Design and Methodology of the Korean Early Psychosis Cohort Study
Article information
Abstract
The present study details the rationale and methodology of the Korean Early Psychosis Cohort Study (KEPS), which is a clinical cohort investigation of first episode psychosis patients from a Korean population. The KEPS is a prospective naturalistic observational cohort study that follows the participants for at least 2 years. This study includes patients between 18 and 45 years of age who fulfill the criteria for one of schizophrenia spectrum and other psychotic disorders according to the diagnostic criteria of DSM-5. Early psychosis is defined as first episode patients who received antipsychotic treatment for fewer than 4 consecutive weeks after the onset of illness or stabilized patients in the early stages of the disorder whose duration of illness was less than 2 years from the initiation of antipsychotic treatment. The primary outcome measures are treatment response, remission, recovery, and relapse. Additionally, several laboratory tests are conducted and a variety of objective and subjective psychiatric measures assessing early life trauma, lifestyle pattern, and social and cognitive functioning are administered. This long-term prospective cohort study may contribute to the development of early intervention strategies and the improvement of long-term outcomes in patients with schizophrenia.
INTRODUCTION
Psychotic disorders such as schizophrenia are often chronic and disabling in a number of clinical aspects, including social and occupational functioning, which are characteristic factors and key diagnostic criteria associated with this disorder. In fact, there are often major changes in the psychosocial functioning of patients with schizophrenia spectrum disorders within the first 3 years of onset even though the decline infunction tends to plateau thereafter.1 Therefore, the first 3 years of this disorder have been described as a critical period during which the future course and prognosis of the patient is determined. McGorry suggested that the critical period for psychotic disorders can be regarded as covering the period following recovery from a first episode of psychosis and extending for up to five years subsequently.2
Over the last 3 decades, a number of clinical cohort studies have investigated the early stages of psychotic disorders.3456 These types of prospective cohort studies that focus on patients with first episode psychosis provide an opportunity to identify prognostic factors in the early stages of the disorder while minimizing the confounding effects of treatment interventions or secondary disabilities.7 Despite the obvious advantages of these early stage cohort studies, the majority has included only Western populations that have relatively superior mental health resources, and thus, the findings may not be generalizable to the rest of the world.8 For example, ethnic and sociocultural factors have been shown to influence the treatment pattern and clinical course of patients with psychotic disorders.9 To our knowledge, only a few large prospective longitudinal cohort studies investigating first episode psychosis have been published using subjects from Asian countries.810
In Korea, mental health services are typically characterized by low accessibility to psychiatric treatment, high caseloads, and a relatively large incidence of inpatient care.11 The duration of untreated psychosis (DUP), which is related to a poor prognosis for patients with schizophrenia,1213 is comparatively long in Korea relative to that of Western countries14 and may be attributed to the high level of stigma associated with psychosis and psychiatric treatment.15 Therefore, research investigating Korean patients with first episode psychosis and objective assessments of clinical and community treatment services are required to determine specific models of treatment that are appropriate for Korean populations.
Recently, early intervention services for young individuals with psychotic disorders have begun to be provided by some university hospitals and community mental health centers. Additionally, a nationwide long-term cohort study investigating the naturalistic clinical courses of patients with first episode psychotic disorders was initiated; the Korean Early Psychosis Cohort Study (KEPS) is the first long-term observational prospective cohort study of clinical outcomes in patients with psychotic disorders in the early stage of illness. The primary goals of the present study are to provide an overview of the KEPS and to detail its design and methodology.
METHODS
Aims
The primary aims of this cohort study are to investigate the clinical trajectories of patients with first episode psychosis and to identify the risk and protective factors associated with relapse and recovery. It is the goal of the present authors that this long-term prospective cohort study will be used to develop an optimal mental health services system and effective policies for the treatment of Korean patients with first episode psychosis.
Study population
The KEPS includes patients between 18 and 45 years of age who fulfill the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) for schizophrenia, schizophreniform disorder, schizoaffective disorder, delusional disorder, brief psychotic disorder, or other specified schizophrenia spectrum and other psychotic disorders including attenuated psychosis syndrome (APS).16 Early psychosis is defined as follows: 1) first episode patients who received antipsychotic treatment for fewer than 4 consecutive weeks after the onset of illness; and 2) stabilized patients in the early stages of the disorder whose duration of illness was less than 2 years after the initiation of antipsychotic treatment and whose current antipsychotic treatment dosage had not changed for at least 2 months. The exclusion criteria consists of patients with a substance- or medication-induced psychotic disorder, psychotic disorder due to another medical condition, mental intellectual disability disorder, and/or severe neurological disorders such as epilepsy, stroke, dementia, or Parkinson's disease.
Sociodemographic and clinical data
The baseline data includes age, gender, diagnosis, education, type of medical insurance, economic status, area of residence (rural or urban), family history of psychiatric illness, familial support (5-point Likert scale), presence of a cohabitant, prescribed medications, comorbid mental and physical illnesses, illness duration, and DUP, which was defined as the amount of time from the appearance of the first psychotic symptoms for more than several days to the time when antipsychotic treatment or a psychiatric hospitalization occurred. Follow-up visit evaluations include adherence to medication, type and length of employment, type of job, use of medical and mental health resources, and socioeconomic costs, including medical costs and time spent on hospital visits and care.
Psychiatric measures
The KEPS utilizes several objective scales, including the Positive and Negative Syndrome Scale (PANSS),1718 Calgary Depression Scale for Schizophrenia (CDSS),192021 Clinical Global Impression (CGI),22 Social and Occupational Functioning Assessment Scale (SOFAS),23 and Columbia-Suicide Severity Rating Scale (C-SSRS).24 Additionally, a dimensional diagnosis using the DSM-5 criteria is conducted to rate eight key psychopathological dimensions of psychotic disorders. A research or treating psychiatrist rates all of the objective measures.
The KEPS also includes several subjective self-rating measures that are administered by a research nurse: the Prospective and Retrospective Memory Questionnaire (PRMQ)25 for measuring prospective and retrospective memory slips in everyday life; the Early Trauma Inventory Self Report-Short Form (ETISR-SF)26 for measuring childhood trauma, including physical, emotional, and sexual abuse as well as general trauma; the Brief Core Schema Scales (BCSS)27 for the assessment of schemata concerning self and others; the Brooding Scale (BS) (Chung, in preparation); the Basic Empathy Scale (BES)28 for measuring affective and cognitive empathy; the Brief Resilience Scale (BRS)29 for the assessment of the ability to bounce back or recover from stress; the Big Five Inventory-10 item (BFI-10)3031 to identify personality patterns; the Early Signs Scale (ESS)32 for measuring changes in key phenomenological and behavioral symptoms; the Social Functioning Questionnaire (SFQ)33 for the quick assessment of perceived social function; the Drug Attitude Inventory-10 item (DAI-10)3435 for measuring subjective attitudes toward antipsychotic medication; the Subjective Well-being Under Neuroleptics-Short Form (SWN-K)3637 for measuring subjective health-related quality of life; the Sexual Health Scale38 as a visual analogue scale (VAS) to assess sexual desire, function, orgasm, and satisfaction; the Frequent Food Questionnaire (FFQ)39 for measuring eating patterns and nutritional intake; the Physical Activity Rating (PAR)40 for categorizing a person's level of physical activity; the Family Adaptability and Cohesion Evaluation Scales-III (FACES-III)41 for measuring family adaptability and cohesion; the Alcohol Use Disorders Identification Test (AUDIT)42 as a screening instrument for hazardous and harmful alcohol consumption; and the Fagerstrom Test for Nicotine Dependence (FTND)43 for measuring the degree of nicotine dependence. The need for treatment services is determined using the VAS in terms of the explanation of illness, explanation of medication, time for personal interviews with clinicians, special group treatment programs, education on lifestyle (exercise, eating, sleep), communication among family members, and employment.
Laboratory measures and cognitive and emotional tasks
All patients included in the present study undergo assessments of height, weight, waist circumference, and systolic and diastolic blood pressure levels. Fasting venous blood samples are collected to determine the levels of cholesterol, glucose, hepatic function, and complete blood counts. For the exploratory genetic tests and measures of essential polyunsaturated fatty acids (EPUFA), the buffy coat and red blood cells are frozen at −80℃ and stored at 5 of the 10 study sites. They will be used as biologic markers of pathogenesis and long-term outcomes.44
Exploratory neurocognitive function assessments are conducted at 5 of the 10 study sites using the following computerized tests:45 attention span and vigilance are measured with the Digit Span Test (DST); verbal and visual memory abilities are assessed with the modified Rey Auditory Verbal Learning Test (VLT)4647 and the Visual Recognition Test,48 respectively; executive function and cognitive flexibility are measured with the Wisconsin Card Sorting Test;49 and sustained attention is assessed using the number of correct responses and reaction time on the Continuous Performance Test (CPT).50 Additionally, the Digit-Symbol Substitution Test (DSST),5152 which measures general cognitive efficiency, working memory, and information processing, and the Controlled Oral Word Association Test (COWAT),53 which measures letter and category fluency for verbal fluency, working memory, and cognitive speed, are manually performed in the study. For emotional task, we use facial expression recognition test (FERT) in which 8 facial expressions (anger, contempt, disgust, fear, happiness, neutral, sadness, and surprise) are presented on computer screen and participants are instructed to press response buttons that correspond to the emotion that is being displayed. Facial expressions were standardized with Korean actors.54 Each expression is presented for 750 ms with inter-trial interval of 4,500 ms. There are 16 trials of emotion labeling, two trials for each of the eight emotions. Measures of reaction time and response accuracy are recorded by the computer.
Study design
The KEPS is a prospective naturalistic observational study that includes a follow-up period of at least 2 years and 4 years when possible. The primary outcome measures are treatment response,555657 remission,58 recovery,65960 and relapse;61 the definitions of these variables are summarized in Table 1. The recovery criteria will be adjusted for all participants. The other criteria will be adjusted for all participants except those with APS,62 who have relatively low baseline PANSS or CGI-S scores. For participants with APS, transition to psychotic disorder and remission from the APS criteria according to a diagnostic interview are the outcome measures.63
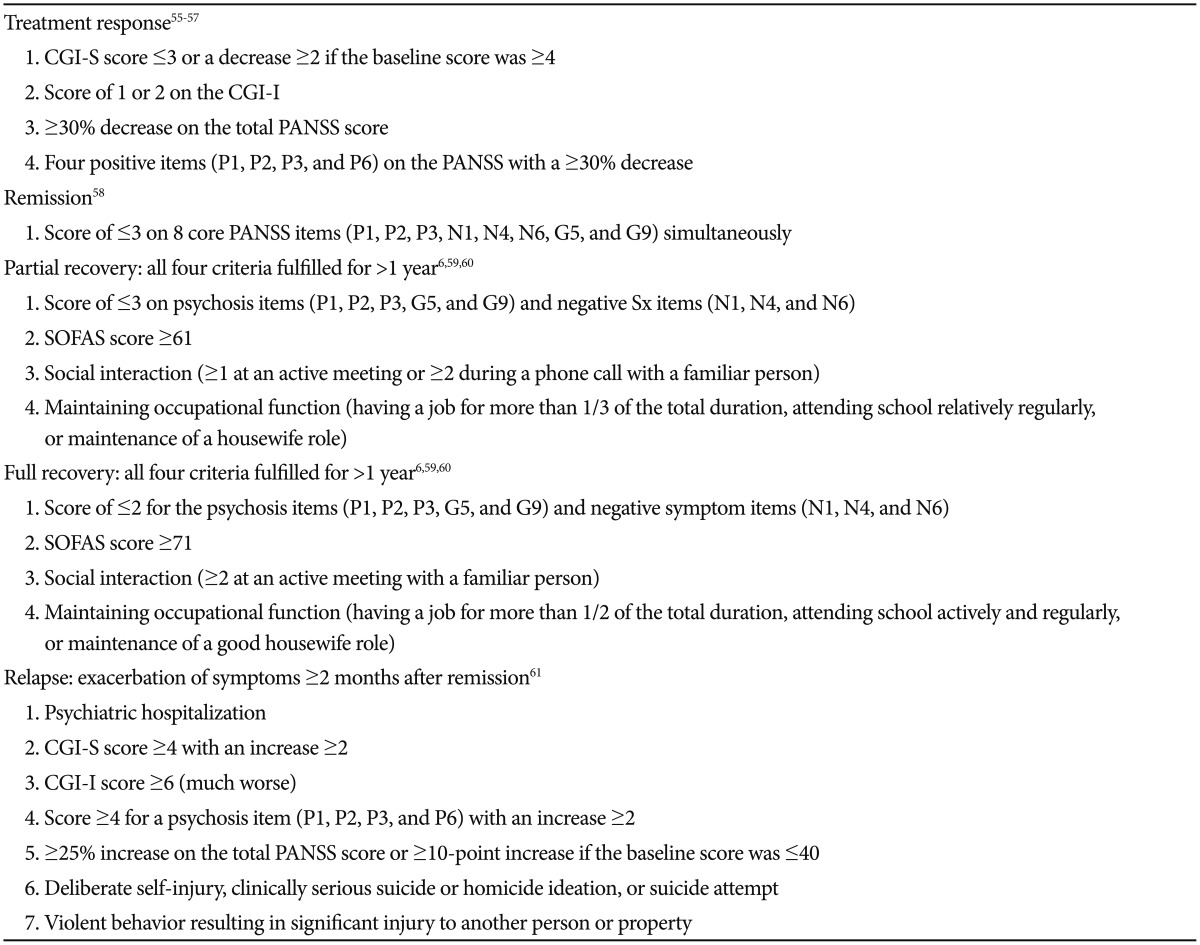
Operational criteria for treatment response, remission, partial recovery, full recovery, and relapse
Early psychotic symptoms can be diagnosed as various disorders and can change with the clinical course of the illness. Diagnosis at the first psychotic episode can be also changed according to the presence of comorbid mood episode or residual symptoms. Therefore, the diagnostic stability is regularly investigated using dimensional diagnosis of DSM-516 and the Mini International Neuropsychiatric Interview (MINI),64 which is administered at baseline, 6 months, 1 year, and 2 years. Primary outcome measures will be also compared according to the diagnosis at baseline.
The baseline assessments are divided into two stages as follows: 1) after screening and registration to a cohort, the PANSS and CGI-S are administered to evaluate the presence of acute psychotic symptoms and 2) a full baseline assessment that includes the PANSS and CGI-S are administered when patients are stabilized from their active psychotic symptoms, which is generally within 4 weeks of the initial baseline assessment. Follow-up assessments are conducted at 2, 6, 9, and 12 months and then biannually through the 3rd year and finally at the 4th year. The visit window is ±2 weeks from a scheduled visit until the 12-month visit and then ±4 weeks after that. The assessment measures that are administered at each follow-up visit are summarized in Table 2.
Drop-out was defined as missing two consecutive outpatient clinic visits. However, patients would be included in the cohort study if they returned to the clinic. After dropping out, the researchers try to contact them for follow-up evaluations at 1 and 2 years. To reduce the drop-out rate, when patients miss a clinic visit, the research team will call them to remind them about their visit.
Because this is a naturalistic observational study, the psychiatric medications and treatments are decided by the treating psychiatrists and are not influenced by the study design. However, patients with a SOFAS score less than 70 are recommended for psychosocial services in a community mental health center. The long-term outcomes according to the use of psychosocial services in a community mental health center will be compared in future studies.
The KEPS began in September 2014 and will be conducted for 5 years. A total of 9 university hospitals and 1 national mental hospital in Korea participate in this cohort study and more than 400 subjects with first episode psychotic disorders will be enrolled. All experimental protocols were approved by the institutional review boards and ethics committees of the applying sites.
Statistical analysis
The KEPS will conduct descriptive analyses of psychosocial and clinical characteristics, including DUP, changes in diagnosis, frequency of early trauma, and prevalence rates of metabolic syndrome and suicide attempts. The group comparisons will be conducted according to short and long DUP, diagnosis, subtype, use of community mental health centers, remission, relapse, and recovery. The changes in psychiatric measure scores, cognitive function, and diagnosis will be also analyzed, and the correlations of nutritional status and EPUFA with the psychiatric outcomes will be provided. The predictors of remission, relapse, and recovery will be analyzed with a logistic regression analysis and a Cox proportional hazard regression will be conducted to identify time and factors related to remission and recovery.
Psychotic disorders, including schizophrenia, are often chronic illnesses that tend to involve recurrent relapses and typically require long-term maintenance with antipsychotic medications. In fact, the relapse rate of patients with first episode schizophrenia within 5 years was 81.9%.65 On the other hand, the remission rate of these patients is relatively low and has been reportedly 23.0–46.4%.60 The Australian study found that the long-term social recovery and symptom remission in patients with first episode psychosis was 23.5%.60 In addition to the maintenance of antipsychotic medications, various psychosocial factors and life-style patterns are also closely associated with long-term clinical outcomes. Therefore, it is important to identify factors related to long-term outcomes in order to reduce the relapse rate and to enhance patient recovery from these disorders. Specifically, the key variables and measures assessed by the KEPS are DUP, early trauma, suicidality, physical health, lifestyle pattern, and cognitive function.
In conclusion, the KEPS is the first cohort study to include comprehensive measures of clinical outcomes and biopsychosocial clinical variables in patients with first episode psychosis in Korea. The identification of factors related to long-term clinical outcomes will provide important information regarding the understanding and management of psychotic disorders. This prospective naturalistic longitudinal study may contribute to the development of early intervention strategies and the improvement of long-term outcomes in Asian patients with schizophrenia.
Acknowledgments
This study was supported by a grant of the Korean Mental Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HM14C2608).
