Decreased IL-1ra and NCAM-1/CD56 Serum Levels in Unmedicated Patients with Schizophrenia Before and After Antipsychotic Treatment
Article information
Abstract
Objective
Schizophrenia (SZ) has been associated with the inflammatory-related and immunological pathogenesis. This study investigates the aberration of cytokines in patients with SZ.
Methods
Thirty patients with SZ without antipsychotic treatment for at least two weeks participated. We measured the serum levels of fourteen cytokines at hospital admission and after 8-week antipsychotic treatment. Severity was measured by expanded version of 24-items brief psychiatric rating scale (BPRS-E). Repeated measure analyses of variance were conducted.
Results
The interleukin-1 receptor antagonist (IL-1ra) was significantly decreased after 8-week antipsychotic treatment than those of before antipsychotic treatment (F=12.15, df=1/30, p=0.002). Neural cell adhesion molecule 1/CD56 (NCAM-1/CD56) was significantly decreased (F=6.61, df=1/30, p=0.016) among those with second-generation antipsychotics but not first-generation antipsychotics treatment. The changes of BPRS-E-manic and BPRS-E-anxiety scores correlated with the baseline IL-1ra (r=-0.393), IL-6 (r=-0.407), and insulin like growth factor binding protein 3 (r=-0.446). Additionally, the changes of BPRS-E and BPRS-E-negative scores correlated with the changes of brain-derived neurotrophic factor (r=0.372) and interferon-gamma (r=0.375).
Conclusion
Our study supports that IL-1ra and NCAM-1/CD56 may be considered as markers of developing SZ.
INTRODUCTION
Schizophrenia (SZ) is a severe and chronic psychiatric disorder that affects approximately 0.30% to 0.66% cases per 10,000 person-years [1]. SZ results in great patient suffering and socio-economic burden [2], and it is one of the world’s top 10 causes of long-term disability within the categories of sociooccupational functioning and self-care [3]. Although researchers have worked diligently to find treatment strategies, SZ continues to be one of the most debilitating psychotic disorders due to the lack of effective treatments [3]. This may be due to our poor understanding of the etiology of SZ. In addition to well-established findings of some mechanisms, such as dopaminergic and glutamatergic pathways [4], that contribute to the development of SZ, studies have indicated that the alternation of the immune-inflammatory cytokines that are produced by Th1 and Th2 cells might play a role [5]. However, the findings of these studies have been inconsistent. A systemic review reported that patients with SZ have increased serum levels of the interleukin (IL)-1 receptor antagonist (IL-1ra), soluble IL-2 receptor (sIL-2R), and IL-6 and decreased levels of IL-2 [5]. A meta-analysis showed that drug-naïve patients experiencing their first episode of psychosis have significantly increased levels of pro-inflammatory cytokines, such as IL-1β, sIL-2R, IL-6, and tumor necrosis factor (TNF)-α, and non-significant effect size estimates were obtained for IL-2, IL-4, and interferon (IFN)-γ [6].
In addition to inflammatory cytokines, researchers have become interested in neurotrophic factors. Because SZ is considered a neurodevelopmental disorder [7], several growth factors have recently been investigated in SZ-related research, and increasing evidence suggests that they are involved in the pathogenesis of SZ. Brain-derived neurotrophic factor (BDNF), which is one of the most abundant factors in the growth factor family, is involved in neurodevelopment, neuronal survival and differentiation, and synaptic plasticity [7]. Although several studies have examined BDNF levels in patients with SZ, the findings have been contradictory. The severity of psychosis in patients with SZ has been reported to be negatively correlated with BDNF levels [8]. However, this finding was not replicated in a subsequent study [9]. Glial cell-derived neurotrophic factor (GDNF), which is a member of the transforming growth factor (TGF)-β family, is a potent neurotrophic factor for dopaminergic neurons [10]. After antipsychotic treatment, GDNF levels have been shown to increase while psychotic symptoms decrease in patients with SZ [10]. However, another study demonstrated that the serum levels of GDNF did not differ between patients with SZ and healthy controls [11]. Other studies have investigated the interactions between SZ and other growth factors, such as nerve growth factor (NGF) [12] and insulin-like growth factor (IGF-1) [13]. However, the involvement of growth factors in SZ is poorly understood and inconclusive.
To date, SZ is a disorder that is clinically diagnosed using the Diagnostic and Statistical Manual of Mental Disorder, 5th edition (DSM-5) [14]. Precise biomarkers are helpful for clinicians for differential diagnoses and for researchers to for the development of newer psychotropic agents. The results of the studies discussed above suggest that the association of changes in cytokines and the severity of psychosis in patients with SZ are still controversial. Furthermore, few studies have performed repeated measurements of multiple cytokines between preand post-treatment in subjects with SZ. Given these aforementioned gaps within the literature, we conducted a prospective study to investigate the relationship between cytokine levels and the severity of SZ. We aimed to assess a variety of cytokines before and after treatment and compare them in multiple groups in a naturalistic setting without a control group.
METHODS
Participants
Thirty patients from a medical center in Southern Taiwan who were admitted from August 2014 to August 2015 were enrolled in the present study. All patients met the diagnostic criteria for SZ according to DSM-5 [14]. The patients were unmedicated for a minimum of two weeks before enrollment. We excluded patients 1) with mental retardation, neurocognitive disorders, major depressive disorder, bipolar I or II disorder, or substance dependence or 2) who could not provide informed consent. All patients were admitted to the acute psychiatric ward and followed and treated for eight weeks with antipsychotics. This study was approved by the Ethics Committee of Kaohsiung Veterans General Hospital (VGHKS13-CT5-08).
Instruments and pharmachotherapy
The Brief Psychiatric Rating Scale (BPRS), which is one of the most frequently used screening tools, is used to quickly assess psychopathology in various psychiatric disorders. The original BPRS, which consists of 16 item, was developed in 1962 [15]. It was later extended to 18 items. More recently, the expanded 24-items BPRS (BPRS-E) was developed to increase the instrument’s sensitivity to psychotic and affective disorders [16]. The BPRS-E was administered to 30 patients before and after the eight weeks of treatment with antipsychotics, which was supervised by a psychiatrist (CLL) [16]. Four conceptual domains (manic excitement/disorganization, depression/anxiety, negative symptoms, and positive symptoms) were considered in a subanalysis in the present study [17]. The presence and severity of psychiatric symptoms were rated from 1 (not present) to 7 (extremely severe). The total scores varied from 24 to 168, with higher scores denoting more severe psychopathology.
During the eight-week follow-up period, the classification and dosage of the antipsychotic agents were flexibly adjusted according to the clinical judgment of the treating psychiatrists. Drug adherence was monitored and ensured by psychiatric nurses.
Bioassay
Venous blood (5 mL) was collected between 7:00 and 8:00 AM to avoid circadian fluctuations of the measured cytokines. After centrifugation at 3,000 rpm for 10 min, the serum was separated from the blood and stored at -70°C prior to the assay. The serum levels of the following 14 cytokines were examined in the present study: IFN-γ, IL-1β, IL-1ra, IL-2, IL-6, IL-8, IL-10, IGF binding protein 1 (IGFBP-1), IGFBP-2, IGFBP-3, BDNF, GDNF, NGF-β, and neural cell adhesion molecule 1/CD56 (NCAM1/CD56). These cytokines were measured using sandwich enzyme-linked immunosorbent assay kits (R&D Systems, Inc., Minneapolis, MN, USA) according to the manufacturer’s protocol. All experiments were performed in duplicate. The intra- and inter-assay variations were less than 10%. The blood of all patients was assayed at admission baseline (week 0) and after antipsychotic treatment (week 8).
Statistical analysis
The data for the patient demographics and clinical characteristics are presented as mean±standard deviation for continuous variables and percentages for categorical variables. The primary analysis examined the effects of the eight weeks of antipsychotic treatment on the cytokines levels. Additionally, because second-generation antipsychotics (SGAs) have different binding profiles and mechanisms of action compared with first-generation antipsychotics (FGAs), we examined if the effects of SGAs differed from those of FGAs on cytokine levels [8]. Therefore, we used a repeated-measure analysis of variance (ANOVA) to examine the effects of effects of treatment (time) and time×the different classes of antipsychotics (FGAs vs. SGAs) as the within-subject contrast. The secondary analyses examined the correlations between the cytokine levels and the BPRS-E scores with Spearman correlation (e.g., between baseline cytokine levels and the mean changes of cytokines and the BPRS-E-total and BPRS-E-subscales scores before and after antipsychotic treatment). All statistical analyses were conducted using SPSS 19.0 (IBM Corp., Armonk, NY, USA) and differences were considered statistically significant when p values were less than 0.05.
RESULTS
Characteristics of the sample
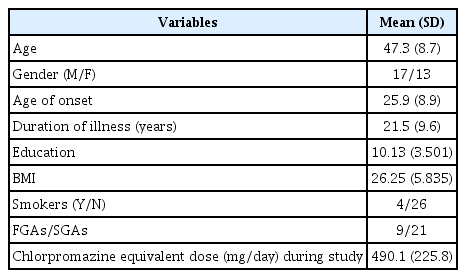
Table 1 lists the sociodemographic and clinical data of the unmedicated patients with SZ. The subjects consisted of 17 men (56.7%) and 13 women (43.3%). All patients were unmedicated for at least two weeks before enrollment. Table 1 presents the data on age, age of illness onset, duration of illness, gender, education, body mass index, smoking, and class of antipsychotics (FGAs vs. SGAs). The mean age, age at illness onset, disease duration of the recruited patients, and mean chlorpromazine equivalent dose (mg/day) were 47.3±8.7, 25.9±8.9, 21.5±9.6 years old, and 490.1±225.8 mg/day, respectively. In addition, 21 out of the 30 patients (70%) were treated with SGAs.
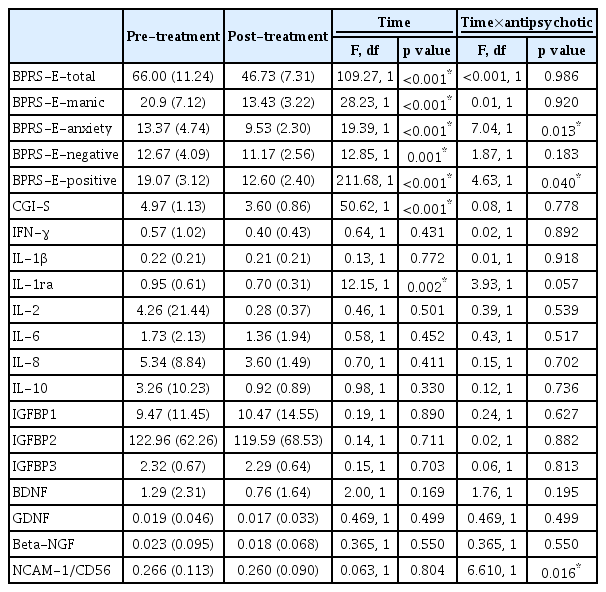
Effects of antipsychotic treatment on the psychopathology and serum cytokine levels
Table 2 shows the comparisons of the pre- and post-treatment psychopathology and cytokine data with the factor of time×antipsychotic class interaction, which were analyzed with repeated-measures ANOVA. Eight weeks of antipsychotic treatment resulted in significant decreases in the BPRSE-total, BPRS-E-manic, BPRS-E-anxiety, BPRS-E-negative, and BPRS-E-positive subscales and Clinical Global Impression-Severity (CGI-S). The levels of only one (IL-1ra) of 14 cytokines decreased significantly after antipsychotic treatment compared with before antipsychotic treatment (F=12.15, df=1/30, p=0.002). Additionally, a repeated-measures ANOVA showed significant interactions between time×antipsychotic class for the BPRS-E-anxiety (F=7.04, df=1/30, p=0.013) and BPRS-E-positive (F=4.63, df=1/30, p=0.040) subscales and NCAM-1/CD56 (F=6.61, df=1/30, p=0.016), with a trend towards an interactions for IL-1ra (F=3.93, df=1/30, p=0.057).
Correlation of the baseline and cytokine level changes and BPRS-E scores after eight weeks of antipsychotic treatment
Table 3 shows that the changes in the BPRS-E-manic and BPRS-E-anxiety scores after treatment correlated with the baseline levels of IL-1ra (r=-0.393, p=0.032), IL-6 (r=-0.407, p=0.025), and IGFBP3 (r=-0.446, p=0.014). Additionally, the changes in the BPRS-E and BPRS-E-negative scores correlated with the changes in the levels of BDNF (r=0.372, p=0.043) and IFN-γ (r=0.375, p=0.041), respectively. For the baseline psychopathology and changes in the levels of serum cytokines after eight weeks of treatment, the baseline BPRS scores correlated with the changes in the levels of IFN-γ (r=-0.424, p=0.02), IL-2 (r=-0.428, p=0.018), and BDNF (r=-0.602, p<0.001) (data not shown).
DISCUSSION
Although several studies have reported an association between cytokine levels and SZ, our study compared the levels of multiple cytokines in patients with SZ before and after antipsychotic treatment. Together with the BPRS-E assessment of severity, we examined cytokines among the multiple domains of inflammatory factors, neurotrophic factors, growth factors, and immunoacting factors. One of the main findings in our study was that IL-1ra levels were significantly decreased after the eight-week antipsychotic treatment, which was similar to previous report [18]. IL-1ra, which is a member of the IL-1 family and which is secreted by immune cells, acts as an inhibitor of the pro-inflammatory effects of IL-1β [19]. Cytokine actions can also be inhibited by naturally occurring cytokine receptor antagonists, such as the IL-1ra, which competes with the physiologic ligand to bind to membrane IL-1 receptors. IL-1ra is produced in response to several inflammatory stimuli, including IL-1 and IL-6, and its levels increase in a variety of infections and inflammatory diseases [19]. Another study has indicated that chronic low-grade systemic inflammation may lead to a two- to three-fold increase in the systemic concentrations of variable cytokines, including IL-1ra [20]. Our IL-1ra results support the involvement of an immune-inflammatory mechanism in SZ [5]. However, the results for the other inflammatory factors, including IFN-γ, IL-1β, IL-2, IL-6, IL-8, and IL-10, indicated an insignificant trend of a decrease after treatment. Although several studies have explored the relationship between psychosis severity and changes in inflammatory factors, the results are inconclusive. A 28-day aripiprazole trial of chronic patients with SZ has shown a significant reduction in the levels of IL-1β, IL-6, TNF-α, IL-1ra, IL-4, and IFN-γ and a significant increase in the levels of IL-10 [21]. Another study on drug-naïve first-episode psychosis has indicated that the levels of IL-6, IL-10, TNF-α, and IL-4 decreased significantly after risperidone treatment [22]. However, a threemonth follow-up study of patients with SZ showed no significant differences in the levels of IL-2, IL-4, and IFN-γ after risperidone was prescribed [23]. Specifically, we analyzed the correlation between the changes in severity on the BPRS-E and cytokine levels. The changes in psychotic severity were significantly associated with the baseline IL-6 levels and changes in the levels of IFN-γ. Moreover, baseline severity correlated with the changes in the levels of IFN-γ and IL-2. A previous study reported similar results: the baseline psychotic severity correlated with the baseline levels of IL-6 [24]. Future studies with well-controlled participants may help to clarify the detailed mechanisms.
Another main result was that the levels of NCAM-1/CD56 were significantly decreased in the patients with SZ who were treated with SGAs but not FGAs. However, the differences in the levels of NCAM-1/CD56 were not significant regardless of the type of antipsychotic. NCAM-1, which is also known as CD56, is a member of the immunoglobulin superfamily, which is often considered a marker of neural lineage commitment and which is associated with natural killer cells [25]. Previous studies have investigated the relationship between SZ and immunological alterations in lymphocytes, and no significant associations were found for NCAM-1/CD56 [26,27]. A meta-analysis [28] has reported that the absolute levels of NCAM-1/CD56 were significantly increased following antipsychotic treatment and that the percentages of CD4 and NCAM-1/CD56 lymphocytes were significantly increased in acutely relapsed inpatients compared to controls. Therefore, future research will be necessary to clarify the immunological alterations of CD56 in SZ.
Several investigations have suggested a connection between SZ and changes in growth factors and/or neurotrophic factors, including BDNF, IGF-1, and IGFBP [29,30]. With regard to IGFs, including IGFBP-1, IGFBP-2, and IGFBP-3, we did not find any significant differences in the levels of IGFBP after treatment. A 20-week clinical trial [31] of treatment with a program of resistance or concurrent exercise did not show significant changes in IGF-1 and IGFBP-3 levels in patients with SZ after treatment, which is similar to the results of the present study. However, our results showed significant correlations between the changes in severity and the baseline levels of IGFBP3, which suggests a potential treatment for future trials. We found no significant differences in the levels of GDNF and NGF after treatment. Compared with healthy subjects, patients with SZ exhibit decreased levels of NGF [32], and a random-effects meta-analysis showed similar results [33]. Furthermore, GDNF levels have been shown to increase along with a reduction of psychotic symptoms in patients with SZ after antipsychotic treatment [10], but another study demonstrated that the serum levels of GDNF did not differ between patients with SZ and healthy controls [11]. A cross-sectional observational study did not find significant differences in the levels of GDNF and NGF between responders and nonresponders treated with clozapine [34]. Although no significant changes in BDNF levels after treatment were found, our results demonstrated that the baseline levels and changes in psychotic severity were significantly associated with changes in BDNF. Patients with SZ exhibit decreased levels of BDNF compared to healthy controls [32]. Another prospective study did not find changes in BDNF levels in patients’ serum, even though the psychosis severity significantly improved after six weeks of antipsychotic treatment [35]. To summarize, the results of the present study suggests that BDNF, GDNF, and NGF may play a role in the progression of SZ, and additional studies are needed to help clarify this suggestion.
We reported the results of the comparisons of multiple groups of cytokines and assessments of psychotic severity. Thus, our results will be helpful for understanding the changes in the immunological, inflammatory, and neurodevelopment mechanisms that have been observed in patients suffering from chronic SZ. Furthermore, our eight-week study period extended across the acute and maintenance stages, which was a strength of the study. However, the following limitations of the study should be considered. First, the lack of a healthy control group and drug-naïve control group was a problem because placebo effects and other confounding factors might have affected our results. Second, because this was a naturalistic study, the antipsychotic agents were adjusted flexibly and therefore not well controlled. Finally, the relatively small number of patients enrolled in the study limits the generalizability of the results.
In conclusion, in this study, we found that the levels of IL-1-ra were significantly decreased after eight weeks of antipsychotic treatment and that levels of NCAM-1/CD56 were significantly decreased in patients with SZ who received SGAs but not FGAs. Further studies are needed to confirm our results.
Acknowledgements
We are grateful to our patients and their parents who voluntarily participated in our study and gave valuable information. This work was supported by grants VGHKS13-CT5-08 from Kaohsiung Veterans General Hospital, Taiwan.