Neuropsychological Tests for Patients with Marchiafava-Bignami Disease: A Case Report
Article information
To the Editor,
Here we report a case of a male patient with Marchiafava-Bignami disease (MBD). This report focuses on the clinical presentation and neuropsychiatric symptoms of MBD. The study was approved by the Institutional Review Board (IRB) of Soonchunhyang University Bucheon Hospital (2020-07-023).
A 37-year-old male patient visited the outpatient clinic and presented with a 9-month history of lack of energy. He is a high-school graduate and an office worker living with his wife and two children. He had no underlying disease, but drank 4–6 bottles of soju (about 28–42 alcohol units) every day for the past five years. During the interview, he spoke very little. According to his wife, he has been slow to do everything for the past six months, and was unable to perform his job. He could not even do simple things at home until his wife ordered him. Even so, the patient’s performance was very lethargic. For example, he took several hours to get ready to go out. His wife reported that the lack of energy, apathy, and distraction were the main issues.
Laboratory screening was normal. His neurological examination revealed no neurological deficit. Magnetic resonance imaging (MRI) of the brain demonstrated a bilaterally symmetrical T2/FLAIR high-signal intensity lesion involving corpus callsosum genu, body, bilateral frontal white matter, internal capsule, and corticospinal tracts (Figure 1). According to his brain MRI report, the patient was suspected to have MBD. During the patient’s first visit, some questionnaires were administered and the respective scores obtained were: Generalized Anxiety Disorder-7, Patient Health Questionnaire-9, and Pittsburgh Sleep Quality Index–1, 8, and 1. The scores revealed mild depression, but no evidence of clinically significant depression was detected during the interview. Initial scores of Mini-Mental Status Examination (MMSE) and Global Deterioration Scale (GDS) were 27 (time orientation -1, recall -2) and 3, respectively. The patient also underwent a battery of neuropsychological tests. Overall intellectual ability of the patient was borderline level. The patient exhibited very low levels of memory and frontal-executive functions, and decreased social function and activities of daily life. The performance in emotion-related tests was generally non-specific. Detailed results are presented in Table 1.
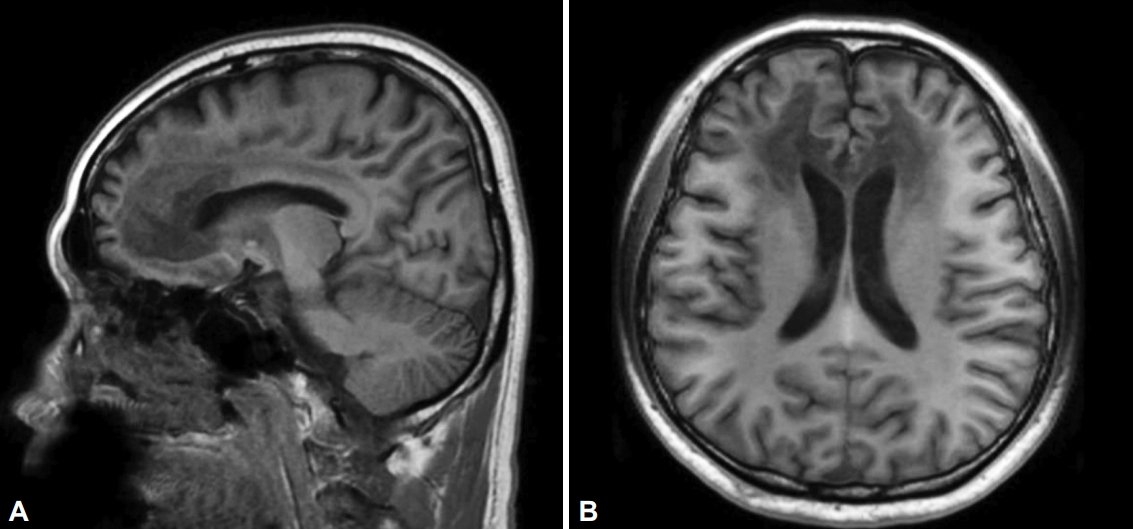
Brain magnetic resonance imaging of the patient. A: Sagittal view of T1-weighted brain image. B: Axial view of T1-weighted brain image. The summary of MRI findings: Bilaterally symmetrical T2/FLAIR high-signal intensity lesion involving corpus callsosum genu, body, bilateral frontal white matter, internal capsule, and corticospinal tracts, Marchiafava-Bignami disease involvement.
We initially administered 50 mg of IV thiamine and gradually increased to 600 mg. After 15 days of treatment, the patient’s wife reported that his memory and apathy symptom were slightly improved. He often spoke something and laughed while watching TV unlike before. However, there was a wide fluctuation in his symptoms, and his slowness was not improved. The MMSE and GDS tests were also checked again. The total scores of these scales were the same as the initial values, but the subscores of MMSE changed (time orientation -1, recall -2 → time orientation -1, attention and concentration -1, recall -1).
MBD is a rare sequelae of chronic alcoholism, and can result in progressive demyelination and necrosis of the corpus callosum [1]. A brain MRI may be necessary for MBD diagnosis [2,3]. The clinical presentation of this disease includes various non-specific symptoms and signs, such as decreased consciousness, psychotic symptoms, depression, apathy, aggression, seizures, hemiparesis, ataxia, apraxia, confusion, dysarthria, behavioral abnormalities, memory deficits, gait disorders, coma, and death [4]. Until now, there have been few guidelines for management of MBD. Several case reports of MBD have demonstrated the effectiveness of treatment with thiamine, corticosteroid, or amantadine [1,4,5]. However, the prognosis of this condition is worse: as of 2004, among approximately 250 reported patients, only 20 experienced positive outcomes [4].
The present case presents a 37-year-old male patient with MBD. The chief complaints were lack of energy, apathy, and distraction, although the general medical condition was relatively fine. The initial MMSE and GDS scores were relatively less severe than our clinical impression. However, the battery of neuropsychological tests revealed the patient’s problem such as cognitive impairment in further detail. Based on our case results, clinicians may consider adopting a detailed neuropsychological battery to better understand the clinical manifestations of patients with MBD. Unlike other case report [1], the effects of parenteral thiamine therapy in our case were inadequately reflected by the MMSE scores, although the caregiver reported a slight improvement of symptoms. We speculate that it may be associated with relatively high level of initial MMSE score of our patient.
MBD was first described in 1903 by Italian pathologists [6], but few studies have been reported since then except a few case reports because of low prevalence. Accordingly, MBD is not clearly understood and additional reports are still needed. In our case report, we introduced male MBD patients with cognitive impairment based on a battery of neuropsychological tests and relatively fine general condition. Clinicians may have the potential to meet MBD patients at any time because of the large population of chronic alcoholic patients worldwide. We believe that our report may help clinicians assess and treat patients with MBD.
Acknowledgements
This study was supported by the Soonchunhyang Research Fund.
Notes
The authors have no potential conflicts of interest to disclose.
Authors’ contribution
CConceptualization: Han-yong Jung. Data curation: HyunChul Youn. Formal analysis: HyunChul Youn. Funding acquisition: Han-yong Jung. Investigation: HyunChul Youn. Methodology: HyunChul Youn, Jeewon Lee, Soyoung Irene Lee. Project administration: Shin-Gyeom Kim, Han-yong Jung. Supervision: Han-yong Jung. Validation: Shin-Gyeom Kim, Jeewon Lee, Soyoung Irene Lee. Visualization: HyunChul Youn. Writing—original draft: HyunChul Youn. Writing—review & editing: all authors.

