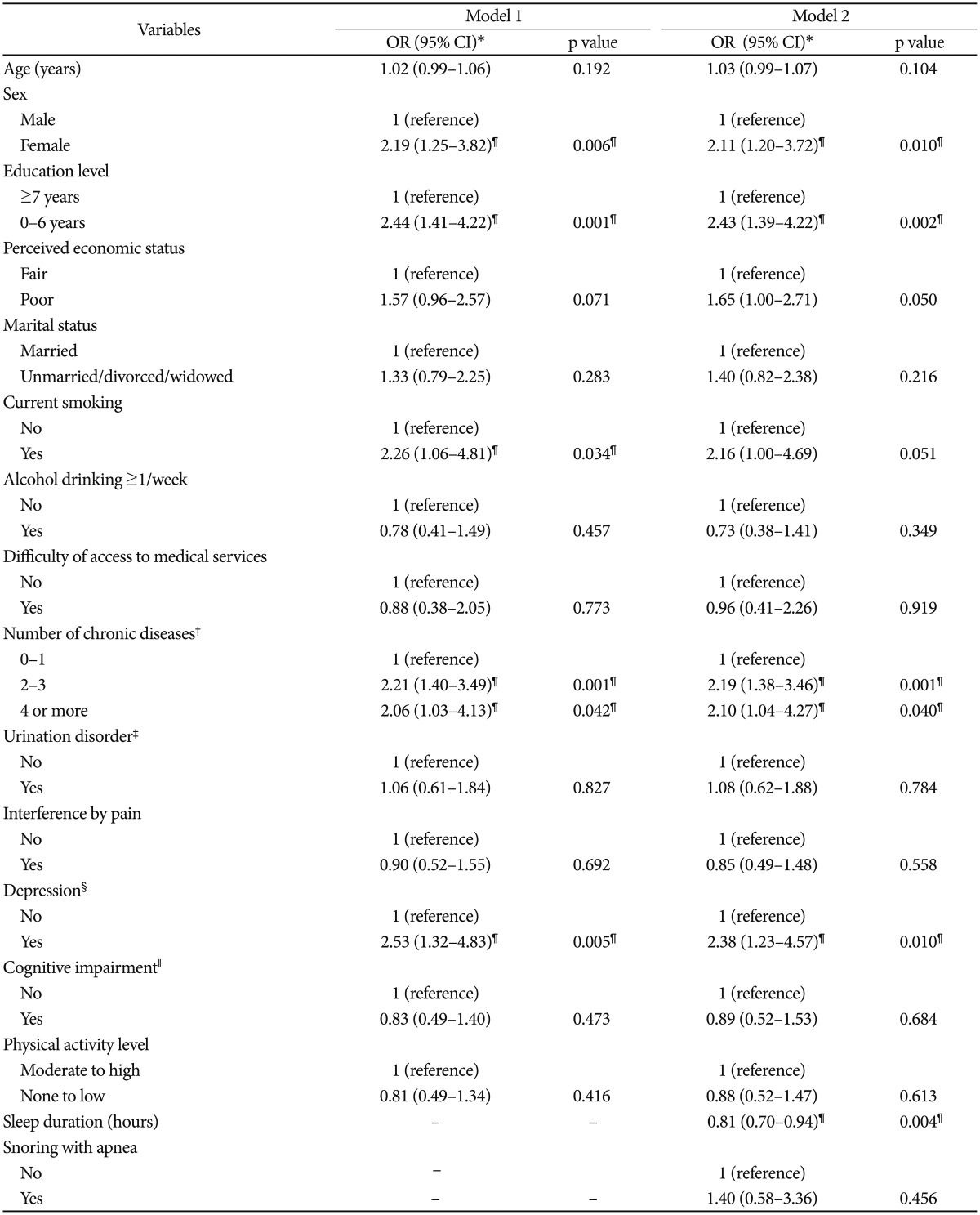
Multiple logistic regression models of factors associated with insomnia among the Korean rural elderly
We found no significant interactions between sex and any other variables (data not shown).
DISCUSSION
We investigated factors associated with insomnia among Korean rural older adults. In this KSHAP community sample, we found that socio-demographic (sex, education level), behavioral (smoking), and clinical (number of chronic diseases, depression, and sleep duration) characteristics were associated with insomnia. This study is valuable in terms of exploring multi-domain correlates of insomnia, including sleep-related factors, among rural community-dwelling older adults in Korea.
Aging perse is known to affect sleep architecture. Older adults often have difficulty of falling asleep or experience mid-sleep awakening, and their sleep efficiencies become reduced compared with those of younger adults.29 For this reason, the prevalence and severity of insomnia increase with age.30 Likewise, we found that participants in the insomnia group had a higher mean age than participants in the no insomnia group. However, the association between age and insomnia disappeared after adjusting for other socio-demographic, behavioral, and clinical factors in our multivariate analyses. This result is in line with an earlier epidemiological study31 that showed no association between age and sleep complaints after adjusting for the health status of elderly individuals. These observations suggest that the effect of age on insomnia could be mediated by age-related changes in sleep architecture and other aging-related factors such as chronic illness or depression.
Depression has repeatedly been found to be associated with insomnia in older adults.532 Depression and insomnia are independent risk factors for each other.3334 The diagnosis and treatment of depression are essential for individuals with insomnia who do not recognize their depressive symptoms. Among the 57 participants considered to have depression in our sample, only five were diagnosed with depression by a doctor. As the prevalence of depression among the Korean elderly is estimated to be 30–40%,2235 the prevalence of depression in this study could be underestimated. Although the number of medical services in rural areas is far less than that in the urban areas,36 this potential under-diagnosis of depression in our cohort does not seem be a result of “difficulty” in access to medical services, as over 90% of participants did not report difficulty in accessing medical services. Because the main objective of the second wave of the KSHAP project was not to perform psychiatric/behavioral evaluations, the plan for the next wave of the KSHAP study should include psychiatric interviews and assessment of medical service utilization, so that we can better understand the relationship between insomnia and depression.
Female sex and low educational level were also associated with insomnia, consistent with previous studies.532 Female sex and low educational level are also risk factors for poor health and chronic illness.37 According to Cutler and Lleras-Muney,38 education is associated with general health of population via income, access to healthcare, problem solving skills, social network, and relative social position. Among all of the clinical factors, we found that only the number of chronic diseases was a significant correlate of insomnia. By contrast, pain was the predominant associative factor of insomnia in other Asian studies.3940 This difference between studies might be due to the fact that we examined interference by pain instead of the mere presence of pain. Based on these findings, we plan to conduct a follow-up study to investigate the effect of targeted intervention programs on insomnia among high-risk groups.
There were some limitations to our study. First, all examined variables were based on subjective reports by participants. Second, this study employed a cross-sectional design, so we were unable to determine causal relationships. Third, medication use was not included in our analyses. Fourth, we did not include anxiety symptoms that could be additional psychological factors influencing insomnia. However, a strength of this study is that we collected a complete dataset (i.e., no missing data) using well-trained interviewers. Moreover, this study reflects a real community situation by investigating multiple factors affecting the health of elderly individuals.
In conclusion, we found that sex, education, chronic disease, and depression independently increase the risk of insomnia among older adults in a Korean rural community. These findings suggest the need to manage insomnia and its correlates in rural older adults by considering socio-demographic, behavioral, and clinical characteristics. It will also be necessary to perform proper interventions targeting underdiagnosed and under treated modifiable factors such as depression. Our results can be useful for establishing prevention policies for insomnia among aged populations.
Acknowledgments
This study was supported by grants from the National Research Foundation of Korea funded by the Korean Government (NRF-2014S1A3A204496) and the Korean Mental Health Technology R&D Project, Ministry of Health & Welfare (HM15C0995), Republic of Korea.