Prominent Clinical Dimension, Duration of Illness and Treatment Response in Schizophrenia: A Naturalistic Study
Article information
Abstract
Objective
Preliminary data indicate that predominant positive symptoms are predictive of subsequent treatment response, while negative and cognitive symptoms are associated with poor outcome. Purpose of the present study was to investigate the relation between the predominant clinical dimension, duration of illness and acute antipsychotic response in a sample of schizophrenic inpatients.
Methods
Fifty-one schizophrenic inpatients, receiving an antipsychotic mono-therapy, were dimensionally assessed at the admission in the Acute Psychiatric Unit of the University of Milan. Treatment response was selected as parameter of outcome and defined as a reduction >50% of baseline total The Positive and Negative Syndrome Scale (PANSS) score. Demographic and clinical variables between responders and non-responders were compared using one-way analysis of variance for continuous variables and χ2 test for dichotomous ones. Binary logistic regression was performed to find if dimensional scores and duration of illness were associated with acute antipsychotic response.
Results
A longer duration of illness was found in non-responders respect to responders (15.61 years vs. 8.28 years)(F=4.98, p=0.03). Higher scores on PANSS positive sub-scale (OR=1.3, p=0.03), lower scores on cognitive PANSS scores (OR=0.75, p=0.05) and shorter duration of illness (OR=0.93, p=0.04) were found to be predictive of acute antipsychotic response.
Conclusion
These preliminary results show that a long duration of illness as well as a more severe cognitive impairment is predictive of treatment non-response, indicating a worse outcome for chronic patients with predominant cognitive symptoms.
INTRODUCTION
According to the Diagnostic and Statistical Manual for Mental Disorders (DSM) schizophrenia is a categorical condition, markedly separated from the physiological behavior of general population.1 However, in the last years, the evidence of a psychopathological "continuum" between the disorder and the general population,2 the isolation of ultra-risk populations and the multi-factorial etiology of the disorder, supported a dimensional approach. Patients diagnosed as schizophrenics, in fact, show distinct antipsychotic response and social functioning in relation to clinical presentation.3 In line with this approach, in the last years several trials have studied the relation between the predominant symptoms and the antipsychotic response in patients affected by schizophrenia.4-6
The available data indicate that a prevalence of positive symptoms is associated with good response to antipsychotic treatment. A very recent study for example showed as the response to pharmacological treatment is linearly correlated to the severity of positive symptoms.7
Negative symptoms are challenging for clinicians and they are associated with poor outcome.8 Atypical antipsychotics, particularly olanzapine and risperidone, are more efficacious respect to haloperidol in the treatment of negative symptoms.9 In addition recent studies show as aripiprazole may improve negative dimension probably for its partial agonist activity at dopamine D2 receptors.4,10-12 In contrast, the use of antidepressants in augmentation to antipsychotics did not show a clear improvement of negative symptoms.13
The severity of the disorganized dimension is predictive of poor outcome,14 non-response to antipsychotics15 and low quality of life.16 Disorganization and positive symptoms are more responsive to first generation antipsychotics than other symptoms, although recent data show as atypical antipsychotics are superior to typical antipsychotics in the treatment of disorganized symptoms.4
One of the challenges of the long-term treatment of schizophrenia is the cognitive recovery or at least the maintenance of cognitive abilities. Of note, the severity of cognitive deficit is one of the most important predictor of long-term outcome in patients diagnosed with schizophrenia.17 Most of the available data seem to indicate some superiority of the atypical antipsychotics respect to first generation antipsychotics in improving cognitive symptoms of schizophrenic patients.18 However, the size of the cognitive improvement, as well as eventual differences between the single atypical antipsychotics, is still controversial.19
The existence of an independent depressive psychopathological dimension in schizophrenics is still debated as the mood symptoms usually disappear with the improvement of positive/negative symptoms in most of patients.20,21 However, few studies have investigated the relation between depressive symptoms and outcome in schizophrenia.21 The atypical antipsychotics seem to be more effective respect to first generation antipsychotics in treating these symptoms.22
The prevalence of an impulsive-aggressive dimension is strongly associated with suicidal behaviour in schizophrenic patients.23 Several studies show as aggressive behaviour is well controlled by first generation antipsychotics, while impulsivity and suicidal behaviour are better improved by atypical antipsychotics with most of the data about clozapine.24
Finally, several studies have investigated the relation between duration of illness and treatment response in schizophrenia and most of the results show as this variable influences negatively treatment response.25
Purpose of the present study is to find an eventual association between prevalent clinical dimension and antipsychotic response in a sample of schizophrenic inpatients. The possible relation between symptomatic clusters and treatment response has a double interest regarding both for research and clinical purposes.
Concerning research: it could be helpful for assessing more homogenous samples in terms of symptoms and severity of illness; Concerning clinical practice: it should be valuable in order to detect patients requiring targeted pharmacological treatments for preventing poor outcome.
Finally other clinical and demographic variables such as duration of illness and age at onset have been taken into account to investigate the possible relation with acute antipsychotic response.
METHODS
Fifty-one patients hospitalized at the Department of Psychiatry of the University of Milan were included in the study.
Inclusion criteria
-A diagnosis of Schizophrenia according to DSM-IV-TR (Diagnostic and Statistical Manual for Mental Disorders-Text Revision),1
-An acute psychotic episode corresponding to a Positive and Negative Syndrome Scale (PANSS) score >50,26
-The patient had to be drug free for at least two weeks,
-Administration of the same antipsychotic mono-therapy treatment for at least one week that is considered by some authors a reasonable time to evaluate drug response.27
Exclusion criteria
-Comorbidity with mental retardation or other neurological conditions involving Central Nervous System (e.g., cerebral tumors),
-Comorbidity with medical diseases (e.g., hypothyroidism) or dysmetabolisms causing psychiatric symptoms,
-Medical comorbidity influencing the pharmacokinetics of antipsychotics (e.g., renal failure),
-Co-Administration of drugs that can significantly influence the pharmacokinetics of antipsychotics (e.g., antiretrovirals),
-Combined treatment with antidepressants, mood stabilizers, benzodiazepines,
-Pregnancy and breastfeeding.
The design of the study was naturalistic and prospective. All patients admitted at the acute psychiatric unit and fulfilling the DSM-IV-TR diagnostic criteria for schizophrenia (Structured Clinical Interview for DSM-IV Axis I)28 were included in the study. All patients provided a written informed consent for participation to the study and to have the clinical information included in their charts and derived by diagnostic interview reviewed. The Positive and Negative Syndrome Scale (PANSS),29 The Calgary Depression Scale for Schizophrenia (CDSS)30 and the Clinical Global Impression (severity of illness)(CGIs)31 were performed at baseline and each 3 days from the admission.
Of note the different psychopathological dimension were assessed this way:
Positive dimension: positive sub-scale PANSS,
Negative dimension: negative sub-scale PANSS,
Disorganized dimension: sum of the scores of the PANSS items conceptual disorganization (P2), difficulty in abstract thinking (N5), stereotyped thinking (N7), disorientation (G10), poor attention (G11),32
Cognitive dimension: sum of the score of the PANSS items conceptual disorganization (P2), difficulty in abstract thinking (N5), stereotyped thinking (N7), tension (G4), mannerisms and posturing (G5), poor attention (G11), lack of judgment and insight (G12),33
Depressive dimension: CDSS score,
Impulsive-Aggressive dimension: hostility (P7) and poor impulse control (G14) PANSS scores.
Furthermore the global severity (severity dimension) was assessed thorough the CGIs baseline scores.31
Patients that showed a reduction of at least 50% of the baseline PANSS scores after 8 days from baseline were defined as responders.34 Treatment response was selected as an outcome measure.
Descriptive analysis of the whole sample were performed.
The sample was then divided in two groups according to the acute pharmacological response and chi-square tests and one-way analysis of variance (ANOVA) were performed to compare respectively dichotomous and continuous variables between responders and non-responders.
A first binary logistic regression was performed considering psychopathological dimension scores as independent variables and antipsychotic response as dependent one.
A second binary logistic was then performed considering as independent variables age at onset and duration of illness, and antipsychotic response as dependent one.
For all the analyses, the level of statistical significance was set at 0.05 and not corrected. SPSS for Windows (version 18.0) was used as statistical program.
RESULTS
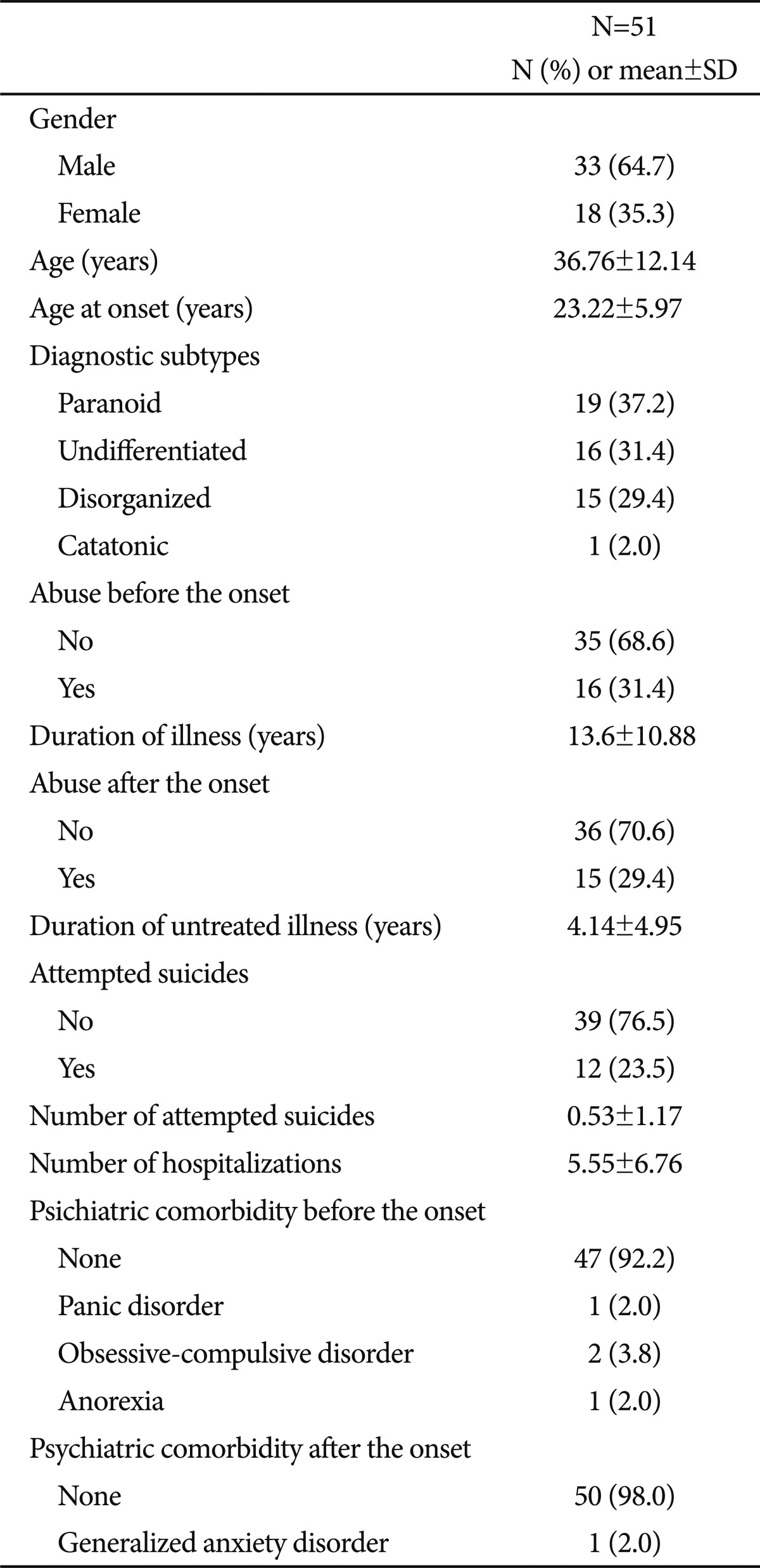
Clinical and demographic variables of the whole sample are described in Table 1.
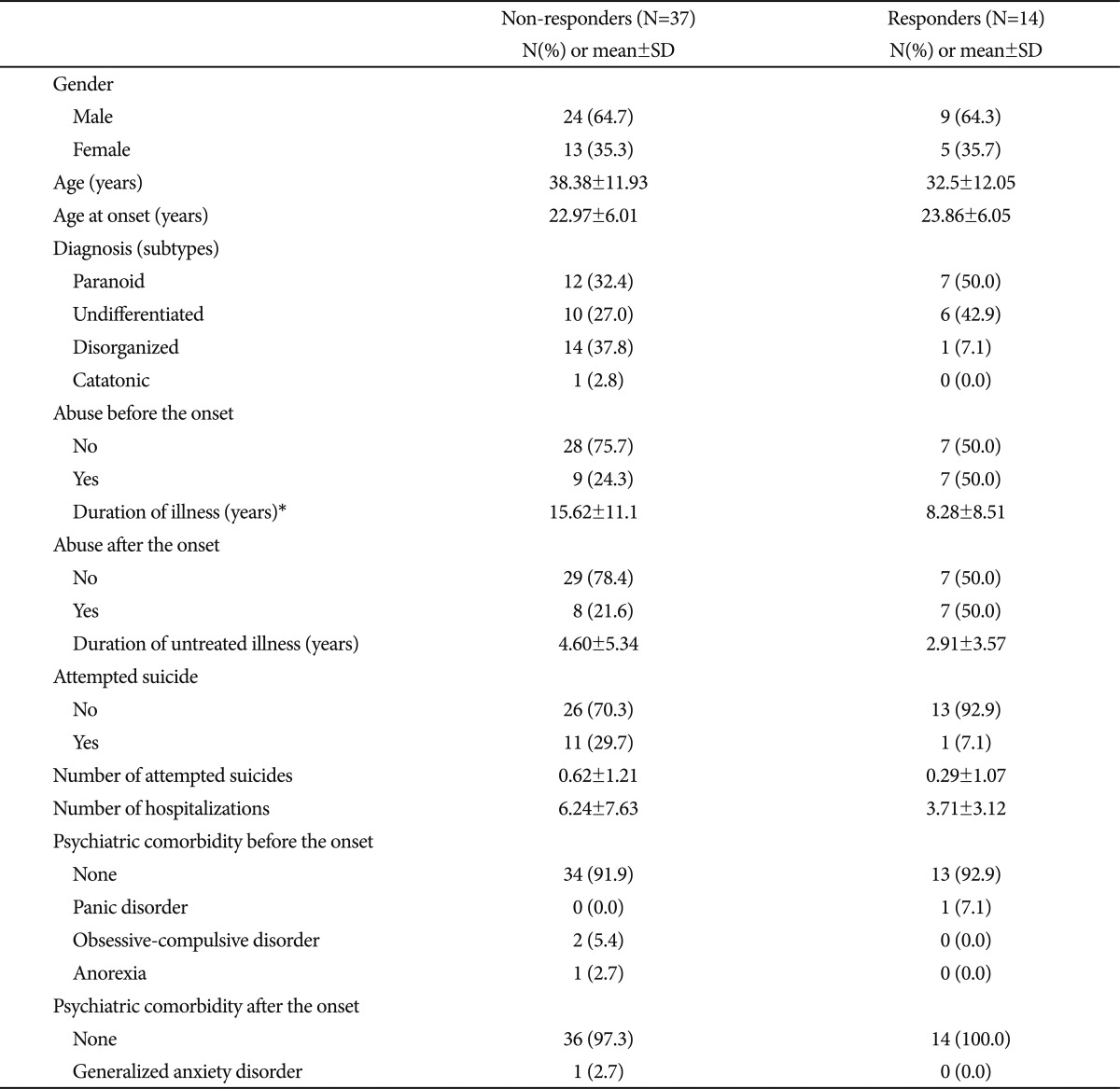
Mean duration of antipsychotic treatment mono-therapy was 12.4 days (±6.4 days). Only 14 patients out of 51 (27.45%) showed a response after 8 days of the prescribed antipsychotic treatment. None of non-responders after 8 days of treatment showed response later to the prescribed antipsychotic mono-therapy. Non-responders did not differ from responders in terms of age (F=2.45, p=0.12), age at onset (F=0.22, p=0.64), number of hospitalizations (F=1.43, p=0.24), number of attempted suicide (F=0.83, p=0.37), duration of untreated illness (F=1.19, p=0.28), duration of hospitalization (F=1.39, p=0.24), duration of antipsychotic treatment mono-therapy (F=2.61, p=0.11) and PANSS baseline scores (F=3.41, p=0.07). In contrast non-responders showed a longer duration of illness respect to responders (15.61 years versus 8.28 years) (F=4.98, p=0.03).
Regarding dichotomous variables non-responders were not different from responders in terms of gender (χ2=0.001, df=1, p=1.00), diagnosis (χ2=5.28, df=3, p=0.14), family history for psychiatric disorders (χ2=7.66, df=7, p=0.38), the presence of abuse before the onset (χ2=3.11, df=1, p=0.10), type of abuse before the onset (χ2=5.31, df=4, p=0.27), the presence of polyabuse before the onset (χ2=0.096, df=1, p=1.00), the presence of abuse after the onset (χ2=3.94, df=1, p=0.08), type of abuse after the onset (χ2=5.95, df=4, p=0.22), the presence of polyabuse after the onset (χ2=4.01, df=1, p=0.07), psychiatric comorbidity before the onset (χ2=3.78, df=3, p=0.36), psychiatric comorbidity after the onset (χ2=0.39, df=1, p=1.00), the presence of previous suicidal attempts (χ2=2.88, df=1, p=0.09), prescribed antipsychotic treatment (χ2=9.87, df=5, p=0.08) (Table 2 and 3).
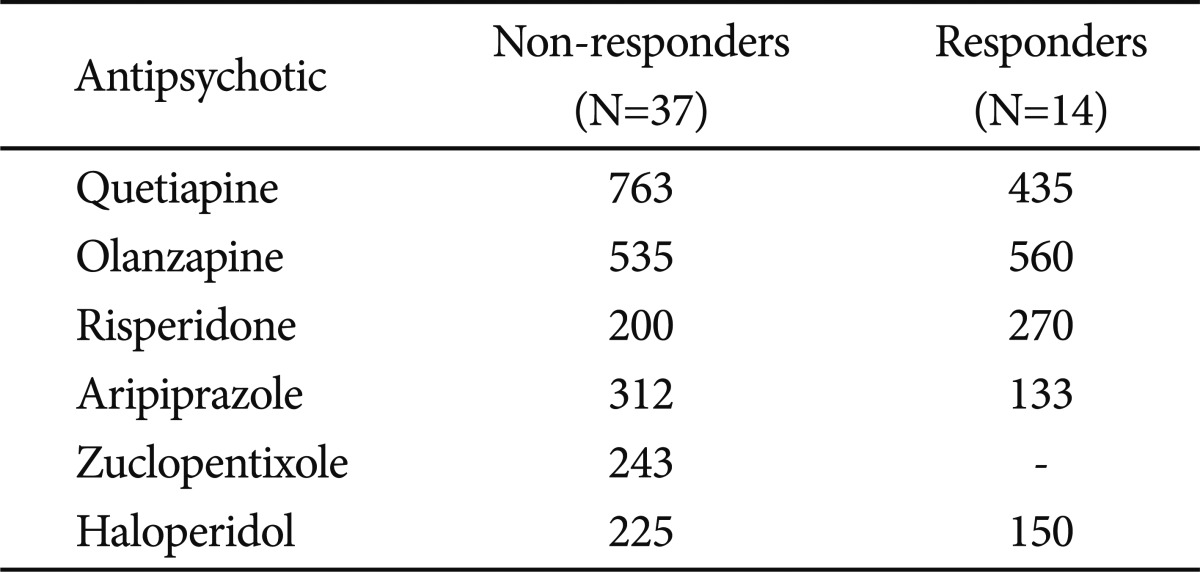
Mean dosages of prescribed antipsychotics in responders and non-responders (chlorpromazine milliequivalents)
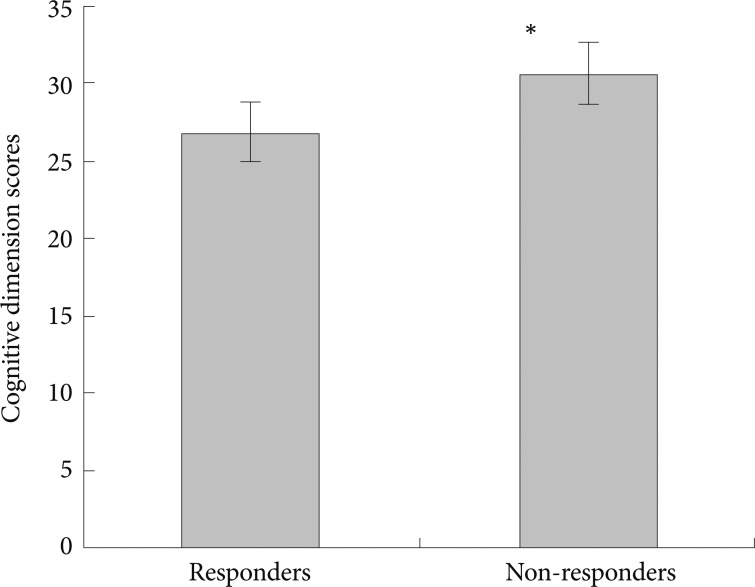
The goodness-of-fit test results (Hosmer and Lemeshow Test: χ2=3.08, df=8, p=0.93) showed that the model including the baseline dimensional scores as possible predictors of response was adequate, allowing for a correct classification of 80.4% of the cases. In addition, the model was overall significant (Omnibus test: χ2=20.65, df=8, p=0.008). Higher scores of dyscognitive dimension (OR=0.75, p=0.05) and CGIs (OR=0.16, p=0.04) were predictive of non-response. In contrast higher scores of positive dimension were predictive of response to antipsychotics (OR=1.23, p=0.028)(Table 4, Figures 1 and 2).
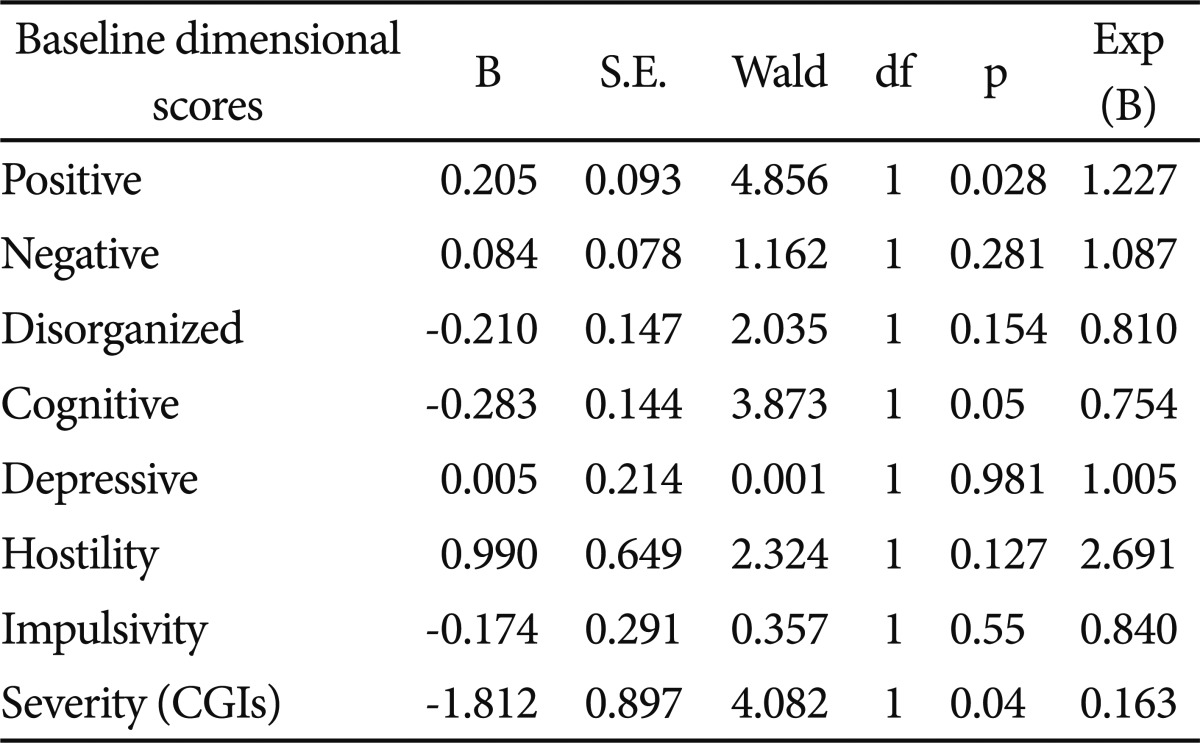
Summary of the statistics for the best-fit logistic regression model applied (baseline dimensional scores)
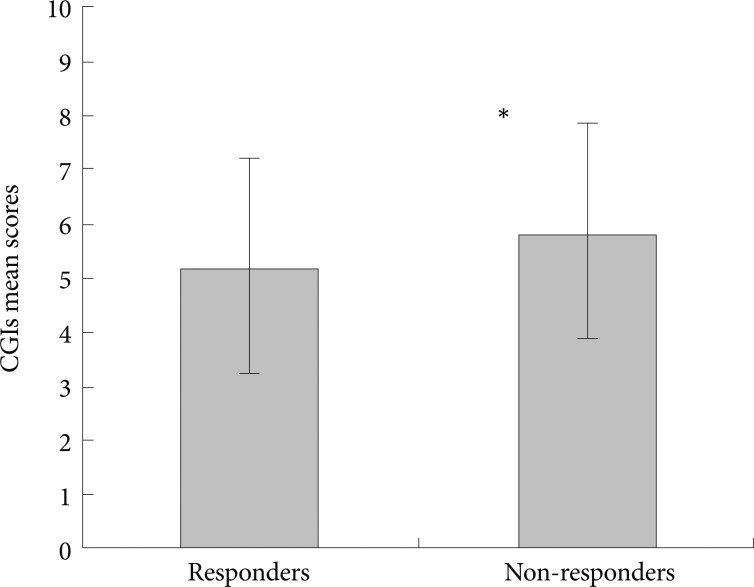
Clinical Global Impression Severity of Illness (CGIs) baseline scores and acute antipsychotic response. *statistics: F=7.34, p=0.009.
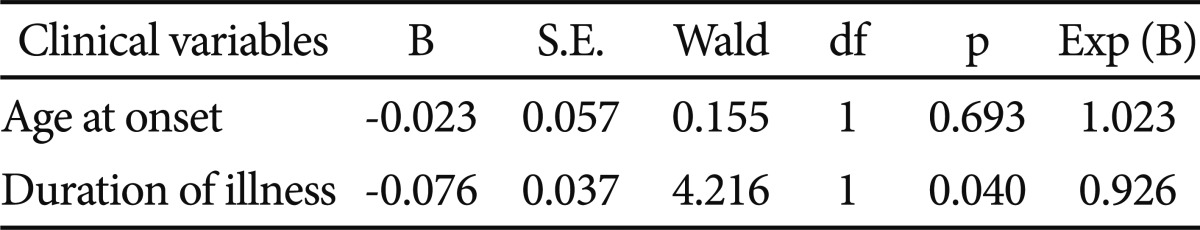
The goodness-of-fit test results (Hosmer and Lemeshow Test: χ2=8.74, df=8, p=0.36) showed that the model including duration of illness and age at onset as possible predictors of antipsychotic response was adequate, allowing for a correct classification of 72.5% of the cases. In addition the model was nearly statistically significant (Omnibus test: χ2=5.40, df=2, p=0.06). A longer duration of illness was found to be predictive of non-response (OR=0.93, p=0.04)(Table 5).
DISCUSSION
The first datum emerging from this study is that only 27.45% of schizophrenic inpatients have a response to antipsychotics in agreement with a relatively recent study.9 Secondly, cognitive impairment and global severity of illness seem to be predictive of lack of response to antipsychotics, while positive dimension would be associated with good acute treatment response. Regarding the possible relation between clinical variables and outcome, duration of illness seems to be predictive of antipsychotic response. Of note patients with long duration of illness seem to be less respondent to acute antipsychotic treatment respect to patients with a short one. Taken as a whole these results show as chronic patients with cognitive impairment are the most challenging for the clinicians, while patients with a short duration of illness and predominant positive symptoms present the best treatment response. In light of these considerations the low rate of response in our sample could be partially explained by the mean long duration of illness of our sample (13.6 years).
Previous studies have already showed as cognitive impairment and long duration of illness are associated with poor outcome,17 while predominant positive symptoms are associated with good prognosis.7 Of note chronic patients with cognitive impairments are likely to show compromised magnetic resonance (MR) images associated with scarce response to antipsychotic treatment.35
Atypical antipsychotics probably prevent the negative effects of duration of illness36 so that primary (recognition and treatment of ultra risk populations) and secondary (early treatment with atypical antipsychotics) prevention strategies could be perhaps the most appropriate strategies to improve outcome of schizophrenic patients.37
The future research should have two main objectives:
1) an accurate evaluation of the impact of a specific symptomatic dimension on the outcome of schizophrenic patients,
2) to investigate the effect of the pharmacological treatment on the biological factors (e.g. neurodegeneration) involved in "resistant" patients with poor response to antipsychotics.38
Finally the predominant symptomatic dimension as a specific predictor of outcome should be introduced in the current diagnostic classifications (DSM and International Classification Disease-ICD).
The limits of the present study have to be shortly described. First the sample size is small and heterogeneous as multiple antipsychotics were prescribed. Of note, the variability of the antipsychotic treatment has to be taken into account although no differences were found between responders and non-responders. Second confounding factors like the time of evaluation of response (8 days from baseline) or the number of previous trials with typical antipsychotics, supposedly affecting negative and cognitive dimensions, are to be taken into consideration. However, as reported in the results none of the non-responders showed response later. In contrast to these limits the study design is naturalistic and prospective with the advantage to be close to the clinical practice. In addition in authors' knowledge no studies have considered all clinical dimensions, including the depressive one, to predict acute treatment response in schizophrenic patients. Studies with larger and homogenous samples are needed to confirm these results.
Acknowledgments
Drs Buoli, Caldiroli and Panza do not have any affiliation with or financial interest in any organization that might pose a conflict of interest with the present article.
Prof. A. Carlo Altamura is:
- Merck consultant,
- Astra Zeneca consultant,
- Sanofi-Aventis speaker bureau,
- Lilly speaker bureau,
- Pfizer speaker bureau.
The paper was funded by TR29 Innovation Programme provided by Lombardy government. The authors express a special appreciation to Lombardy government for the interest and financial support of the present research.