Development of a Biomarker-Based Diagnostic Algorithm for Posttraumatic Syndrome after Physical Injury: Design of the BioPTS Study
Article information
Abstract
Severe physical injury is a leading cause of posttraumatic syndrome (PTS). This is to develop a biomarker-based diagnostic algorithm for posttraumatic syndrome (BioPTS) study. This is a 2-year longitudinal cohort study assessing patients who were hospitalized beginning in 2015 at Chonnam National University Hospital in Gwangju, Korea, after experiencing severe physical injuries. Baseline evaluations were made during the acute phase (within 1 month) of the physical injury and included extensive information on sociodemographic and clinical variables as well as a list of biomarkers. All participants will be followed up for 2 years, and the diagnostic and predictive validities of various biomarkers for PTS will be estimated. The BioPTS study will develop the most accurate models for the diagnosis and prediction of PTS, and will contribute to existing research regarding the complex relationships between severe physical injury and psychological issues.
INTRODUCTION
Psychiatric issues following the experience of a severe physical injury
Traumatic physical injury affects millions of people each year; it is estimated that these types of injuries will be responsible for 12% of the global burden of disease by 2020.1 Severe physical injury is also a leading cause of posttraumatic syndrome (PTS), which is associated with depression, anxiety disorders, and particularly, posttraumatic stress disorder (PTSD).234 Moreover, it is suggested that comprehensive interventions are crucial to address potential mental health issues in patients immediately following a physical injury.
Previous studies of PTS after severe physical injury
Previous studies on the epidemiology of PTS after a severe physical injury are summarized in online Supplementary Table 1. A majority of these studies focused on PTSD, several assessed depression and anxiety, and although most of these studies assessed survivors of traumatic injury, several evaluated individuals involved in a natural disaster or terror attack. The prevalence rates for PTS range from 10 to 30%,256 but many studies have examined the important roles played by psychosocial risk factors, such as social support and an optimistic personality,78 and the impact of physical injury on long-term psychological problems.91011 Previous studies on biomarkers associated with PTS are summarized in online Supplementary Table 2. A majority of these studies focused on PTSD, and the commonly evaluated biomarkers include various genetic, epigenetic, endocrine, and neurotransmitter systems.81213 These biomarkers were assessed separately or partially rather than comprehensively.
Limitations of previous studies investigating PTS
Although a considerable amount of findings have been published, a number of unanswered questions remain. First, most studies have primarily focused on PTSD, and depression and anxiety, which frequently occur after physical injuries, tend to be overlooked.2 Second, PTS symptoms manifesting within 1 month of the trauma are largely ignored because PTSD can only be diagnosed 1 month after the trauma. This may be due to the fact that the physical state is the primary concern during the acute phase.11
Third, the recent publication of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) increased the number of possible PTSD symptoms from 17 to 20.14 Additionally, the DSM-5 states that a diagnosis of acute stress disorder (ASD) requires the display of at least three of the five dissociative symptoms and nine symptoms from any of the five categories of intrusion, negative mood, dissociation, avoidance, and arousal after traumatic events. These changes have had an inevitable effect on the how previous PTSD and ASD studies are understood. Finally, biomarkers play an essential role in the prediction and early diagnosis of a number of diseases,15 but relatively few studies have investigated biomarkers for predicting and diagnosing PTS.161718192021
Biomarker-based diagnostic algorithm for PTS study
To overcome the limitations of previous studies, the present study was designed to develop a biomarker-based diagnostic algorithm for PTS after physical injury, known as the biomarker-based diagnostic algorithm for PTS (BioPTS) study. All possible PTS symptoms, including depression, anxiety, and PTSD, will be evaluated from the acute phase (within 1 month) to the chronic phase (up to 2 year) of the physical injury based on the diagnostic criteria of the DSM-5. Additionally, a list of biomarkers will be examined, and their diagnostic and predictive validities for PTS will be estimated. Subsequently, the most accurate models for the diagnosis and prediction of PTS will be used to develop a biomarker-based diagnostic algorithm. The present article presents the basic design and methods of the BioPTS study.
METHODS
Study outline and recruitment
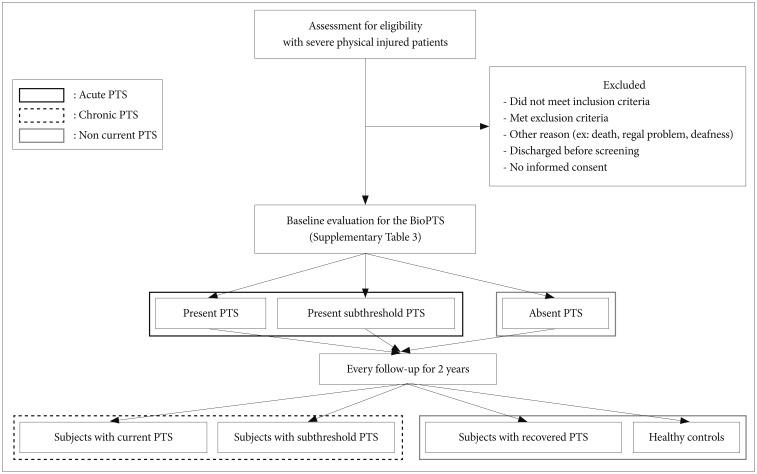
The outline of the BioPTS study is depicted in Figure 1. Participants were consecutively recruited from among patients who were recently hospitalized for a severe physical injury beginning in 2015 at the Department of Trauma Center of Chonnam National University Hospital in Gwangju, Korea. Injury severity was evaluated using the Injury Severity Score (ISS) and the Glasgow Coma Scale (GCS).2223 Patients who met the eligibility criteria and agreed to participate in the study underwent psychiatric assessments at 1, 3, 6, 12, and 24 months after the physical trauma. The sample was set up to include a range of psychopathologies: individuals with no symptoms or disorders (healthy controls), individuals recovering from illness (non-current PTS), and individuals with symptoms or a disorder (current PTS or current subthreshold PTS). The MINI International Neuropsychiatric Interview (MINI) and Clinician-administered PTSD Scale-5 (CAPS-5) were used to diagnose depression, anxiety disorders, and PTSD.2425 The baseline evaluation was conducted in a hospital setting, and after discharge, each subsequent assessment to determine the extent of PTS was conducted via telephone.
Study subjects
The inclusion criteria for the present study consisted of the following: 1) hospital admission more than 24 hours after a severe physical injury (ISS≥9), 2) over 18 years of age, and 3) a native Korean speaker. To maintain a representative sample, the following exclusion criteria were applied: 1) moderate or severe brain injury (GCS<10); 2) primary clinical diagnosis of a psychiatric disorder not associated with PTS that could affect the course of PTS or a diagnosis of a current psychotic disorder, bipolar disorder, or a history of suicide attempts; and 3) the presence of significant preexisting cognitive impairments such as organic mental problems or neurocognitive disorders.
Assessments and measures
The contents and evaluation schedule are summarized in online Supplementary Table 3; more detailed information regarding the assessments and measures used in the present study are provided in Supplementary Table 4. With respect to trauma-related assessments, the type of injury was evaluated using the Life Events Checklist, injury severity was evaluated with the ISS and GCS, traumatic medical conditions and intensive care unit (ICU) treatment information were obtained from general practitioner records, and subsequent traumatic events and stress were determined using the Life Experiences Survey (LES).222326
For the general health assessments, medical records were examined to obtain information regarding the duration of hospitalization, body weight, height, systolic and diastolic blood pressure levels, pulse rate, and menstruation status. An inventory of somatic disease was conducted using detailed questions about the presence of and treatment for 15 different chronic illnesses. Additionally, detailed sociodemographic data regarding age, gender, ethnicity, partner or household status, socioeconomic status, religion, smoking, and drinking were collected.
To assess depression, the presence of a depressive disorder was determined using the MINI;24 the severity of depressive symptoms was assessed with the Hamilton Rating Scale for Depression (HAMD),27 the Hospital Anxiety and Depression Scale (HADS),28 the Clinical Global Impressions (CGI-I) scale, and the CGI Severity (CGI-S) scale;29 the presence of suicidal ideation was evaluated with the Brief Psychiatric Rating Scale (BPRS) and the SAD PERSONS scale (SADS);30 and lifetime suicide attempts were assessed with a past suicide attempt questionnaire. For the assessment of anxiety, the presence of an anxiety disorder was determined using the MINI;24 the severity of anxiety symptoms was assessed with the Hamilton Anxiety Rating Scale (HAMA),31 the HADS,28 the CGI-I, and the CGI-S;29 and abnormal illness behavior was evaluated using the Illness Attitude Scale (IAS).32
For the assessment of trauma related-disorders, the diagnosis and severity of ASD and PTSD were evaluated with the CAPS-5 and the Impact Event Scale-Revised.3334 Presently, there are no validated measures for the assessment of PTSD according to the criteria of the DSM-5; thus, the current protocol includes a modified version of the CAPS for the DSM-5 developed by the authors of the CAPS.25
To measure cognitive functioning, cognitive impairments were evaluated using the Korean Mini-Mental State Examination (K-MMSE) and the Perceived Deficits Questionnaire-Depression. 3536 In terms of assessing physical disability, activities of daily living and mobility were evaluated using the Modified Barthel Index, and health-related quality of life was assessed with the EuroQol-5 dimension.3738 For the functional disability assessments, functional impairments were evaluated with the Sheehan Disability Scale (SDS), and a global rating of current functioning was obtained using the Social and Occupational Functioning Assessment Scale (SOFAS).3940
In terms of the assessment of other psychosocial factors, previous episodic psychiatric problems were evaluated using standard questions, childhood trauma was assessed with the Childhood Adversity Questionnaire (CAQ),41 social support was determined with the Multidimensional Scale of Perceived Social Support (MSPSS),42 the perception of stress was measured with the Perceived Stress Scale (PSS),43 the ability to cope with stress was evaluated with the Connor-Davidson resilience scale,44 and personality was assessed with the Big Five Inventory. 45 Data regarding previous episodic psychiatric problems included age at onset, duration of illness, and family history of psychiatric disorders.
To identify biomarkers associated with PTS, blood samples were collected from the patients to evaluate neuroimmunological biomarkers, hypothalamic–pituitary–adrenal gland (HPA) axis biomarkers, and other blood biomarkers as well as genetic and epigenetic biomarkers. Blood samples for determination of neuroimmunological biomarkers and HPA axis biomarkers were obtained at 8:00 a.m. All samples were stored at -80℃ until immediatedly before assay and all were assyed in duplicate. Neuroimmunological biomarkers were measured using a multiplexed bead-based cytokine assay with Bio-Plex Pro Human Cytokine Tha/Th2 Panel kits (Bio-Rad Laboratories, Hercules, CA, USA) on the Luminex™ 100 system (Luminex, Austin, TX, USA) according to the manufacturer' instructions. HPA axis biomarkers were determined by using a commercially-available radioimmunoassay kit (DiaSorin Ins., Stillwater, MN, USA). Genomic DNA (1 µg) was extracted from leukocytes using the QIAamp DNA Blood Mini Kit (Qiagen, Valencia, CA, USA) following the manufacturer's suggested protocol. The DNA then underwent bisulfite treatment using the EpiTech Bisulfite Kit (Qiagen) according to the manufacturer's protocol. PCR products were sequenced using the PSQ 96M Pyrosequencing System (Biotage) according to the manufacturer's protocol. The level of the epigenome which programs the activity of our genome by several mechanisms, namely, DNA methylation, and RNA interference.
Additionally, heart rate variability (HRV), electrocardiogram data, and resting blood pressure levels were evaluated to examine electrophysiological biomarkers. HRV recordings were obtained in each subject using a standard electrocardiogram (ECG) recorder implemented in SA-6000 (Medicore Co. Ltd, Seoul, Korea). Power spectral analysis of HRV assesses the quantitative contribution of high frequency (HF; 0.15–0.4 Hz), low frequency (LF; 0.04–0.15 Hz), and very low frequecy (VLF; 0.0033–0.04 Hz), 5-minute total power, LF/HF ratio. The index of particular interest was the SDNN (standard deviation of the beat-to-beat interval averaged over successive 5 min invervals).
CONCLUSIONS
The BioPTS study will be a significant contribution to research on the complex relationships between psychological problems and severe physical injury. The specific prospective naturalistic study design might facilitate other related studies and enhance the current understanding of this issue. Additionally, the BioPTS study will provide an additional means of access for clinicians who treat these patients.
Acknowledgments
The study was funded by a grant of National Research Foundation of Korea Grant (NRF-2015M3C7A1028899) to Professor JM Kim.
References
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.4306/pi.2017.14.4.513
Supplementary Table 1
Previous studies on the epidemiology of posttraumatic syndrome (PTS) following severe physical injury
Supplementary Table 2
Previous studies on the biomarkers of posttraumatic syndrome (PTS) following severe physical injury
Supplementary Table 3
Schedule of assessments for the biomarker based diagnostic algorithm for posttraumatic stress syndrome (BioPTS) study
Supplementary Table 4
Detailed information on assessments and measurements for the biomarker based diagnostic algorithm for posttraumatic stress syndrome (BioPTS) study