Effects of Group Cognitive-Behavioral Therapy in Young Patients in the Early Stage of Psychosis
Article information
Abstract
Objective
To develop a model of group cognitive-behavioral therapy (CBT) for Korean patients with early psychosis.
Methods
The group CBT utilized in the present study consisted of metacognitive training, cognitive restructuring, and lifestyle managements. The Subjective Well-being Under Neuroleptics (SWN-K), Ambiguous Intentions Hostility Questionnaire (AIHQ), Drug Attitude Inventory (DAI), Beck Depression Inventory (BDI), Perceived Stress Scale (PSS), and Clinical Global Impression (CGI) were administered prior to and after CBT sessions. The participants were categorized into two groups according to the median duration of untreated psychosis (DUP; 4 months).
Results
A total of 34 patients were included in this analysis. From pre- to post-therapy, there were significant increases in the SWN-K and DAI scores and significant decreases in the hostility subscale of the AIHQ, PSS, and CGI scores. Significant time × DUP interaction effects were observed for the SWN-K, DAI, and BDI scores, such that there were significant changes in patients with a short DUP but not in those with a long DUP.
Conclusion
The group CBT program had a positive effect on subjective wellbeing, attitude toward treatment, perceived stress, and suspiciousness of young Korean patients with early psychosis. These effects were particularly significant in patients with a short DUP.
INTRODUCTION
The intent of early intervention procedures for patients with schizophrenia is to provide effective treatment during the early stages of the disorder to reduce its ultimate severity.12 The primary method of early intervention involves shortening the duration of untreated psychosis (DUP), which is defined as the period from the onset of psychosis to the onset of antipsychotic treatment.3 After controlling for relevant confounding variables, a longer DUP was found to be associated with a lower rate of remission of positive symptoms, worse global functioning, and a poorer quality of life at follow-up.45678 Therefore, the DUP represents a modifiable predictor of outcomes during the early course of schizophrenia.9 A secondary method of early intervention involves intensive treatment during the critical period of schizophrenia, i.e., the first 3–5 years, because the future course and prognosis of patients are determined during this period.1011
The guideline of the National Institute for Health and Care Excellence (NICE) in the UK recommends that early interventions provided by psychosis services should be accessible to all individuals with a first episode or first presentation of psychosis, irrespective of that individual's age or DUP.12 Furthermore, these early interventions should provide a full range of pharmacological, psychological, social, occupational, and educational interventions. A key element of the psychological interventions for individuals with first-episode psychosis is cognitive-behavioral therapy,1213 the efficacy of which has been well established.14151617 The components of cognitive-behavioral therapy (CBT) for patients with psychosis should include the establishment of a relationship between the patient's thoughts, feelings, and actions and their symptoms and functioning, as well as the monitoring of their thoughts, feelings, and behaviors with respect to their symptoms.1214 Additionally, CBT should promote alternative ways of coping with the target symptoms and reducing the distress associated with the disorder.12
Although many studies have investigated the effects of CBT in patients with psychosis, a majority of these studies have focused on individualized CBT interventions rather than group interventions.18 Recently, group therapies that treat cognitive biases have been applied to patients with psychotic disorders.181920 One example is group metacognitive training (MCT),2122 which have been reported to effectively improve delusional symptoms, self-esteem, and well-being in patients with schizophrenia.2324
Although active clinical and psychosocial services, including CBT, are typically provided to patients with psychosis from the early stage of illness in Western countries,14 services and research in this area are not yet well developed or actively reported in Asian countries. Thus, the present study aimed to develop a model of group CBT for Korean patients with early psychosis and to evaluate the effectiveness of this model.
METHODS
Development of the group CBT program
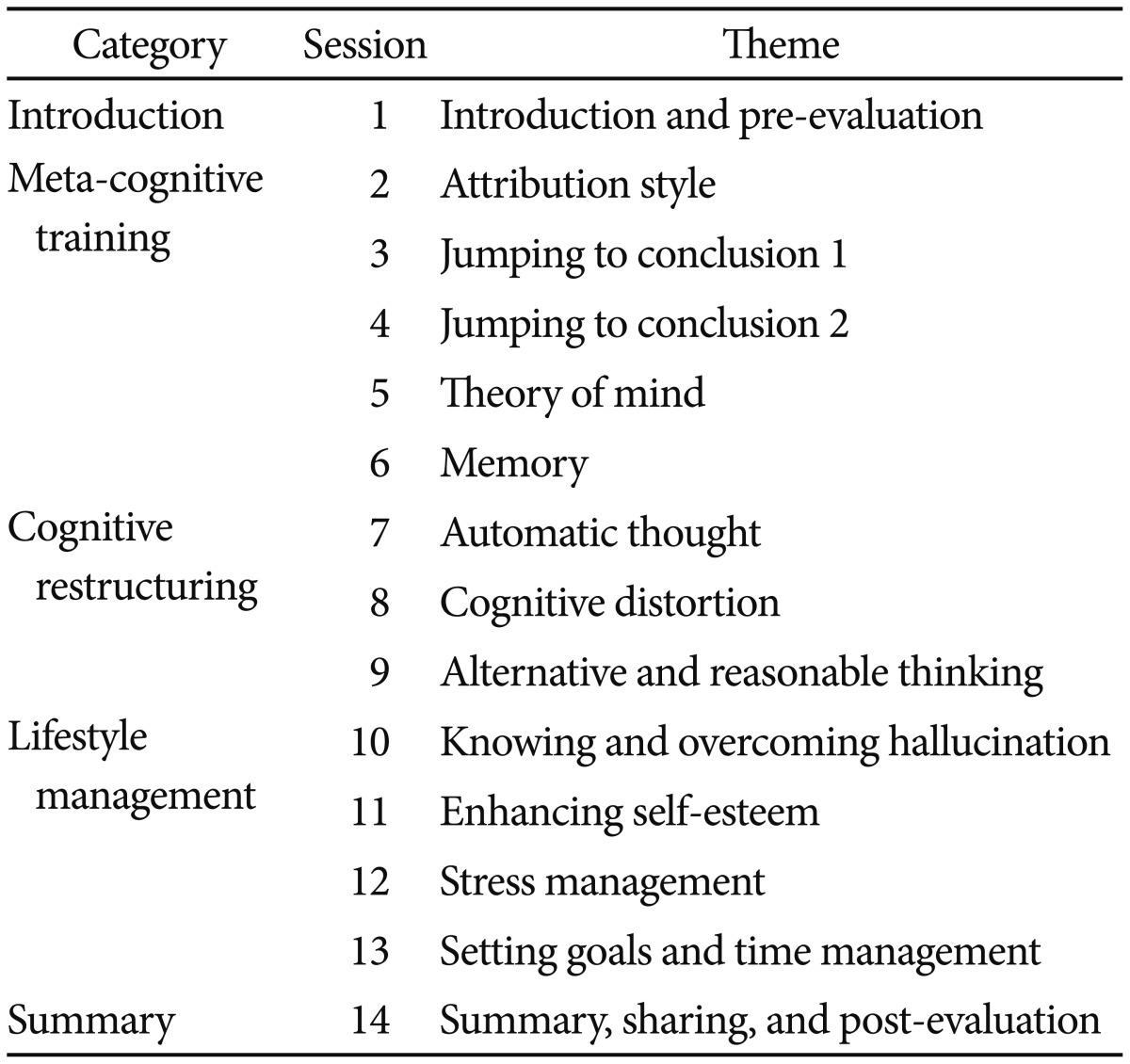
Gwangju Bukgu-Community Mental Health Center (CMHC) initiated a program that includes early intervention services for young people with psychosis, as part of a national demonstration project exhibiting special community mental health services in Korea. Clinical and research teams at Gwangju Bukgu-CMHC and Chonnam National University Hospital launched a 13 session group CBT program in August 2012 and then revised it to include 14 sessions in 2014 (Table 1); this CBT program consists of three components: MCT, cognitive restructuring, and stress management. First, five sessions of the MCT procedure, which was developed at the University Medical Center Hamburg-Eppendorf, were selected and modified for the present study.21 The MCT is a manualized group treatment program that targets dysfunctional coping styles and cognitive biases involved in the formation and maintenance of psychotic symptoms such as attributional distortions, jumping to conclusions, and impaired social cognition.2122 After these were implemented, three sessions of cognitive restructuring using Beck's cognitive therapy model were conducted,25 and then three or four lifestyle management sessions that included stress management, self-esteem enhancement and the process of setting goals were conducted.2126 The first and last sessions were used for introduction and summary purposes, respectively, as well as evaluations and feedback. In addition to the many pictures used during MCT, approximately 10 Korean drama or comedy clips were used to practice cognitive therapy.
Subjects and measures
The participants in the present study were young Korean individuals who utilized the early intervention services, including group CBT, of Gwangju Bukgu-CMHC; these services are provided to people between 15 and 35 years of age.2728 Most patients who received the early intervention service had a psychotic disorder lasting less than 5 years.
The present study was a retrospective chart review study. For inclusion in this study, the patients were required to be 15–35 years of age, have a diagnosis of a psychotic disorder or psychotic features according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, fifth edition,29 have completed more than 70% of the sessions, and have completed all scales before and after the CBT sessions. This study was approved by the Institutional Review Board of Chonnam National University Hospital.
Measures
Demographic and clinical information, including age, gender, education, duration of illness, diagnosis, history of psychiatric admission, history of suicide attempts, chlorpromazine equivalent dosage of antipsychotics, and DUP, were collected from the clinical records at Gwangju Bukgu-CMHC. Self-reports were routinely obtained during the first and final sessions to collect feedback from the participants. These reports included the Subjective Well-being Under Neuroleptics short form (SWN-K) scale for subjective quality of life,3031 Ambiguous Intentions Hostility Questionnaire (AIHQ) for hostile social cognitive biases and paranoia,3233 Drug Attitude Inventory (DAI) for attitude toward treatment,3435 Beck Depression Inventory (BDI) for depression,3637 and Perceived Stress Scale (PSS) for stress levels.3839 General severity was determined using the Clinical Global Impression (CGI), which was performed by the case managers.40
The AIHQ is a self-report scale comprised of 15 hypothetical negative situations that vary in intentionality (ambiguous, intentional, and accidental situations).41 This study used the five questions involving ambiguous situations.42 The AIHQ yields Hostility and Aggression bias scores and a composite Blame bias score. The perceived Hostility and Aggression bias scores are calculated by objective ratings of the participant's written responses. The composite Blame score is the mean score of the subject's ratings of intent, anger, and blame.43 A greater tendency toward perceived hostility with the AIHQ is a significant predictor of the degree of persecution or paranoia in patients with schizophrenia.4143 The SWN-K, which is the most widely used self-report scale for assessing the well-being of patients, includes 20 items that are rated on a 6-point Likert scale. The SWN-K measures five domains: emotional regulation, mental functioning, self-control, social integration, and physical functioning. Higher scores on the SWN-K and DAI indicate better status and higher AIHQ, BDI, PSS, and CGI scores indicate worse clinical status.
The DUP was assessed by a clinical interview. Due to the lack of standardized criteria available to distinguish between a short and long DUP, the median split approach was selected to maximize statistical power and to optimize the interpretation of the findings.343
Statistical analysis
The participants were categorized into two groups according to the median value of DUP. The sociodemographic and clinical variables of the two groups were compared using the chi-square test, independent t-test, or Mann-Whitney U test, as appropriate. Repeated measure analysis of variance (ANOVA) for outcome measures was conducted to evaluate time effects between at baseline and at the endpoint. To evaluate the effects of the DUP as a moderator of treatment effectiveness, a two-way repeated-measure ANOVA with time and DUP representing values below or above the median was conducted after adjusting for gender and baseline scores. The two-way interaction compared the slope of linearized time for patients in the group CBT program who had a DUP either higher or lower than the median. The effect size estimates were determined using the method of Cohen, which was computed as the difference between the endpoint and baseline mean values divided by the standard deviation.44 All statistical tests were two-tailed, and a p value<0.05 was considered to indicate statistical significance. The Statistical Package for Social Sciences version 21.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
RESULTS
The present study initially included 58 patients who participated in the group CBT program between September 2012 and December 2015; each group CBT session included 5–9 patients. Among them, 47 (81.0%) patients completed more than 70% of the total sessions and 11 (19.0%) patients dropped out, mainly due to lack of interests. After excluding patients who did not complete all scales both before and after group CBT (n=5) and who were not diagnosed with a psychotic disorder (n=8), 34 patients were included in this analysis. The mean age of the participants was 23.2±4.7 years, and the median (interquartile range) duration of illness and DUP were 3.8 years (1.1–6.0) and 4.0 months (1.7–18.2), respectively. Of the participants, 24 (70.6%) were diagnosed with schizophrenia, seven (20.6%) were diagnosed with other specified schizophrenia spectrum disorder, and three (8.8%) were diagnosed with affective psychosis. Additionally, 24 (70.6%) had a history of psychiatric hospitalization, 16 (47.1%) had a history of suicide attempts, and 26 (76.4%) patients had CGI scores of 3 (mild) or 4 (moderate), while none had scores higher than 5 (severe).
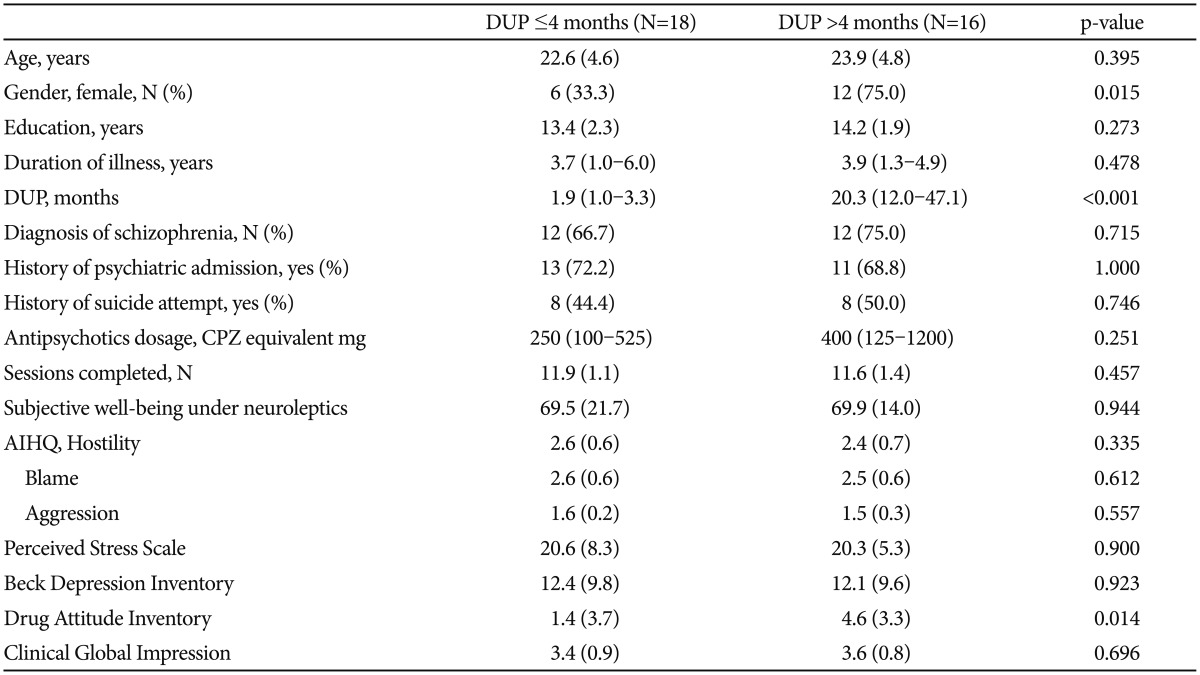
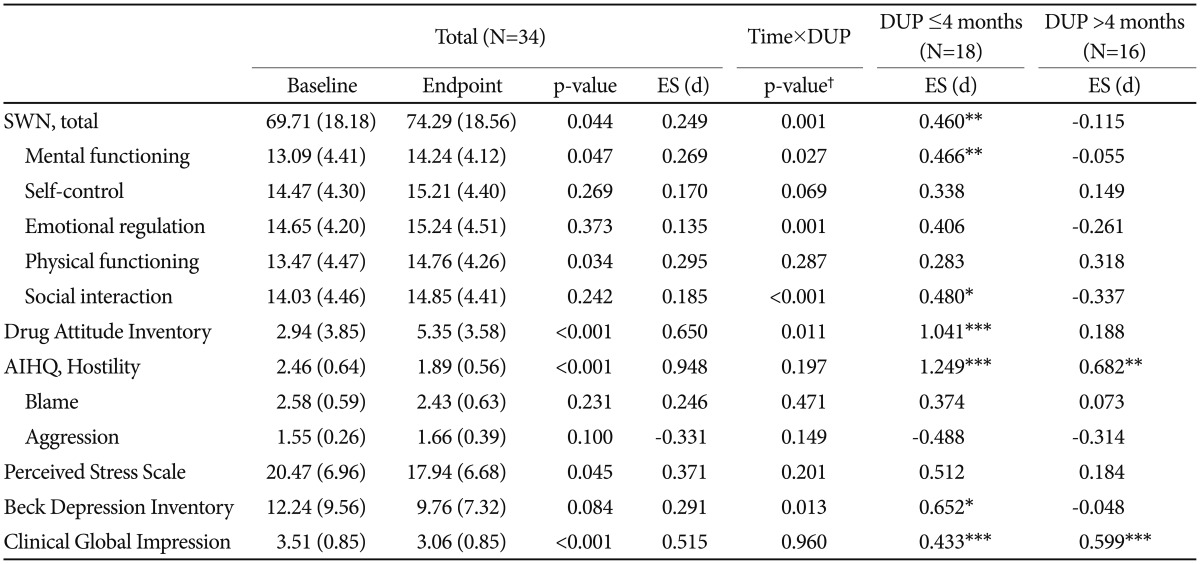
When the participants were categorized into two groups according to the median DUP (4 months), it was revealed that patients with a DUP >4 months were more likely to be female and to have a significantly higher DAI score. No significant differences were observed between the two groups in any of the other clinical characteristics, including scores on the other scales and number of sessions completed (Table 2). Table 3 shows the changes in scores on the scales after group CBT. Significant time effects were observed for the SWN, DAI, the hostility subscale of the AIHQ, PSS, and CGI. The SWN-K and DAI scores exhibited a significant increase from pre- to post-therapy, while scores on the PSS, CGI, and the hostility subscale of the AIHQ decreased significantly. The scores for the mental functioning and physical functioning subscales of the SWN-K also increased significantly. The BDI scores decreased after the CBT sessions, but this change did not reach statistical significance (p=0.084).
After adjusting for gender and baseline scores, significant time×DUP interactions were observed for the SWN-K, DAI, and BDI scores (Table 3). Figure 1 shows that there were significant changes on these scales in the short DUP group (≤4 months) but not in the long DUP group (>4 months). The effect sizes for the improvements in these scales were either medium or large in the patients with a short DUP (Cohen's d=0.459–1.052). There were also significant time×DUP interactions observed for the mental functioning, emotional regulation, and social interaction subscales of the SWN-K (Figure 1), such that patients with a short DUP exhibited significantly increased scores. Scores on the CGI and hostility subscale of the AIHQ were significantly decreased in both groups, and the effect sizes for the improvements in these scales were medium and large, respectively. There was no relapse, re-hospitalization, or serious adverse event associated with the group CBT.
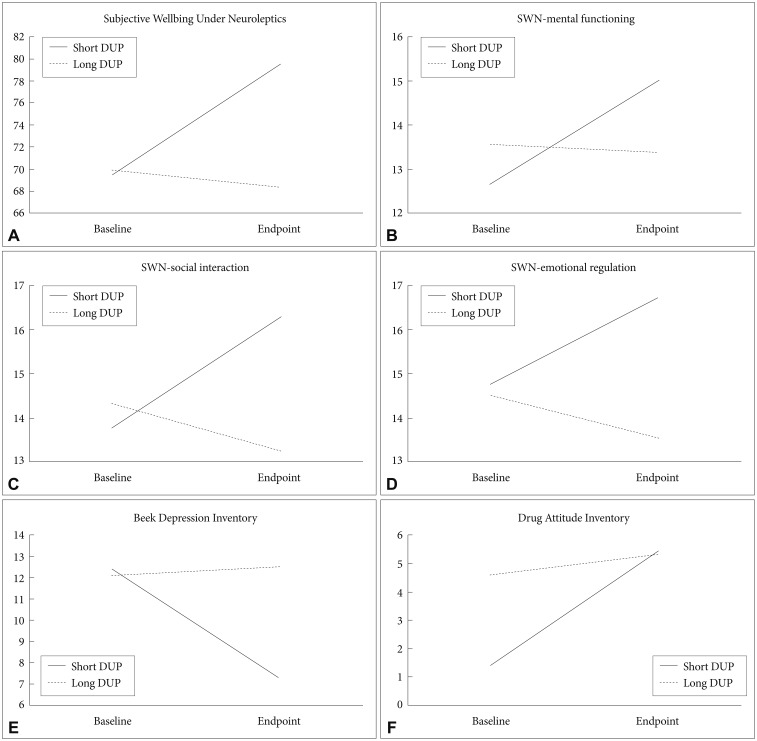
Changes in scores on the scales after group cognitive-behavioral therapy according to the median duration of untreated psychosis (DUP). p-values of paired t-tests in short DUP and long DUP groups are (A) 0.007 and 0.469, (B) 0.005 and 0.804, (C) 0.029 and 0.108, (D) 0.075 and 0.136, (E) 0.018 and 0.810, and (F) <0.001 and 0.370, respectively. SWN: Subjective Wellbing Under Neuroleptics.
DISCUSSION
The present findings demonstrated that the group CBT program for patients with early psychosis effectively increased subjective well-being and attitude toward treatment and decreased suspiciousness and perceived stress. The improvements in well-being and attitude toward treatment were particularly significant in patients with a DUP that was shorter than 4 months, and the effect sizes were moderate to large, while suspiciousness and global severity improved regardless of the DUP. To the best of our knowledge, this is the first study to show the beneficial effects of a group CBT program on subjective responses in young Asian patients with early psychosis, and that these effects were mediated by the DUP. In addition, the drop-out rate was not high, and no serious adverse event associated with group CBT was observed. This suggests that group CBT may be an effective and practical therapeutic tool in Korean patients with early psychosis.
The group CBT program used in the present study is composed of three parts. Therapeutic mechanisms and theoretical backgrounds of these three parts are somewhat heterogeneous but are closely associated with each other in this program. The first part, MCT, aims to enhance patient awareness regarding cognitive biases and cognitive flexibility.21 Metacognition refers to the general ability to think about thinking, i.e., the ability to think about one's mental state and the mental states of others.45 Training programs that improve metacognition, which is impaired in patients with schizophrenia, may help motivate patients to restructure their cognitive distortions. Previous studies investigating insight into an individual's illness and cognitive flexibility, or the ability to consider alternative beliefs, as predictors of better CBT outcomes have supported the potential effectiveness of the combination of MCT and formal cognitive therapy.46474849 After learning cognitive restructuring, the patients were encouraged to adopt these skills in real life with subsequent sessions on stress and time management and enhancing self-esteem. This sequential combination of techniques may help patients decrease suspiciousness and perceived stress while increasing their subjective wellbeing and positive attitudes toward treatment.
Group CBT is a cost-effective method to deliver cognitive behavioral therapies, but compared with individual CBT, this technique has recently been developed for and evaluated in patients with psychosis. While previous studies have shown that group CBT and MCT effectively treat psychosis,13162324 there are conflicting results and heterogeneity in terms of the outcome measures.1518 For example, some patients experience significant benefits from participating in group psychotherapy, whereas others achieve only minimal gains.49 Alliance with one's therapist, a feeling of cohesion, and conscientiousness are predictors of better group CBT outcomes.2050 The present findings suggest that the DUP is also a predictive factor in the effectiveness of group CBT.
Many previous studies have shown that the DUP influences various aspects of short-term and long-term improvements in the symptoms of patients with first-episode psychosis.68515253 Furthermore, meta-analyses investigating the associations between the DUP and long-term outcomes determined that a longer DUP is significantly correlated with a lower likelihood of remission, poor social functioning, and worse global outcomes.35455 However, definitive conclusions cannot be made regarding the longitudinal effects of the DUP on employment and quality of life, due to the small number of studies evaluating these issues.55 Furthermore, there is a relative lack of evidence showing the influences of the DUP on the effects of specific psychosocial treatments, including CBT, in young patients with psychosis.
The present study findings, showing that there were significant improvements in subjective responses in patients with a short DUP but not a long DUP, support the need for early intervention in psychosis services.1 Thus, delays in treatment may reduce the therapeutic potential of psychosocial interventions provided during the course of the illness. Cognitive deficits, which is associated with an extended DUP,5657 may interfere with a patient's ability to engage with existing forms of CBT, because cognitive therapies require patients to utilize memory and problem-solving functions.58 In the short DUP group, functional and developmental reserves against the toxic effects of a long DUP may also contribute to a favorable response following group CBT.58
A recent study conducted in the U.S. revealed that the DUP influences the treatment response following comprehensive psychosocial services in patients with first-episode psychosis.42 In that study, participants with a median DUP of ≤74 weeks showed greater improvements in quality of life and psychopathology compared with those with a longer DUP and those in community care. The authors proposed that reducing the DUP from its current level of approximately 1 year to a recommended standard of 3 months should be a major focus of applied research efforts.596061 Patient outcomes are significantly worse when the DUP exceeds 3 months.462 The present findings indicated that a DUP shorter than 4 months may be critical to achieve a good response to psychosocial interventions in Korean patients with early psychosis.
There were significant improvements in the score on the hostility subscale of the AIHQ in both the short and long DUP groups. A perceived hostility bias may play a pivotal role in the paranoia associated with the first psychotic episode of schizophrenia and/or its prodromal phase, and this bias has been linked to a high paranoia score.43 The findings of the present study are compatible with those of previous studies that showed improvements in positive psychotic symptoms following MCT and individual CBT.23 Although the AIHQ is a self-report questionnaire, the score on the hostility subscale is rated by clinicians based on the attributional style of patients who respond to the questionnaire. The present study also demonstrated significant improvements in general clinical impression, as rated by clinicians, of patients regardless of the DUP. This is in line with a recent study that found the DUP does not influence the effects of MCT on schizophrenia symptoms.45 However, the group CBT procedure used in the present study, which included MCT, improved subjective well-being, attitude toward treatment, and depression more effectively in patients with a short DUP than in those with a long DUP. A previous study found that a longer DUP and a poorer level of insight predicted poor adherence to CBT, but this study did not investigate changes in therapeutic outcomes according to the DUP.57 In the present study, no differences in adherence to group CBT according to the DUP were detected, but scores on the DAI, which represent one's attitude toward treatment, were significantly improved in the short DUP group.
The SWN-K and DAI have been widely used to measure subjective responses to and attitudes about pharmacological treatments, and the importance of subjective measures has been repeatedly addressed in recent studies on schizophrenia.6364 Subjective well-being is highly and positively correlated with quality of life,6566 and it has been increasingly addressed in studies assessing the clinical courses and outcomes of patients with schizophrenia.67686970 In the present study, the effect size for the improvement in the total SWN-K score was moderate, and the mental functioning and social integration scores significantly improved with medium to large effect sizes in the short DUP group. Improvement in social integration is one of the most important treatment goals for patients with schizophrenia.71 Group interactions and activities as well as content of the CBT modules that were intended to enhance self-esteem, and the use of coping strategies, might have contributed to these improvements. It is interesting that the attitude toward medication significantly improved in the present study, even though the group CBT program did not include formal psychoeducation. However, the therapeutic relationship with one's case manager and peer sharing about one's treatment experience might have contributed to this.
The present study has several limitations that should be noted. First, the sample size was relatively small. Second, this was a retrospective study and formal objective ratings of the patients' psychopathologies and functioning were not included. Third, assessments of neurocognitive and intellectual functioning, which may be associated with the DUP and the ability to engage during CBT, were not performed. Fourth, the effects of other treatment factors were not controlled because this study had not control group. Finally, while the mean age of the subjects in this study was in the early twenties, most patients were not seen at their first episode. Therefore, a prospective controlled study is warranted, mainly focusing on the first episode or ultra-high risk stage in the Korean population.
In conclusion, the group CBT program used in the present study had a positive effect on subjective well-being, attitude toward treatment, perceived stress, and suspiciousness of young Asian patients with early psychosis. These effects were more pronounced in those with a shorter DUP, suggesting that the receipt of appropriate treatment at the proper time during the course of one's psychotic illness can have a substantial impact on outcome. The present study provides additional support for early identification of psychosis and intervention methods that can improve its course.
Acknowledgments
This study was supported by grants of the Korean Mental Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HM15C1140 and A120051). This research work was conducted as part of the Gwangju Mental Health Demonstration Project supported by Ministry of Health & Welfare and Gwangju Metropolitan city, Republic of Korea. We thank Jae-Kyeong Kim and Jin-Hee Hong for their assistance in subject recruitment.