Baduk (the Game of Go) Improved Cognitive Function and Brain Activity in Children with Attention Deficit Hyperactivity Disorder
Article information
Abstract
Objective
Attention deficit hyperactivity disorder (ADHD) symptoms are associated with the deficit in executive functions. Playing Go involves many aspect of cognitive function and we hypothesized that it would be effective for children with ADHD.
Methods
Seventeen drug naïve children with ADHD and seventeen age and sex matched comparison subjects were participated. Participants played Go under the instructor's education for 2 hours/day, 5 days/week. Before and at the end of Go period, clinical symptoms, cognitive functions, and brain EEG were assessed with Dupaul's ADHD scale (ARS), Child depression inventory (CDI), digit span, the Children's Color Trails Test (CCTT), and 8-channel QEEG system (LXE3208, Laxtha Inc., Daejeon, Korea).
Results
There were significant improvements of ARS total score (z=2.93, p<0.01) and inattentive score (z=2.94, p<0.01) in children with ADHD. However, there was no significant change in hyperactivity score (z=1.33, p=0.18). There were improvement of digit total score (z=2.60, p<0.01; z=2.06, p=0.03), digit forward score (z=2.21, p=0.02; z=2.02, p=0.04) in both ADHD and healthy comparisons. In addition, ADHD children showed decreased time of CCTT-2 (z=2.21, p=0.03). The change of theta/beta right of prefrontal cortex during 16 weeks was greater in children with ADHD than in healthy comparisons (F=4.45, p=0.04). The change of right theta/beta in prefrontal cortex has a positive correlation with ARS-inattention score in children with ADHD (r=0.44, p=0.03).
Conclusion
We suggest that playing Go would be effective for children with ADHD by activating hypoarousal prefrontal function and enhancing executive function.
INTRODUCTION
ADHD and executive function
Attention deficit hyperactivity disorder (ADHD) is a common neurodevelopmental disorder in school-aged children, and has a worldwide prevalence rate of 5%.1,2,3 ADHD is characterized by age-inappropriate inattention, hyperactivity, and impulsivity. These symptoms are assumed to result from disturbances in the brain region supporting executive function.4 Executive function is essential for cognitive development and is vital to individual social and intellectual function in daily life. Children with ADHD symptoms often show impairments in executive function, which has a significant impact on academic achievement and social functioning in daily life.5,6 One important neuropsychologic theory suggests that ADHD symptoms arise from a primary deficit in the executive functions that maintain the appropriate problem solving set for the attainment of later goals.7 Executive functions of perceptual cognition in relation to time and space, self-regulation, problem solving, logical and flexible thinking, and reconstitution of behavior have been suggested to be important in ADHD.7,8 Previous studies have also demonstrated that executive function can be enhanced by training intervention in children and adolescents with ADHD.9,10
ADHD treatment and adverse effects
Pharmacological treatment and behavioral interventions have been regarded as the standard treatment for ADHD.11 Stimulant medications are recommended as the first-line treatment for ADHD and can produce improvements in clinical and behavioral symptoms.12,13,14 However, non-pharmacological behavior modification treatments are also recommended for improving behavioral inhibition deficits and executive dysfunction in ADHD.15 For example, neurofeedback therapy, multimodal psychosocial treatment, school-based programs, working memory training, parent training, and self-monitoring have been introduced and applied as alternative treatments.10,16,17,18,19,20 EEG biofeedback, meditation, channel specific perceptual training, and vestibular stimulation have been applied for ADHD as alternative treatment with a promising prospective evidence.20 EMG biofeedback and cerebellar training demonstrated more evidences of treatment effectiveness.20 However, there is still a need for development of further adjuvant methods to improve ADHD symptoms and quality of daily life in children with ADHD.
Board games and executive function
Recent studies have demonstrated that board games involve many aspect of cognitive function. Several neuroimaging studies have revealed that the playing of board games such as Go or chess is related to executive function and problem solving skills.21,22 Chen et al. (2003) investigated the neural basis of Go using functional magnetic resonance imaging and observed enhanced activations in cortical areas of the dorsal prefrontal, parietal, occipital, posterior temporal, and primary somatosensory and motor areas. Quantitative analysis indicated a modest degree of stronger activation in the right parietal area than in the left, which are regions associated with executive function. Tachibana et al.23 investigated the efficacy of a Go intervention program for elementary school children.
The game of Go is a traditional board game for two players that originated in ancient China more than 2,500 years ago. The object of Go is to enclose a lager total area of the board than your opponent. The rules are simple, each player places black or white pieces alternately on the intersections of 19 by 19 crossed lines. The pieces may not be moved once placed on the board, although a player can capture and remove the opponent's pieces. Players must create at least two "eyes" in a group of stones to make them alive. If two eyes are present, the opponent can never capture a group of pieces.24,25 The key factor in playing Go is spatial positioning.
Playing Go requires several cognitive process steps related to executive function: attention, visuospatial perception, working memory, and decision making.26 Playing Go provides good opportunities to develop cognitive skills because of the many creative strategies available within a set of well-defined, simple rules.26 This game is noted for its rich strategy in spite of its simple rules. It was reported that long-term Go training appears to cause structural brain changes associated with higher-order cognitive capacities of learning, abstract reasoning, and self-control.27 Lee et al.27 conducted voxel-based analyses of diffusion-tensor imaging data and found that, compared to inexperienced controls, long-term trained Go players showed larger regions of white matter with increased fractional anisotropy values in the frontal, cingulum, and striato-thalamic areas, which are related to attentional control, working memory, executive regulation, and problem-solving. Additionally, the finding that fractional anisotropy is increased in the inferior temporal regions of expert Go players indicates that these players tend to develop a task specific template and right side dominance, suggesting that the tasks involved are mainly spatial processes.27 Long term Go training may cause structural brain changes associated with many cognitive properties, and such changes might be helpful for improving higher-order cognitive capacities such as learning, abstract reasoning, and self-control, which can facilitate education and cognitive therapies.26,27,28
Executive function and EEG changes in the prefrontal lobe
In a review of quantitative electroencephalography (QEEG) in children with ADHD, elevated theta power, reduced relative alpha and beta power and increased theta/beta ratio have been suggested as a marker of inattention and executive problems in ADHD.29,30,31 QEEG can serve as a valid neurometric tool in the diagnosis of ADHD,32 and changes in QEEG can now be used to evaluate changes in ADHD symptoms correlated with brain activity. Children with ADHD have been shown to have an altered pattern of QEEG activity compared with children without ADHD, especially during attention-loaded tasks, showing increased slow cortical activity mainly over in the frontal areas and decreased fast cortical activity.33 In addition, several stimulants and atomoxetine have been shown to change the EEG patterns in the frontal lobes of children with ADHD.34,35,36,37
We investigated the effectiveness of playing Go as a complementary therapy for improving executive function, including inattention, hyperactivity, and impulsivity, in children with ADHD. We hypothesized that 16 weeks of Go training would change the clinical symptoms of ADHD, cognitive functions and the EEG pattern within prefrontal cortex in patients with ADHD. In details, ARS score and the time of Children's Color Trails Test (CCTT) would be decreased, the total score of digit span would be increased. In addition, theta/beta ratio within prefrontal cortex would be greatly decreased in ADHD group, compared to healthy control subjects.
METHODS
Subjects
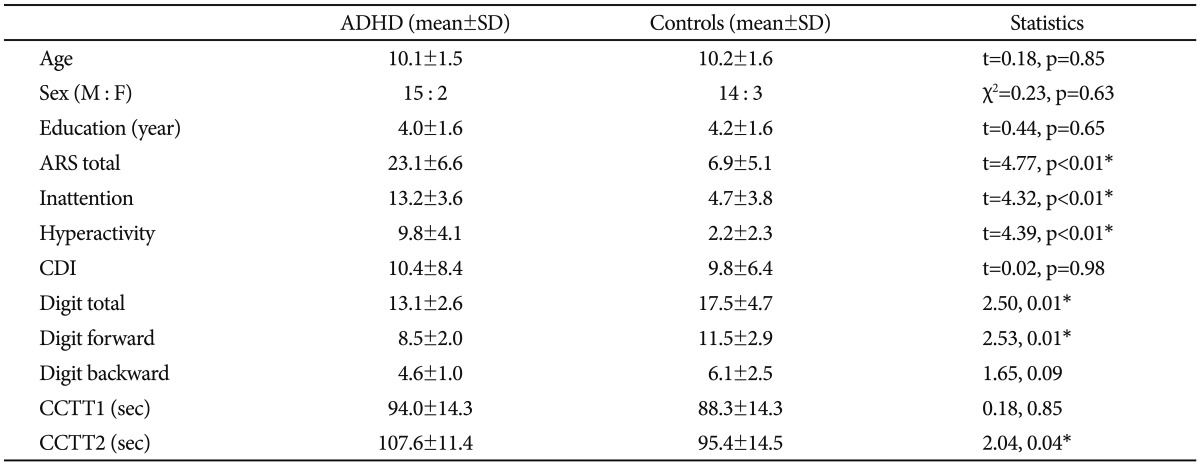
We enrolled the participants by advertising at elementary schools in Andong. After obtaining informed consent from the children and their parents in accordance with Institutional Review Board guidelines, 42 participants were enrolled in this study. Two students with previous experience learning Go, one student with a tic disorder, and five students who dropped out prior to the start of the study were excluded. Seventeen drug-naïve children with ADHD were aged 7 to 12 years and seventeen age- and sex-matched comparison subjects without ADHD were recruited. These participants had no experience of other treatment for ADHD including behavioral therapy and psychosocial treatment. All children were screened with the Korean Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version (K-SADS-PL) by psychiatrist and assessed with the ADHD Rating Scale (ARS).35,36,37,38 The ARS was performed by the parents of each child. There were no differences in the Child Depression Inventory scores between the ADHD and control groups (t=0.02, p=0.98) (Table 1).
The inclusion criteria were as follows: 1) participants had no experience playing Go before the current study, 2) children in the ADHD group were diagnosed by a psychiatrist according to the Diagnostic and Statistical Manual of Mental disorder IV-TR criteria (DSM-IV-TR),37,38,39,40 3) children were able to attend all two hour/day, 5 days/week Go lessons during the 16-week study period. The exclusion criteria were as follows: 1) children who were being treated with stimulants, atomoxetine, neuroleptic, or any other psychoactive drugs or 2) children with organic brain disease, seizure disorder, mental retardation (IQ<70), severe illness or disorder, or other Axis I psychiatric diseases except ADHD, 3) those with any motor or perceptual handicap that would prevent them from playing Go.
Procedures
During the 16 weeks, both ADHD children without medication and children of control group were asked to learn and play Go for two hours/day with an instructor of the game of Go. Before and at the end of 16 weeks of playing Go, clinical symptoms, cognitive functions, and brain QEEG were assessed using ARS, CDI, the digit span forward/backward task, the CCTT, and 8-channel QEEG system (LXE3208, Laxtha Inc., Daejeon, Korea).
The children in the ADHD group had never taken medication for ADHD including stimulants, and had no other treatments for ADHD. The Go training curriculum was designed for beginners aged 7 to 12 and progressed for 16 weeks. Participants played Go under the instructor's education for 2 hours a day during weekday, Monday to Friday. Go training with the same protocol had been provided in two elementary schools and a public library in Andong, Republic of Korea as an after-school activity and the training curriculum was same.
Measures
Recording and analysis of quantitative electroencephalography
Electroencephalographic activity was recorded by QEEG-8 (LXE3208, Laxtha Inc., Daejeon, Korea). The electrodes were placed on Fp1, Fp2, F3, F4, T3, T4, P3, P4 according to the International 10-20 System,41 with two additional electrodes placed on the inter-connected ear lobe to serve as the reference (A2) and ground (A1). The QEEG was recorded with a resolution of 12 bits, a low frequency filter of 0.5, a high frequency filter of 46 Hz, and at a sampling frequency of 256 Hz. Impedance was maintained below 5 kΩ.
All recordings were performed by the same EEG technician. Electroencephalographic activity was recorded with open eyes and during cognitive tasks for 5 minutes, during which participants were asked to judge whether or not pairs of figures were identical. If the pair of figures was identical, participants were asked to press the left arrow key on a computer keyboard, and if the pair of figures was not identical, participants were asked to press the right arrow key. The figures were modified from Raven's Progressive Matrices,42 which is often used as a nonverbal test in educational settings for groups ranging from 5 year olds to people who are elderly. In each test item, the subject is asked to identify the missing element that completes a pattern. This format is designed to measure reasoning ability or components of general intelligence.
Artifact-free 300-second periods were recorded and analyzed. Epochs of movement-related artifacts were excluded from the analyses by direct visual inspection of the raw data. The results were presented as absolute spectral power values (µV2) for individual segments of EEG spectrum theta (4-8 Hz), alpha (8-13 Hz), low beta (12-15 Hz), mid beta (15-20 Hz), and high beta (20-30 Hz). The average power spectrum of the EEG frequencies was calculated by the fast Fourier transform (FFT), a mathematical process that can be used to identify the various frequency bands (delta, theta, alpha and beta) on a QEEG. A Complexity 2.0 (Laxtha, Inc., Daejeon, Korea) EEG analyzing system was used for the analysis of electroencephalographic activity data.
Digit span forward/backwards test
The digit span task in the Wechsler Intelligence Scale for Children requires holding phonological units in the form of digits in short-term memory.43 The examiner reads aloud a sequence of numbers initially three digits in length and continues to nine digits numbers, and the participants are asked to repeat each sequence in the forward order and then in the reverse order. The digit span forward test determines verbal working memory and the digit span backwards test measures complex attention and working memory. Participants' scores were compared to age-matched normative data. Digit span internal consistency (Cronbach's alpha=0.90) and test-retest reliability (r=0.83, p<0.05) were both high.43,44,45
Children's Color Trails Test 1, 2
The CCTT was developed and standardized based on the Trail-Making Test as a Korean version for children.46 The Trail making test, an indicator of the speed of cognitive processing and executive functioning, is the most widely used instrument in neuropsychological assessment. The CCTT consists of two parts: CCTT-1 and CCTT-2. All data are presented as T-scores and are adjusted for age and sex. Higher T-scores indicate better performance on the test. The total time to finish the CCTT-1, CCTT-2 and the difference interference indices have been previously shown to differ significantly between normal children and children with untreated ADHD.47 CCTT-2 reflects primarily working memory, secondary task switching and reflects cognitive flexibility and cognitive persistence.48,49
DuPaul's ADHD Rating Scales
The severity of ADHD symptoms was assessed with the Korean version of the parent and teacher version of DuPaul's ADHD Rating Scale (ARS), which is outlined in the Diagnostic and Statistical Manual of Mental disorders.50 The Korean version of ARS has shown internal consistency (Cronbach's alpha=0.77-0.89) and has been reported to be highly valid and reliable.51 The ARS consists 18 items outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria for diagnosing ADHD, nine of which are inattention (odd numbered) items and nine (even numbered) of which are hyperactive/impulsivity items. Each of the items has a 4-point scale scoring from 0 to 3 points (never or rarely, sometimes, often and very often). The ARS provides a total score, an inattention subscore, and a hyperactive/impulsive subscore. A higher score indicates a greater severity of ADHD. In this study, the ARS was performed by the parents of each child.
Kiddie-Schedule for Affective Disorders and Schizophrenia-Present and Lifetime version-Korean version
The K-SADS-PL is an effective instrument for diagnosing major child psychiatric disorders. The validity and reliability of the Korean version was verified previously.38
Statistical analysis
The differences in demographic characteristics, ADHD symptoms, cognitive function, and QEEG between ADHD group and control group were assessed using the Mann-Whitney U Test. Differences in the changes in ARS total, inattention, hyperactivity and impulsivity, digit span forward/backward, CCTT-2, and QEEG profiles during the 16 week Go training period were analyzed by repeated measures ANOVA. For correction of multiple comparisons, p values were set as less than 0.05/10 for EEG analysis. The effect size (f2) is 0.37 with 0.8 power (1-β). All analyses were performed using SPSS (version 11.0, IBM).
RESULTS
ADHD symptoms
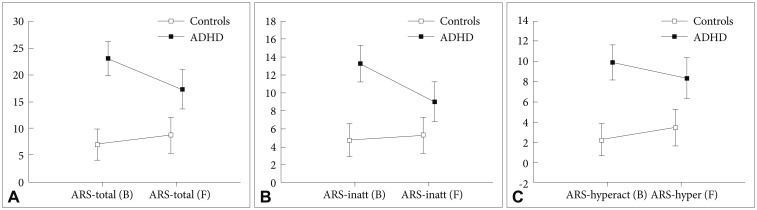
During 16 weeks of learning Go, There were significant difference in the changes of ARS total score (F=23.1, p<0.01) and inattentive subscores of ARS (F=19.4, p<0.01) between ADHD group and healthy control group. In the ADHD group, the ARS total score (z=2.93, p<0.01) and the inattentive subscore of ARS (z=2.94, p<0.01) decreased over the 16-week Go training period (Figure 1). However, the hyperactivity subscore of ARS (z=1.33, p=0.18) did not change. In the control group, there were no changes in the ARS total score (z=1.03, p=0.30), inattentive scores (z=0.27, p=0.79), or hyperactivity scores (z=1.11, p=0.27) during the Go training period.
Quantitative electroencephalography in prefrontal cortex
At baseline, relative high-beta right (Fp2), relative theta right (Fp2), theta/alpha left (Fp1), theta/alpha right (Fp2), theta/beta left (Fp1), and theta/beta right (Fp2) were higher in the ADHD group than in the control group. After 16 weeks of learning Go, the comparison subjects showed increased relative high-beta right (Fp2) (z=2.42, p=0.02), decreased relative theta left (Fp1) (z=2.43, p=0.02), relative theta right (Fp2) (z=2.42, p=0.02), theta/alpha left (Fp1) (z=3.88, p<0.01), theta/alpha right (Fp2) (z=3.88, p<0.01), theta/beta left (Fp1) (z=3.88, p<0.01), and theta/beta right (Fp2) (z=3.88, p<0.01), while children with ADHD showed decreased theta/alpha left (Fp1) (z=3.32, p<0.01), theta/alpha right (Fp2) (z=3.32, p<0.01), theta/beta left (Fp1) (z=3.32, p<0.01), and theta/beta right (Fp2) (z=3.33, p<0.01) (Figure 2). During 16 weeks of learning Go, the change in theta/beta right (Fp2) in children with ADHD was greater than that in children of comparisons (F=4.45, p=0.04) (Table 2). There were no significant different changes in other leads.
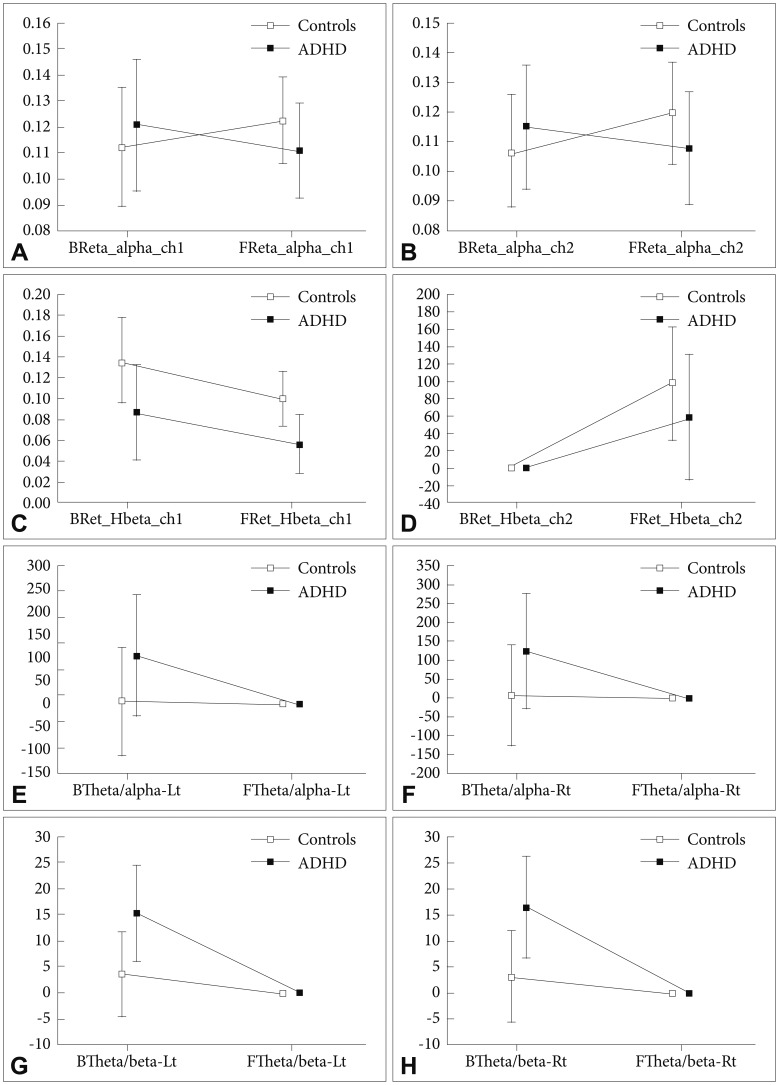
Comparisons of changes in the QEEG profile in the prefrontal cortex between the ADHD and control groups. A: Relative alpha left (Fp1) (F=2.16, p=0.15). B: Relative alpha right (Fp2) (F=2.44, p=0.13). C: Relative high-beta left (Fp1) (F=0.04, p=0.85). D: Relative highbeta right (Fp2) (F=0.54, p=0.47). E: Theta/alpha left (Fp1) (F=1.37, p=0.25). F: Theta/alpha right (Fp2) (F=1.38, p=0.24). G: Theta/beta left (Fp1) (F=3.86, p=0.06). H: Theta/beta right (Fp2) (F=4.45, p=0.04). ADHD: attention deficit hyperactivity disorder, QEEG: quantitative electroencephalography, B: baseline, F: follow up.
Executive function
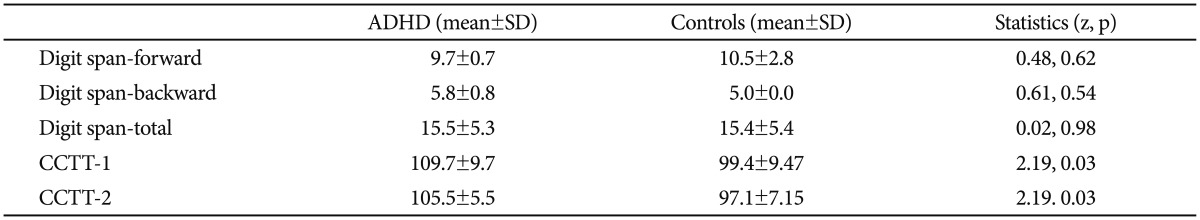
After the 16-week Go training period, the digit span total score (z=2.60, p<0.01) and digit span forward score (z=2.21, p=0.02) had increased in the ADHD group (Figure 3). The digit span backward score (z=1.80, p=0.07) also increased, but the increase was not statistically significant (Figure 3). The control group also showed improved digit span total scores (z=2.06, p=0.03) and digit span forward scores (z=2.02, p=0.04).
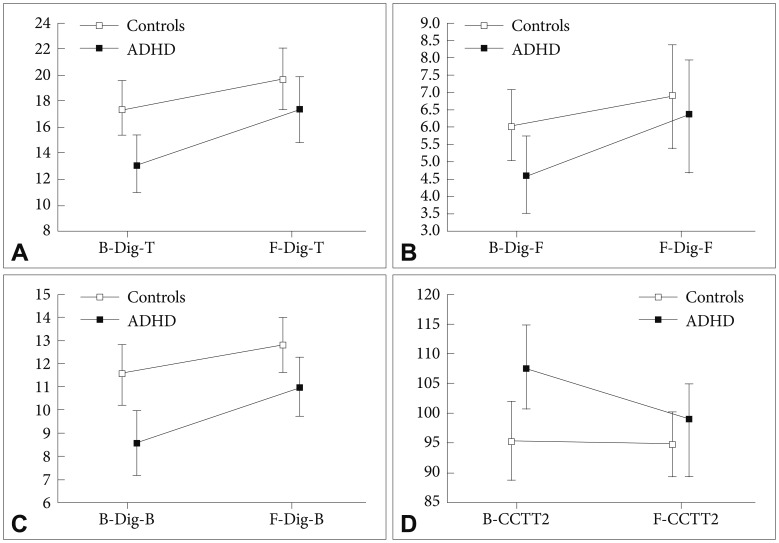
Comparisons of changes in executive function between the ADHD and control groups. Repeated measure ANOVA. A: Digit span total score (Dig-T) [Baseline (B)/Follow up (F)] (F=3.22, p=0.08). B: Digit span forward score (Dig-F) (F=2.08, p=0.16). C: Digit span backward score (Dig-B) (F=1.39, p=0.25). D: Children's Color Trails Test (CCTT) 2 (F=2.53, p=0.12). ADHD: attention deficit hyperactivity disorder, ANOVA: analysis of variance.
ADHD children showed a decrease in CCTT-2 time (z=2.21, p=0.03) after the 16-week Go training period. However, there was no significant change in the comparison group. There were no significant statistical differences in digit total scores (F=3.22, p=0.08), digit forward scores (F=2.08, p=0.16), or digit backward scores (F=1.39, p=0.25) CCTT-2 (F=2.53, p=0.12) between the two groups (Table 3).
Correlations between ARS score, cognitive symptoms, and EEG
The change in right theta/beta (Fp2) had a positive correlation with ARS-inattention scores and a negative correlation with digit span forward scores (r=-0.65, p=0.01) in children with ADHD (r=0.44, p=0.03).
DISCUSSION
Our current results suggested that playing Go may improve attention symptoms, executive function, and EEG changes in the prefrontal cortex in children with ADHD. In addition, changes in attention and executive function are associated with changes in EEG of the prefrontal cortex.
Go improved attention symptoms
We suggest that playing Go is effective for improving inattention in ADHD children. Previous studies have supported the suggestion that Go is effective for inattention. In a brain study of a Go player, a high degree of frontal lobe activation, and more specifically, the lateral prefrontal cortex, was observed. The activation of this area is associated with attention and spatial perception.26 The findings reported by Klingberg et al.10 provided preliminary evidence that visuospatial working memory training has therapeutic effects on ADHD symptoms, including inattention.
Go improved executive functions
The symptom of ADHD significantly correlated with executive functioning such as verbal and spatial working memory, attention shifting, sustained attention, cognitive inhibition, and visuospatial planning.21,26 The results of lower executive function in the ADHD group as compared with the control group as assessed with the digit span forward and the Children's Color Trails Test are in line with what previous studies have shown. ADHD is associated with significant weaknesses in several executive function domains, such as response inhibition, vigilance, working memory and planning.4 Barkely et al. (1997) suggested that ADHD symptoms arise from a primary deficit in executive functions, which are associated with the maintenance of a problem solving set appropriate for attainment of later goals.
After practicing Go for 16 weeks, notable improvements in executive function were observed in the ADHD group. The digit span forward results imply a positive effect on verbal working memory. The results of CCTT indicated improved visuoperceptual abilities (CCTT1) and cognitive flexibility and cognitive persistence (CCTT2),47,48,49 supporting the possible therapeutic effects of playing Go with ADHD children. Adaptive training of working memory (WM) has recently been shown efficacy as an alternative treatment for ADHD.9 It was demonstrated that computerized training of working memory improved response inhibition and reasoning and resulted in a reduction in parent-rated inattentive symptoms in children with ADHD.10
The change of EEG in prefrontal cortex
The theta/beta ratio (Fp1, Fp2) was higher in the ADHD group than in the control group, which is consistent with other studies of QEEG and ADHD.30,31 Various QEEG studies assessing different parameters have been carried out in children with ADHD, and the results have suggested a role for QEEG in evaluating symptom severity and distinguishing ADHD diagnostics.52 In previous studies comparing children with ADHD and children without ADHD, an increase in the delta and theta powers,53 increase in theta and decrease in beta54,55,56 and increase in theta and decrease in alpha and beta57 have been observed, which are characterized as a QEEG profile of ADHD.
Previous studies have shown increased theta activity and decreased beta activity in the prefrontal cortex of children with ADHD during cognitive tasks, indicating hypoarousal in the prefrontal cortex of children with ADHD related to a delay in maturation of cortical function.33 El-Sayed et al. demonstrated that an increase in the theta/beta ratio is a common trait in ADHD. After 16 weeks of learning and playing Go, the change in the theta/beta right in children with ADHD was greater than that in control group (F=4.45, p=0.04). Having more QEEG profile changes in right than the left prefrontal cortex was consistent with results of a previous study that suggested the presence of stronger activation in the right hemisphere than in left while playing Go.26 We suggest that Go training would be effective for ADHD children by activating hypoarousal of the prefrontal functions.
Changes in attention and executive function were associated with changes in the EEG of the prefrontal cortex. This result was consistent with previous studies showing the role of the prefrontal cortex in coordinating, controlling, and executing cognitive processes, allowing for the regulation of attention, impulses, and decision making.58,59
The current study had several limitations. First, the number of subjects was not large enough to generalize the effects of playing Go on children with ADHD. Future studies of a larger number of children will need to be done to conclusively investigate the effects of playing Go. Second, the EEG assessment was focused only on the prefrontal cortex.
To the best of our knowledge, this is the first study investigating the therapeutic effects of playing Go on enhancing cognitive functions in children with ADHD. We suggest that playing Go may be an alternative and complementary therapeutic method and that a modified intervention program for inattention and executive deficit based on the theory of playing Go could be developed.
Acknowledgments
This work was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A120013).