Overview of the Korean Longitudinal Study on Cognitive Aging and Dementia
Article information
Abstract
Objective
Due to an unprecedented rate of population aging, South Korea is facing a dementia epidemic. For this reason, the Korean Longitudinal Study on Cognitive Aging and Dementia (KLOSCAD) was launched in 2009 with support from the Korean Health Industry Development Institute to investigate the epidemiology, biopsychosocial risk factors, and outcomes of dementia and dementia-related conditions.
Methods
The KLOSCAD is the first nationwide multi-center population-based prospective cohort study. In October 2010, 12,694 individuals were randomly sampled from residents aged 60 years or older who lived in 13 districts across South Korea. In the baseline assessment, which was conducted from November 2010 through October 2012, 6,818 (53.7%) individuals participated. Follow-up assessments have been conducted every two years, with the first follow-up assessment conducted between November 2012 and October 2014, and the second between November 2014 and October 2016. The third is now in progress, and will span from November 2016 to October 2018. Diagnosis of cognitive disorders, neuropsychological battery, behavioral and psychological symptoms of dementia, activities of daily living, physical and neurologic examination and laboratory tests, life styles, quality of life, and identification of death were evaluated in each assessment.
Results
The cumulative drop-out rate at the second follow-up assessment was 38.7%. Dementia and mild cognitive impairment were 5.0% and 27.0%, respectively.
Conclusion
The KLOSCAD may provide strong scientific evidence for advancing the fight against dementia both in Korea and globally.
INTRODUCTION
Most dementing illnesses are complex multifactorial diseases that are incurable and require comprehensive and longterm observation. In developed Western countries that became an aged society (at least 14% of the national population 65 or older defined by the United Nations) earlier than Korea, community-based prospective cohort studies on aging and dementia have been being actively conducted since the early 1990s. In many Asian countries that are rapidly aging, most community-based prospective cohort studies on aging and dementia began after the year 2000. Asians have different genetic backgrounds, environments, and life styles and thus may have different disease epidemiology and dementia risk factors than Caucasians.
In South Korea (hereafter, Korea), the number of dementia patients is rapidly increasing due to an unprecedented rate of population aging. It will take only 25 years for Korea to shift from an aging society into a superaged society. Korea became an aging society in 2000, and is expected to become an aged society by the end of 2017, and a superaged society by 2025 [1]. In 2017, the prevalence of dementia among Koreans aged 65 years or older was estimated to be 10.2%, and the number of individuals with dementia to be 724,857 [2,3]. The number of dementia patients will double every 17 years and reach nearly 3 million in 2050 [2,3]. The age-standardized incidence of Alzheimer’s disease (AD) and mild cognitive impairment (MCI) is reported to be 7.9 and 28.1 cases per 1,000 person-years, respectively [4]. The current national dementia cost to Korea is estimated to be approximately 12 billion US dollars (USD), which is approximately 0.9% of the Korean national gross domestic product (GDP). This cost is expected to double every 10 years and will reach approximately 93 billion USD by 2050, which will be approximately 3.8% of the expected Korean national GDP [5].
The Korean government declared ‘A War Against Dementia’ in 2008 and has been preparing a National Dementia Plan every five years. The Korean National Assembly unanimously passed the ‘Dementia Management Act (DeMA)’ in August 2011. Based on the National Dementia Plans, the Korean government began to support a community-based prospective elderly cohort study that aimed to investigate epidemiological estimates, risk factors, preventive measures, and outcomes of dementia. This study, the Korean Longitudinal Study on Cognitive Aging and Dementia (KLOSCAD), is the first multicenter nationwide population-based prospective cohort study for investigating the epidemiology, biopsychosocial risk factors, and outcomes of normal cognitive aging and various dementing illnesses. The study launched in 2009 with support from the Korean Health Industry Development Institute. The four main aims of this study were to: 1) estimate the epidemiology of dementia and related disorders in Korea; 2) explore the diagnostic markers of dementia and establish their normative data in elderly Koreans; 3) propose optimal strategies for preventing and managing dementia in Koreans; and 4) provide evidence for developing cost-effective dementia policies in Korea.
Methods
Subjects (Table 1)

Demographic and clinical characteristics of the study subjects at baseline, 1st follow-up, and 2nd follow-up
The initial sample size (NS) of the KLOSCAD was estimated to be 6,248 using the following equation:
NS=1.962 PQW/[E2+(1.962 PQW/NT)]
where P refers to the expected prevalence (%) of dementia, Q refers to 100-P (%), W refers to the expected design effect, E refers to the maximum acceptable random sampling error (%), and NT refers to the number of the total population [6]. P was assumed to be 8.94%, which was the estimated prevalence of dementia in 2011 based on a previous nationwide survey performed in 2008 [3]. W was assumed to be 2, and E was set as 1%. The number of Korean individuals aged 65 years old or over in 2011 (5,700,972) was computed as NT. Assuming a response rate of 50%, we needed to approach 12,496 individuals to obtain our desired sample of 6,248. Assuming a response rate of 50%, we needed to approach 12,496 individuals to obtain our desired sample of 6,248. In order to construct a representative cohort of elderly Koreans, we randomly sampled 30 villages and towns from 13 districts across South Korea. We then randomly selected 10% of residents aged 60 years or older in urban areas and 20% in rural areas using residential rosters on October 2010. Finally, 12,694 elderly individuals were sampled, and 6,818 (53.7%) participated in the baseline assessment of the KLOSCAD. All participants were fully informed of the study protocol, and provided written informed consent, signed by the subjects or their legal guardians.
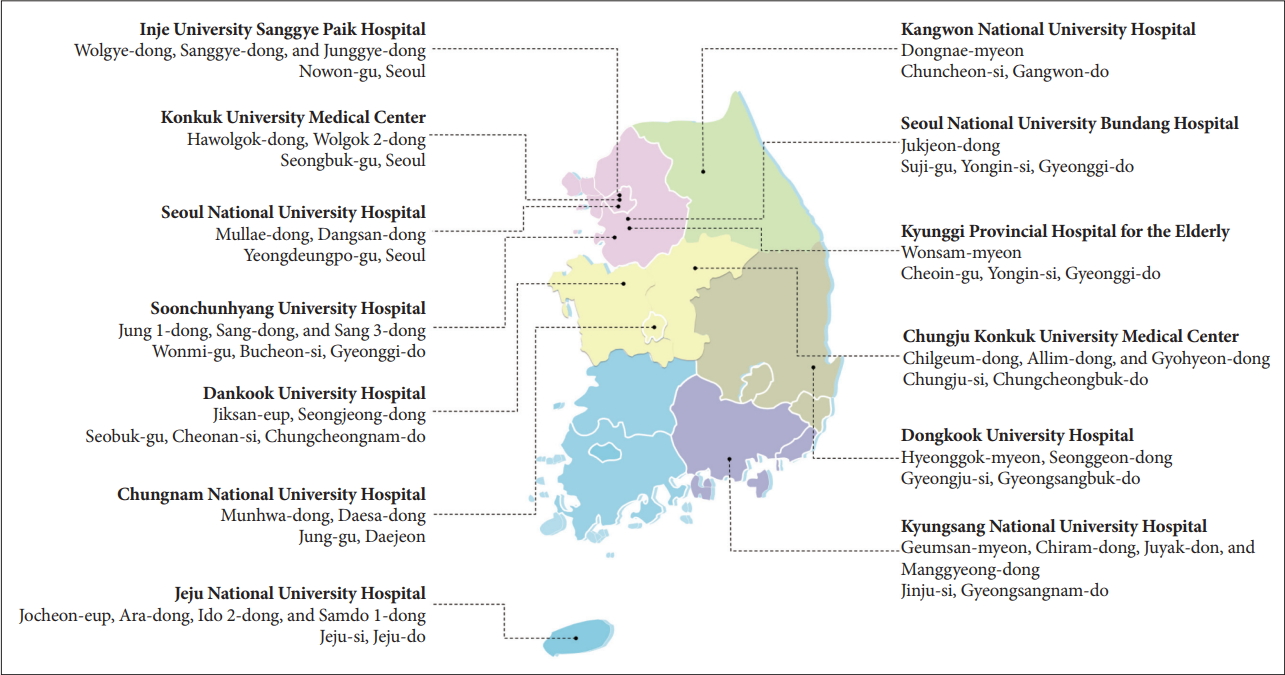
Research centers (Figure 1)
The KLOSCAD is a multi-center study steered by Seoul National University Bundang Hospital (SNUBH). Including SNUBH, 13 research centers across the country participate in the KLOSCAD: 3 in Seoul, 3 in Gyeonggi-do, 1 in Gangwondo, 2 in Chungcheongnam-do, 1 in Chungcheongbuk-do, 1 in Gyeongsangbuk-do, 1 in Gyeongsangnam-do, and 1 in Jejudo. Each center was responsible for evaluating participants from a particular district. All investigators and research staff, including geropsychiatrists, neuropsychologists, and nurses from the 13 research centers, completed 8 hours of protocol-based training and passed 10 case examination tests prior to the baseline assessment.
Schedules
The baseline evaluation was conducted over two years, from November 2010 to October 2012. Follow-up evaluations have been conducted every two years. The first follow-up evaluation was conducted from November 2012 to October 2014, the second from November 2014 to October 2016, and the third (currently in progress) from November 2016 to October 2018. The Institutional Review Board of SNUBH (no. B-0912/089-010), Korea, approved this study protocol.
Assessments
Diagnostic assessments of cognitive disorders and comorbid conditions
Geriatric neuropsychiatrists with expertise in dementia research administered a face-to-face standardized diagnostic interview as well as physical and neurological examinations using the Korean version of the Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet (CERAD-K) Clinical Assessment Battery (CERAD-K-C) [7] to diagnose cognitive disorders. Comorbid mental disorders, including depressive disorders, were evaluated using the Korean version of Mini International Neuropsychiatric Interview (MINI-K) [8,9], and cerebrovascular accidents were evaluated using the Transient Ischemic Attack and Stroke Interview form from the Atherosclerosis Risk In Community study (ARIC) [10]. The Unified Parkinson’s Disease Rating Scale (UPDRS) [11] was administered to the subjects found to be abnormal in Tinetti Performance Oriented Mobility Assessment (POMA) [12] and/or the Screening Questionnaire for Parkinson’s Disease (PDSQ) [13] and/or who had a history of movement disorders including Parkinson’s disease. Trained research nurses examined the family history of cognitive disorders, cerebrovascular diseases, and Parkinson’s disease in first-degree relatives using a study-specific form that included the kinship with the subject and age of onset. Rapid eye movement (REM) sleep behavior disorders, restless legs syndrome, and sleep apnea were screened using the REM Sleep Behavior Disorder Screening Questionnaire (RBDSQ) [14], Cambridge Hopkins questionnaire for ascertainment of restless legs syndrome (CH RLSq) [15], and the STOP-Bang questionnaire (STOPQ) [16] respectively.
Cognitive function assessments
Trained research nurses administered the Subjective Memory Complaints Questionnaire (SMCQ) [17] to the subjects and the Korean version of the Short Informant Questionnaire on Cognitive Decline in the Elderly (SIQCODE-K) [18] to their informants to evaluate subjective complaints associated with cognitive impairment. Research neuropsychologists or trained research nurses administered the Korean version of the Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet (CERAD-K) Neuropsychological Assessment Battery (CERAD-K-N) [7,19], Digit Span Test (DST) [20], Executive Clock Drawing Task (CLOX) [21,22], Frontal Assessment Battery [23], and Severe Cognitive Impairment Rating Scale (SCIRS) [24] to each subject. The CERAD-K-N consists of nine neuropsychological tests: Verbal Fluency Test, 15-item Boston Naming Test, Mini Mental Status Examination, Word List Memory Test, Constructional Praxis Test, Word List Recall Test, Word List Recognition Test, Constructional Recall Test, and Trail Making Test A/B [7,19].
Behavioral and psychological symptoms of dementia assessments
Trained research nurses evaluated behavioral and psychological symptoms of dementia (BPSD) using the Korean version of the Geriatric Depression Scale (GDS-K) [24], the Korean version of the Neuropsychiatric Inventory (NPI-K) [25], the Korean version of Dysexecutive Questionnaire (DEX-K) [26,27], and the Sleep Disorder Inventory (SDI-K) [28].
Activities of daily living assessments
Trained research nurses evaluated the basic and instrumental activities of daily living (ADL) using the Disability Assessment for Dementia (DAD) [29,30], and the level of dependency using Dependence Scale (DS) [31,32].
Physical and neurologic examination and laboratory tests
Geriatric neuropsychiatrists conducted routine physical and neurologic examinations. They evaluated gait and balance using the Tinetti Performance Oriented Mobility Assessment (POMA) [12]. Research nurses checked vital signs (blood pressure, heart rate, and respiration rate), and measured height, weight, and head, neck, waist, and hip circumferences. They evaluated all medications that the subjects were taking or had taken within six weeks using a study-specific assessment form, and the burden of comorbid illnesses using the Cumulative Illness Rating Scale (CIRS) [33]. They also evaluated handedness using the Edinburgh Handedness Inventory [34]. Complete blood cell counts, chemistry profiles, a rapid plasma reagin (RPR) test for screening syphilis, a thyroid function test (free T4, thyroid stimulating hormone), and vitamin B12, folate, and apolipoprotein E (APOE) genotyping were administered to all subjects. Additionally, brain magnetic resonance imaging [T1-weighted, T2-weighted, and Fluid-attenuated inversion recovery (FLAIR)] was performed on the subjects who were diagnosed with dementia.
Life styles
Trained research nurses evaluated socio-demographic information, social activities, and occupational history using studyspecific assessment forms in face-to-face interviews, and evaluated the risk of driving using the Driving Risk Questionnaire (DRQ) [35]. They evaluated the use of nutritional supplements and beverages using study-specific assessment forms in faceto-face interviews, at-risk drinking using the Korean version of Alcohol Use Disorders Identification Test (AUDIT-K) [36,37], and nicotine dependence using the Korean version of the Fagerstrom Test for Nicotine Dependence (FTND-K) [38,39]. Additionally, they also evaluated sleep habit and quality using the Korean version of the Pittsburgh Sleep Quality Index (PSQI) [40].
Quality of life
Trained research nurses evaluated QoL using the EuroQol (EQ)-5D [41] and the Quality of Life-Alzheimer’s disease (QoL-AD) [42,43], and the level of perceived social support using the Medical Outcomes Study Social Support Survey [44].
Identification of death
We identified the deaths of subjects annually from the National Mortality Database of Statistics Korea.
Diagnosis
A panel of research neuropsychiatrists determined the final diagnoses and the Clinical Dementia Rating (CDR) [45]. They diagnosed dementia according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnostic criteria [46]. They determined the subtypes of dementia according to the following diagnostic criteria: AD according to the criteria of the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association [47], vascular dementia (VaD) according to the criteria of the National Institute of Neurological Disorders and Stroke-Association Internationale pour la Recherche et l’Enseigne-menten Neurosciences [48], dementia with Lewy bodies (DLB) and Parkinson’s disease with dementia (PDD) according to the consensus guideline proposed by McKeith et al. [49], frontotemporal lobar degeneration (FTLD) according to the Neary criteria [50], and alcohol-related dementia (ARD) according to the diagnostic criteria proposed by Oslin et al. [51] MCI was diagnosed according to the Consensus Criteria from the International Working Group on MCI [52]. The presence of objective cognitive impairment was ascertained when the performance of the subjects was -1.5 standard deviations (SD) or below the age-, gender-, and education-adjusted norms in any of neuropsychological tests.
Major depressive disorder (MDD) was diagnosed according to the DSM-IV criteria, and minor depressive disorder (MnDD) according to research criteria proposed in Appendix B of the DSM-IV criteria. Subsyndromal depression (SSD) was defined according to the following study-specific operational criteria: 1) the presence of two or more concurrent symptoms of depression by the DSM-IV with at least one being a core depressive symptom such as depressed mood or loss of interest, 2) the presence of each symptom for ‘more than half of every day’ or ‘more than seven days during two weeks,’ 3) evidence of social and occupational dysfunction, and 4) does not meet the criteria for the diagnosis of MDD or MnDD.
Analysis
The research geropsychiatrists and research statisticians estimated the age group (60–65 years old, 65–69 years old, 70–74 years old, 75–79 years old, 80 years old or over) and gender-specific prevalence and incidence. For each estimate, 95% confidence intervals (CI) were derived using the exact binomial method. Standardized prevalence and incidence rates of elderly Koreans were estimated using the direct standardization method, in which age, gender, and education were adjusted using data from the 2010 National Census of Korea. Risk factors were explored using logistical regression analysis, cox proportional hazard analysis, or path analysis. Survival and institutionalization were estimated using the Kaplan-Meier survival analysis.
Results
Progress of the Study
Response rate
The cumulative drop-out rate at the second follow-up assessment was 38.7%. In the first follow-up assessment, 1,494 did not respond (‘Lost’ in Figure 2); 1,170 refused to participate, 50 were institutionalized, 56 were too unwell to participate, and 218 moved or changed their contact information. In the second follow-up assessment, 2,178 did not respond (‘Lost’ in Figure 2); 1,263 refused to participate, 89 were institutionalized, 37 were too unwell to participate, and 789 moved or changed their contact information.
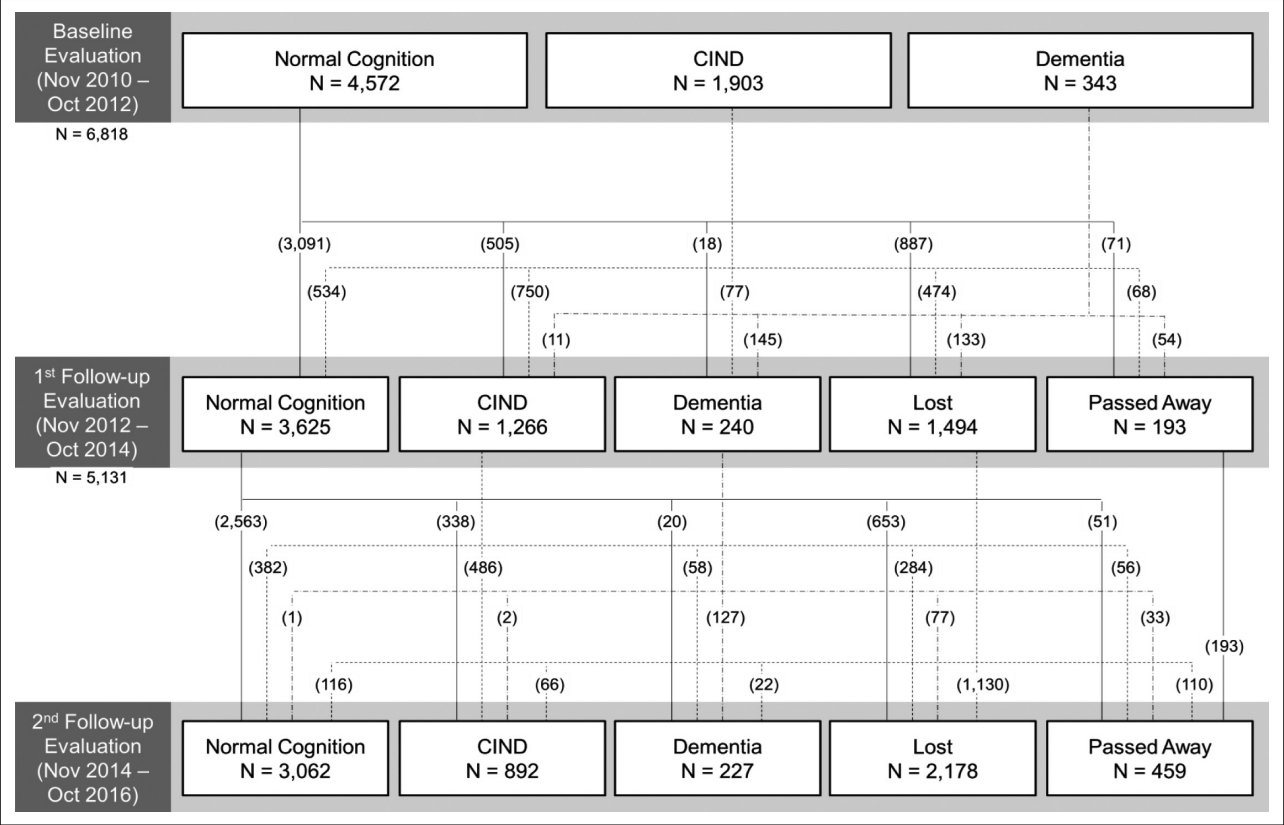
Flow diagram of the Korean Longitudinal Study on Cognitive Aging and Dementia (KLOSCAD). CIND: cognitive impairment not dementia.
The demographic and clinical characteristics of the subjects in the baseline, first follow-up, and second follow-up assessments are summarized in Table 1. The subjects in the follow-up evaluations were older, more educated, and had lower depression scale scores. The CIRS scores that indicate the cumulative burden of comorbid diseases increased with the aging of the cohort. With an increase in the number of follow-up assessments, the proportion of cognitively normal participants increased (67.1% at baseline, 70.6% at 1st followup, 73.2% at 2nd follow-up).
International collaboration
The KLOSCAD participates in the development of the Cohort Studies of Memory in an International Consortium (COSMIC) [53], and has contributed to various collaborative research projects on cognitive disorders [54,55]. The KLOSCAD is one of the contributors of the International Neuropsychological Normative Database Initiative (INNDI), which aims to develop regression-based norms that enable users to adjust cognitive test scores for a test taker’s age, sex, education, country of origin, and language [56]. The KLOSCAD has also contributed to the Global Alzheimer’s Association Interactive Net-work (GAAIN), which is an operational online integrated research platform of global networks of Alzheimer’s disease study centers [57].
Discussion
The KLOSCAD is the first multi-center nationwide population-based prospective cohort study on cognitive aging and dementia in Korea. Since we expect that more than 3,000 subjects will respond to the third follow-up assessment, we are preparing to extend this study until 2024. Attrition based on the disproportionate loss of subjects presenting cognitive decline over time might lead to biased estimates of longitudinal outcomes. Among the baseline diagnosis, 34.3% of cognitive normal, 43.1% of MCI, and 71.7% of dementia were lost to the 2nd follow-up assessment. We will investigate attrition and reflect it in the design and analysis of specific hypotheses [58]. The KLOSCAD will not only provide epidemiological data of dementia and related disorders, but also find the various diagnostic and predictive markers for dementia using data from comprehensive assessments. We believe this study will provide strong scientific evidence for advancing the fight against dementia, both in Korea and globally.
Acknowledgements
This study was supported by a grant from the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea [grant no. HI09C1379 (A092077)].