A 12-Week Multi-Domain Lifestyle Modification to Reduce Depressive Symptoms in Older Adults: A Preliminary Report
Article information
Abstract
Objective
The objective of this study was to compare the effectiveness of usual care management (UCM) and a newly-developed lifestyle modification with contingency management (LMCM) for geriatric depressive symptoms in the community.
Methods
A randomized controlled trial was conducted in 93 older adults with major depressive disorder at community mental health centers. A 12 week multi-domain LMCM was developed by providing positive reinforcement using ‘gold medal stickers’ as a symbolic incentive to motivate their participation and adherence. Participants were allocated to LMCM (n=47) and UCM (n=46) groups. They were then subjected to the 12 week treatment. Effects of the two intervention methods on Geriatric Depression Scale were determined using mixed model analysis.
Results
Participants in the LMCM group had greater decline in GDS score per month than participants in the UCM group after adjusting for age, sex, years of education, living alone, and MMSE scores at baseline examination [coefficient for GDS score (95% CI): -1.08 (-1.51, -0.65), p<0.001, reference: UCM group].
Conclusion
LMCM is safe and easy to use with a low cost. LMCM is suitable as psychosocial intervention for older adults with depressive symptoms in the community.
INTRODUCTION
Depression is one of the major causes of disability for the elderly. It accounts for 1.6% of total disability [1]. There are three representative approaches to treat depression: medication, psychological intervention, and lifestyle modification [2-4]. While medication and psychological intervention are first line treatments for depression, lifestyle modification offers a potentially safe and low-cost option. It is especially suitable for elderly populations in the community [4].
Lifestyle modification for managing depression involves the application of environmental, behavioral, and psychological concepts to increase physical and mental wellness [5]. This may involve modification of several domain related to depression, including diet, physical activity, relaxation, recreation, and avoidance of smoking and alcohol [4,6,7]. Especially, scheduling meaningful activities which encourage community engagement and strengthen social relationship is a psychosocial technique that can improve depression [8,9].
However, lifestyle modification in geriatric patients should be considered in the context of easy applicability and effectiveness for the elderly in the community. Motivational issues, time and resources restrictions, and priority issue might have impacts on older adult’s ability to implement lifestyle changes in the community [10]. First, it is necessary to consider readiness to habitual behavior change regarding lifestyle modification [4]. Second, continuous and active engagement is needed when developing and planning of intervention [11]. Third, intervention should be individually tailored. It should offer incentives to improve motivation because lack of motivation is frequently found in older patients with depression [12].
Previously, we have proposed a therapeutic model to change the lifestyle of the elderly by reducing cognitive dysfunction though taking cognizance of factors mentioned above [8]. Based on the previous model, we developed a community-implantable multi-domain lifestyle modification model with contingency management to reduce depression in older adults. The main objective of the present study was to conduct a randomized controlled trial to test the effectiveness, feasibility, and acceptability of this intervention compared to usual care management for older adults with depression in the community.
Methods
Participants
The study was conducted from August 2015 to January 2016 for adults with depression in geriatric community mental health centers located at Suwon and Gwangju, Republic of Korea. The study protocol registered at ClinicalTrial.gov (NCT03095820). These community centers had outreach sites throughout the city’s districts. They provide a range of social, health, educational, and recreational services for the elderly. A total of 93 participants with mean age of 77.8±6.6 years (77.1% females) were recruited through these community agencies. Inclusion criteria for participants were: 1) those with non-psychotic, unipolar MDD DSM-IV diagnosis (Mini-International Neuropsychiatric Interview) [13]; 2) those with Montgomery Asberg Depression Rating Scale (MADRS) score of 17 or higher [14]; and 3) those who were taking antidepressants at stable dosage for at least 6 weeks prior to study entry without any medical recommendation for medication change for the next 3 months. Pharmacotherapy was uncontrolled and provided by community physicians. Exclusion criteria were: 1) those with other Axis I psychiatric disorder; 2) those with acute or severe medical illness (e.g., metastatic cancer, liver failure); 3) those who were taking drugs known to cause depression; 4) those with advanced dementia; and 5) those with aphasia or inability to speak Korean. Subjects used in this study were solely of Asian ethnicity (Korean). The study was approved by the Institutional Review Board of the Ajou University (AJIRB-SBR-SUR-5-132). All participants provided signed informed consent.
Randomization and masking
Randomization was designed in blocks of four participants using SAS. The study coordinator sequentially allocated participants to either usual care management (UCM) or lifestyle modification with contingency management (LMCM). The allocation ratio was 1:1. Raters were independent evaluators who were unaware of randomization status or study hypotheses. Participants were unaware of study hypotheses either.
Therapist training and treatment fidelity
The intervention was carried out by trained health worker in mental health community center. For treatment fidelity, they received training on brief advising process, assessing activity level using a simple self-assessment tool, providing how to increase the activity level, and selecting adequate lifestyle modification goals. A manual was also provided to health workers with systematic introductions. Health workers followed the study’s written protocols when making any intervention-related recommendations.
Intervention
We developed a 12 week multi-domain LMCM. Prize-based contingency management is an approach based on operant conditioning theory [15]. It encourages and maintains desirable behavior change by providing positive reinforcement for recovery of depressive symptoms [15]. Prizes for positive reinforcement in this study were symbolic gold medal stickers to motivate participation and increase sustainability of desirable behavior for depression [8]. Although the most commonly used incentives have been financial, we have developed a symbolic incentive that is simple. It can be easily and widely provided in the community.
Based on SIGN guidelines for non-pharmaceutical management of depression, the following four lifestyle factors related to geriatric depressive symptoms were managed: physical activity, healthy diet, social activity, and emotional regulation [4,16]. Lifestyle modification message included information on deleterious effects of geriatric depression and the importance of engaging in moderate physical activity, maintaining healthy diet, social activity, and emotional regulation to prevent it. Through detailed initial interviews with participants, simple individual goals of prize-based contingency management for each element were set. For example, physical activity goals involved encouraging participants to perform at least 30 min of moderate physical activity 3 times per week. The most frequently recommended type of activity was walking. Healthydiet recommendation consisted of encouraging participants to consume high quantity of fruit and vegetables, control their weight, have intake of fish or meat at least twice a week, and so on. To encourage social activity, participants were provided with information about the value of an active life style from the perspective of social connectedness and taking part in available recreational community services for the elderly. Emotional regulation management consisted of relaxation and recreation to improve mood and balance work-rest-play dynamic. Relaxation and recreational activities provided opportunity to direct their mind away from rumination and worry. To maintain the motivation of participants, prize-based contingency management was applied for each lifestyle modification goal. Once a week of telephone-check and once a month of visitcheck were provided to each participant during the follow-up period of 12 weeks. Evaluations were conducted at baseline and at each visit.
UCM was used as a control condition [17,18]. UCM was a telephone (once a week) and home-delivered (once a month) supportive psychotherapy administered in 12 weekly sessions focusing on non-specific therapeutic factors such as facilitating expression of effect, conveying empathy, and imparting optimism. To parallel the delivery of LMCM, community health worker provided UCM to participants in a conventional manner.
Measurements
Two clinicians (investigators) agreed on the diagnosis after reviewing SCID-R and other ratings. Certified raters performed in-home assessments at study entry (baseline) and at 4, 8, and 12 weeks of the study period. Depressive symptoms in the elderly were assessed using the Korean version of the Geriatric Depression Scale (GDS)-Short Form [19]. It was a self-report assessment validated for use in elderly Korean subjects. The questionnaire consisted of 15 Yes/No questions related to depression. A cut-off point of 8 exhibiting a sensitivity of 85% and a specificity of 69% for diagnosing a major depressive episode as compared to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition-Text Revision (DSM-IV-TR) [19] was used in this study. This evaluation for self-rated depression using GDS was confirmed by trained health worker in mental health community center.
Questionnaires were conducted at baseline to evaluate the following: 1) demographic characteristics (including age, sex, and years of education); 2) medical illness; and 3) cognitive burden (including scores of the Korean version of the Mini-Mental State Examination-MMSE [20]).
Sample size determination
Based on a between treatment effect size of 0.70 for depression and disability, we predicted that with at least 36 participants per group and 13% attrition rate, we would have at least 0.80 power at 0.05 two-tailed significance level with ICC=0.40.
Statistical analyses
Descriptive statistics were used to estimate frequencies, means, and standard deviations of collected variables. Independent group’s t-test was used to analyze continuous variables while chi-square test was used to analyze categorical variables. Mixed-effects linear regression analyses (LMM) and repeated measure of ANOVA were used to compare GDS scores (baseline and at 4, 8, and 12 weeks) between UCM and LMCM groups. The model included a random intercept fixed effect for intervention, time, and interventions by time interactions. Age, gender, years of education, living alone, and cognitive function were included as covariates in the model. Missing GDS values were imputed with fitted values derived from regression models following the intent to treat principle. p-values of less than 0.05 were considered statistically significant. All statistical analysis were performed using Predictive Analytics Software (PASW) version 22.0 (SPSS Inc., Chicago, IL, USA).
Results
Participants characteristics
A total of 125 individuals were screened and 93 were found to be eligible. They were randomized to UCM (n=46) vs. LMCM (n=47) groups for 3 monthly sessions (Figure 1). Of these 93 participants, 12 (12.9%) were males and 81 (87.1%) were females. The mean age of these participants was 77.8±6.6 years. The mean number for years of education was 4.4±3.9 years. Their average MMSE score was 23.2±3.7, which was higher than the cutoff for potential dementia (cut-off value of 17 to 18). Baseline demographic and clinical characteristics of these 93 participants are summarized in Table 1. In baseline examination, there was no significant difference in age, sex, years of education, living alone, cognitive function, or baseline GDS score between subjects who were receiving UCM and those who were receiving LMCM (Table 1). All participants in UCM and LMCM groups were depressed according to cut off point of GDS score (at 8). Of these 93 participants randomized, 88 (94.6%) completed the evaluation (UCM, 44 of 46, 95.7%; LMCM, 44 of 47, 93.5%). There was no significant difference in demographics, cognitive function, and depressive symptoms between subjects who dropped out and those who completed assessments.
Change in depressive symptoms between two interventions
As shown in Figure 2, the UCM group showed a 1.93-point decline in GDS score while the LMCM group had a 4.98-point decline in GDS score during the 12 weeks of intervention. Improvement in depressive symptoms from baseline to the end of 3-month session was higher in the LMCM group compared to that in the UCM group (repeated measure of ANOVA: F=19.43, p<0.001 between UCM and LMCM groups). Moreover, differences in GDS scores between UCM and LMCM group were prominent only at 12 weeks among the four assessment time points of the study (UCM: 10.2±3.6, LMCM: 7.5±4.1, t=3.45, p=0.001 at 12 weeks), although depressive symptoms reduction was observed in both intervention groups by the end of the study. When GDS scores of subjects were categorized into two groups (normal, GDS score of 0–7; depressed, GDS score of 8 or higher), remission rate of geriatric depression was 19.6% (9/46) in the UCM group and 46.8% (22/47) in the LMCM group. Difference in the remission rate between the two intervention groups was statistically significant (χ2=7.76, df=1, p=0.005).
Change of geriatric depressive symptoms according to interventions. UCM: Usual Care Management, LMCM: Lifestyle Modification with Contingency Management.
In mixed-effects model consisting of intervention group, time, and intervention group by time interaction as fixed effects with intercept and slope as random effects, significant differences in the decline of GDS score were also observed by the end of the study. Participants in the LMCM group had greater decline (by approximately 1.08 in GDS scores per month) than participants in the UCM group after adjusting for age, sex, years of education, living alone, and MMSE scores at baseline examination [coefficient for GDS score (95% CI): -1.08 (-1.51, -0.65), p<0.001, reference: UCM group] (Table 2).
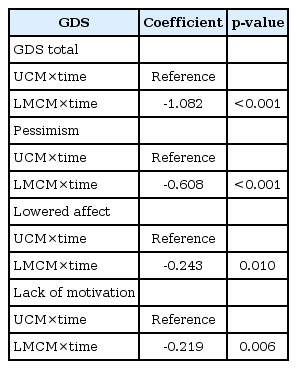
Regression coefficients in the mixed effect models for total and subtotal of GDS score influenced by UCM and LMCM
In addition to total GDS score, effects of the two intervention methods on subscale of GDS (pessimism, lowered affect, and lack of motivation) were also examined. In mixed model analysis, pessimism, lowered effect, and lack of motivation subscales of GDS had greater improvement in the LMCM group compared to those in the UCM group [coefficient for subscale of GDS (95% CI), pessimism: -0.61 (-0.85, -0.37), p<0.001; lowered affect: -0.24 (-0.43, -0.06), p=0.01; lack of motivation: -0.22 (-0.37, -0.06), p=0.01].
Discussion
The main finding of this study was that health worker-initiated psychosocial intervention with symbolic rewards was superior to primary health worker offered-usual care management for geriatric depressive symptoms in the community. By the end of the study, the remission rate in the LMCM group was approximately 2.4 times higher than that in the UCM group. These results were unchanged after adjusting for demographic factors and quantitative measure of general cognitive function. Moreover, the tendency of gradual decrease in depressive symptoms over time in the LMCM group was maintained at 12 weeks, while such decrease was not maintained in the UCM group at 12 weeks.
The effect of community-based usual care management on elderly patients with depression has been reported in previous studies [21,22]. Most community based care management for older adults consisted of providing health care-related information, connecting to mental health care service system, and providing psychoeducation and supportive psychotherapy [23]. However, our approach had an emphasis on symbolic incentives as well as mental health to promote lifestyle modificationrelated psychotherapy, thus improving geriatric depressive symptoms. Simple counseling by only advising elderly patients about their mental health is difficult to change their behaviors. It might increase resistance to change their depressive symptoms due to their lack of motivation [9,24,25]. Supportive and continuous encouragement from primary health workers with contingency management using symbolic incentives might increase their engagement in lifestyle modification [9]. Our specific technique consisted of specific goal-setting, prompting self-monitoring, providing feedback on performance, and goal reviewing to increase their engagement. It might lead to meaningful change of behavior and reduction of their geriatric depressive symptoms [26]. In particular, regular and continuous contacts and attention with symbolic incentives provided by therapists might help decrease their social isolation, a crucial psychodynamic for occurrence of depression in the community dwelling elderly [27,28]. In addition, results of GDS subscales revealed that this approach could stimulate the lack of motivation in patients with depression in the community.
Our study has some limitations. First, the stability of the effect on geriatric depressive symptoms of LMCM compared to UCM after 12 weeks was unclear. To prove the superiority of sustainability of LMCM over that of UCM, future investigation with a longer examination period is needed. Second, inter-group heterogeneity such as preclinical Alzheimer’s disease might have been undetected. Depressive symptoms in subjects might reflect the presence of preclinical Alzheimer’s disease. To have a more homogeneous population set in our study, we only included patients over 60 years old with MMSE scores equal or greater than 24 who were cognitively intact. Third, since subjects who participated in this study were enrolled after seeking medical attention in senior citizen centers, results of this study may not reflect the general population. Finally, we did not include factors such as duration of depressive episodes or the rate of relapse/recurrence during treatment. Inclusion of these variables might alter our findings.
In summary, this study demonstrated the effectiveness of lifestyle modification with symbolic incentives in improving geriatric depressive symptoms in older adults in the community. This psychosocial intervention with symbolic incentives might be useful for the elderly who are at risk of having adverse reactions to drugs or with limited response to usual care management in community dwelling older adults. The LMCM is safe and easy to use with a low cost. It can increase social connectedness through continuous attention provided by health workers. It is suitable for older adults with depression in the community. Our results demonstrate that effective psychosocial intervention is important in managing late life depression in older adults in the community.
Acknowledgements
This study was supported by a grant (HI15C1032) funded by a R&D Project of Korea Mental Health Technology.