A Literature Review on the Efficacy and Related Neural Effects of Pharmacological and Psychosocial Treatments in Individuals With Internet Gaming Disorder
Article information
Abstract
Objective
Internet gaming disorder (IGD) has attracted considerable attention as a serious mental and public health issue worldwide. Currently, there are no established treatment guidelines for IGD. Herein, we review the latest findings on the efficacy and related neural effects of pharmacological and psychosocial treatments for individuals with IGD.
Methods
A database search of relevant studies published between 2007 and 2020 was conducted using PubMed and Google Scholar. Twenty-seven studies were reviewed for current evidence related to the efficacy and neural effects of pharmacological and psychosocial IGD treatments.
Results
Pharmacological studies suggest that bupropion may play a significant role in IGD. Additionally, nuclear imaging studies on IGD have demonstrated functional impairment of the dopamine system, providing a neurobiological basis for the efficacy of dopamine-enhancing drugs. Among the various psychosocial interventions, current evidence suggests that cognitive behavioral therapy may be an effective intervention for IGD. Cognitive behavioral therapy and bupropion were found to influence resting-state functional connectivity within the cortico-subcortical circuit and default mode network, suggesting a possible neural mechanism. Innovative approaches, including virtual reality treatment, residential camps, voluntary abstinence, and transcranial direct current stimulation, have shown promising results. However, methodological limitations, such as the absence of proper controls, small sample sizes, short duration, inconsistency of inclusion criteria across studies, and self-report measures of outcome, hamper conclusions regarding the efficacy of treatments.
Conclusion
Ongoing basic research and clinical trials overcoming these limitations could add to the existing knowledge on IGD and contribute to the development of evidence-based treatments.
INTRODUCTION
Excessive Internet use is increasingly being recognized as a significant mental health problem, and the number of studies focusing on pathological on-line gaming has increased substantially over the past two decades [1,2]. Internet gaming disorder (IGD) was included in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as a tentative disorder needing further research [3]. The DSM-5 defines IGD as “persistent and recurrent use of the internet to engage in games, often with other players, leading to clinically significant impairment or distress.” The nine criteria for IGD in the DSM-5 are based on preliminary studies outlining the criteria for substance use disorder and gambling disorder. IGD, as a form of behavioral addiction, shares typical characteristics with substance addiction, including withdrawal, tolerance, loss of control, and cravings [4]. Before the DSM-5 criteria, various instruments, such as the Beard Diagnostic Questionnaire [5], the Young Internet Addiction Scale (YIAS) [6], and the Scale for the Assessment of Internet and Computer game Addiction (AICA-S) [7], were used to assess excessive online gaming. The criteria of these scales differed somewhat from one another [8]. The DSM-5 criteria have contributed to the accumulation of reliable results for IGD.
There is no consensus on the prevalence rate of IGD in the general population; most studies on IGD have investigated self-selected teenagers. Previous studies applying the DSM-5 criteria have reported an incidence of IGD ranging from 1.2% to 5.9% in adolescents [9-13], with the proportion of males with IGD being consistently greater than that of females. IGD has become a significant public health problem in some Asian countries due to its increasing prevalence and negative impact on mental health [14-17]. Approximately 7.4% of South Koreans aged 20–40 years were estimated to be at risk for IGD based on the DSM-5 criteria [18]. Overall socioeconomic costs in South Korea due to Internet addiction (IA), including pathological online gaming, were estimated to be in the range of 1.5–4.5 billion US dollars in 2009 [19]. Although controversy exists over whether these behavioral problems should be classified as a primary mental disorder [20], a growing body of literature has indicated that pathological online gaming is related to social problems and a variety of psychological and behavioral problems, including emotional symptoms, impulsivity, hyperactivity/inattention, anxiety, sleep disturbance, and self-injurious behavior [2,8,16]. Although rare, game-induced epileptic seizures have been reported in severe cases [21]. Additionally, IGD has been found to be frequently comorbid with other psychiatric disorders such as depression [9,17,22,23], attention-deficit/hyperactivity disorder (ADHD) [22,24,25], obsessive compulsive disorder [22,24], and substance abuse [26].
Regardless of the inclusion of IGD as an established mental disorder, there is a growing need for evidence-based guidelines for the effective treatment of this condition. Many individuals with pathological online gaming have sought and received various forms of treatment from mental health professionals [27,28], and in some countries, there are psychiatric clinics and centers that offer specific treatment for patients with IGD. However, updated information on effective treatments for IGD is needed by clinicians. This study reviewed the current evidence on the efficacy and related neural effects of pharmacological and psychosocial treatment of IGD. Furthermore, nuclear and genetic findings suggesting the neurobiological underpinning and mechanism of IGD were reviewed to elucidate the underlying role of dopamine-enhancing drugs in the treatment of IGD. Finally, we considered the limitations of previous studies and provided recommendations for future research.
METHODS
Study selection process
We searched the PubMed database (available at http://www.pubmed.ncbi.nlm.nih.gov) and Google Scholar (available at http://www.scholar.google.com) between 2007 and 2020 using the following key words: “Internet gaming disorder,” “Internet game,” “Internet video game,” “problematic online gaming,” “game addiction,” “Internet addiction,” “online games,” and “treatment.” The eligibility criteria for selecting studies were as follows: 1) participants were diagnosed with IGD or problems related to excessive gaming; 2) detailed information regarding the intervention was provided; 3) the experimental design was either multi-armed (randomized or non-randomized) or a pre-post comparisons; 4) the outcome was measured by IGD symptom severity or gaming time; 5) the number of participants per group was nine or greater; 6) studies were available in English; and 7) studies focusing on epidemiology or prevention rather than treatment were also excluded.
RESULTS
A database search resulted in 1,494 records. After screening, based on the title and abstract information, 45 studies remained and underwent extensive review by three reviewers. Of the 45 studies, 18 did not meet the following eligibility criteria: 11 studies included individuals with IA or Internet use disorder, 3 did not evaluate the treatment outcome related to IGD severity or gaming time, 2 did not provide detailed information regarding the intervention, 1 was not an experimental design, and 1 was not available in English. Finally, 27 studies were included in this review (Figure 1).
Pharmacological treatment of IGD
Antidepressants
Among antidepressants, only bupropion and escitalopram have been evaluated for use as an IGD treatment. Bupropion can inhibit the reuptake of both dopamine and norepinephrine [29,30]; besides its antidepressant effects, bupropion attenuates craving and withdrawal, which help in smoking cessation [31]. Bupropion has also been found to effectively treat ADHD [32] and gambling disorder [33]. Escitalopram is one of the selective serotonin reuptake inhibitors (SSRIs) used broadly for the treatment of major depressive disorder (MDD) [34] and anxiety disorder [35]. In the first case of escitalopram use in a patient with IGD, it was found that 30 mg/day of escitalopram for three months reduced the urges for gaming significantly, with complete functional recovery [36].
The first open-label trial [37] using bupropion evaluated the efficacy and neural effects of six weeks of treatment in 11 male patients with comorbid IGD and subclinical depression. Bupropion was administered at a dose of 150 mg/day during the first week and increased to 300 mg/day thereafter. At baseline, hyperactivation of the dorsolateral prefrontal cortex (DLPFC) in response to gaming cues was found in patients with IGD, compared with controls. After bupropion treatment, IGD severity as well as gaming time and craving significantly decreased in patients with IGD. Interestingly, the activation of the DLPFC to gaming cues decreased and was positively correlated with game craving, suggesting that bupropion may decrease craving by attenuating activation of the DLPFC, possibly through modulating both dopamine and norepinephrine.
In a study by Han and Renshaw [38], 50 male IGD patients with comorbid MDD were randomly assigned to the bupropion or placebo groups in a 12-week trial. The starting dose of bupropion was 150 mg/day and was increased during the first week to 300 mg/day. Both groups received weekly educational sessions on healthy Internet use and the adverse consequences of excessive gaming. The YIAS, Clinical Global ImpressionSeverity (CGI-S), Beck Depression Inventory (BDI), and total time spent gaming were used to assess treatment efficacy. Following eight weeks of active treatment, IGD severity, depressive symptoms, and gaming time improved markedly in the bupropion group compared with the placebo group. During the four weeks of the post-treatment phase, there was no significant change in IGD severity or gaming time in either group, whereas the BDI scores of the bupropion-treated group increased to the level of the placebo, suggesting that the effect of bupropion on IGD symptoms may be independent of its effect on depression.
Bae et al. [39] investigated the efficacy of 12 weeks of bupropion treatment and related resting-state functional connectivity (RSFC) alterations in 16 patients with IGD. The starting dose of bupropion (150 mg/day) was adjusted to 300 mg/day in the second week based on efficacy and tolerability. At the end of the treatment period, a significant improvement in the total YIAS score was observed. The other clinical symptoms, evaluated with the BDI, ADHD Rating Scale (ARS), and Behavioral Inhibition and Activation Scales (BIS/BAS), also showed improvement. After bupropion treatment, RSFC decreased not only within the default mode network (DMN) but also between the DMN and cognitive control network. Bupropioninduced alterations in RSFC within the DMN were significantly correlated with clinical improvement, suggesting that the DMN may potentially be associated with the therapeutic effect of bupropion.
In an open-label comparative 6-week trial of bupropion and escitalopram [40], 119 patients with IGD were randomly assigned to a bupropion group (n=44), an escitalopram group (n=42), or an observation group (n=33). Clinical outcomes were measured using the YIAS, CGI-S, BDI, ARS, BIS/BAS, and BIS. Depending on the individual symptoms during the first week of treatment, starting doses were increased from 150 mg/day and 10 mg/day of bupropion and escitalopram, respectively, to 300 mg/day and 20 mg/day. Compared with the observation group, both the bupropion and escitalopram groups showed greater improvement in all clinical outcome measures. In particular, significant reductions in total scores of the YIAS, CGI-S, ARS, and BIS were found in the bupropion group compared with those in the escitalopram group, suggesting that bupropion may be more efficacious than escitalopram in alleviating the severity of IGD and IGD-related attentional problems and impulsivity.
Nam et al. [41] conducted a 12-week comparative trial of bupropion versus escitalopram in a sample of individuals with comorbid IGD and MDD. Thirty subjects were randomly assigned to the bupropion or the escitalopram group. The initial doses of bupropion (150 mg/day) and escitalopram (10 mg/day) were increased to 300 mg/day and 20 mg/day respectively during the first week. Both groups also received education regarding Internet gaming. After the treatments, IGD and MDD symptoms significantly improved in both groups, with no significant differences between the treatment groups. Additionally, analysis of RSFC showed that bupropion decreased RSFC within both the DMN and the salience network (SN) as well as between the DMN and SN, whereas escitalopram attenuated RSFC only within the DMN. In particular, RSFC in the SN and between the DMN and SN significantly decreased in the bupropion group compared with that in the escitalopram group. Furthermore, this decreased RSFC was associated with an improvement in IGD symptoms and impulsivity.
Drugs used for the treatment of ADHD
Stimulants, such as methylphenidate (MPH), and non-stimulant medications, such as atomoxetine (ATM), are effective in treating ADHD through distinct pharmacological mechanisms [42]. The therapeutic effects of MPH on ADHD symptoms are associated with activities blocking dopamine and norepinephrine transporters, thus enhancing dopaminergic and noradrenergic neurotransmission within the central nervous system [43,44]. ATM primarily acts as a potent inhibitor of the presynaptic norepinephrine transporter, with minimal affinity for other neurotransmitter transporters or receptors [45,46]. Because of the higher prevalence of IGD in patients with ADHD [24], previous studies have investigated the efficacy of MPH and ATM on IGD symptoms in children and adolescents with ADHD [47,48].
Han et al. [47] first reported the effectiveness of MPH on IGD symptoms in a sample of children. Sixty-two drug-naïve children diagnosed with both ADHD and IGD were treated with osmotic release oral system-MPH for eight weeks. The mean maintenance dose of osmotic release oral system-MPH was 30.5±13.3 mg/day. After eight weeks of treatment, the severity of both IGD and ADHD was significantly reduced, and the mean gaming time had greatly decreased. The number of subjects classified as having severe IGD (a YIAS score greater than 80) decreased from 16 at baseline to 3 at the endpoint. The change in YIAS score was positively correlated with changes in inattention and omission errors. Post-hoc analysis revealed that subjects with severe IGD showed greater reduction in omission errors than their control counterparts. These results suggest that IGD and ADHD are closely related and that the two conditions may share a common etiology, such as functional deficit of the prefrontal cortex and dopaminergic neurotransmission [49,50].
In a 12-week randomized trial by Park et al. [48] the efficacy of MPH (n=44) versus ATM (n=42) was compared in adolescents with IGD and ADHD. Assessment evaluations included the YIAS, ARS, BIS/BAS, and the Children’s Depression Inventory. After two weeks, the initial doses of 10 mg/day of MPH and 10 mg/day of ATM were increased to 40 mg/day and 60 mg/day, respectively. By the end of the study, IGD severity and impulsivity had improved in both groups, and there was no significant difference between the two treatment groups. The MPH group showed greater improvement in ADHD severity than the ATM group, whereas the ATM group showed greater improvement in depression severity than the MPH group. In both groups, the change in BIS/BAS scores was positively correlated with that of YIAS scores, suggesting that impulsivity may be an important factor in the clinical improvement of IGD.
Nuclear imaging and genetic findings supporting IGD pharmacotherapy
Dopamine plays a key role in substance dependence by mediating both reward and withdrawal mechanisms [51,52]. In line with evidence that deficient dopamine reward activity is associated with drug and alcohol dependence [53-56], nuclear imaging studies using positron emission tomography (PET) and single-photon emission computed tomography (SPECT) have shown that dysfunction of the dopaminergic system may occur in individuals with IGD or IA. One PET study [57] that used 11C-raclopride to detect endogenous dopamine activity demonstrated that dopamine was released in the striatum during video gaming in healthy volunteers. The binding potential of 11C-raclopride to dopamine D2 receptors (DRD2) was reduced during video gaming, compared with baseline levels, indicating an increase in endogenous dopamine release and binding. The magnitude of change in binding potential was comparable to that following an injection of amphetamine, suggesting that, similar to psychostimulant drugs, a significant change in dopaminergic activity can be induced by playing a video game. Furthermore, the reduced binding potential of 11C-raclopride was positively correlated with performance level. In a study by Kim et al. [58], DRD2 binding potential was assessed in males with and without IA using PET and 11C-raclopride. Individuals with IA exhibited decreased levels of DRD2 availability in the bilateral caudate and left putamen compared with controls, indicating hypodopaminergic activity in IA. Furthermore, the degree of DRD2 availability was negatively correlated with the severity of IA. The results of a genetic study by Han et al. [59] indicated that IGD may be associated with dopaminergic gene polymorphisms. The Taq1A1 allele of DRD2 and the low activity allele of catecholamine-O-methyltransferase were significantly more prevalent in individuals with IGD than in age-matched controls. Additionally, the presence of the DRD2 Taq1A1 allele was associated with a higher reward dependence. The DRD2 Taq1A1 allele has been found to be associated with reduced DRD2 density in the striatum and diminished dopaminergic tone [60,61]. Thus, these findings are consistent with reward deficiency syndrome [62].
The dopamine transporter (DAT) is a membrane protein that actively transports released dopamine into presynaptic neurons [63]. One previous study demonstrated alterations in DAT concentration in the striatum following psychostimulant administration [64]. One SPECT study [65] with 99mTc-TRODAT-1 examining presynaptic dopaminergic function found that DAT expression levels in the striatum were significantly reduced in individuals with IA compared with those in controls. Moreover, the volume, weight, and 99mTc-TRODAT-1 uptake ratio of the striatum were significantly decreased in individuals with IA compared with those in controls. Tian et al. [66] investigated DRD2 function and glucose metabolism both at rest and during Internet gaming tasks in patients with IGD using PET with 11C-N-methylspiperone and 18F-fluoro-deoxyglucose. Prefrontal glucose metabolism both at rest and during the Internet gaming tasks was significantly lower in the patients with IGD than in controls, reflecting prefrontal dysfunction similar to drug addiction [67]. 11C-N-methylspiperone binding level in the resting state was reduced in the inferior temporal gyrus in patients with IGD compared with that in controls. Similarly, the striatal 11C-N-methylspiperone binding potential of patients with IGD decreased significantly, compared with that in controls, following the Internet gaming task, indicating a decreased level of DRD2. In particular, a significant association was found in patients with IGD between lower DRD2 levels in the striatum and decreased glucose metabolism in the orbitofrontal cortex (OFC). The OFC has been implicated in the decision-making process [68], and dysfunction of the OFC is associated with compulsive drug use and impulsivity [55,69]. These results imply that DRD2-mediated prefrontal dysfunction could be an underlying mechanism of IGD. Taken together, these results suggest that excessive online gaming may be associated with the sub-sensitivity of the dopamine reward system, which provides a neurobiological basis for the efficacy of dopamine-enhancing drugs in IGD.
Psychosocial treatment of IGD
Cognitive behavioral therapy-based intervention
Cognitive behavioral therapy (CBT) has been applied in the treatment of various psychiatric disorders, including behavioral addictions such as gambling disorder [70]. A recently proposed model of IGD emphasizes that IGD is maintained by reduced cognitive control over decision-making processes and Internet-related cognitive bias and coping style [71]. Consistent with this model, CBT has been the main psychological intervention for IGD. During CBT, patients are taught to monitor their thoughts and identify those that cause addictive emotions and actions while they establish new coping skills to prevent relapses [6]. Sessions of CBT for IGD involve cognitive restructuring, problem-solving training, communication training, and relapse prevention. Besides standard CBT, various CBT-based psychotherapies that utilize distinctive techniques combined with CBT principles have been applied in the treatment of IGD.
Three studies [72-74] applying CBT-based interventions were randomized controlled trials (RCTs). In a multicenter RCT, Wölfling et al. [72] evaluated the effects of 15 weeks of manualized CBT, using short-term treatment for Internet and computer game addiction (STICA), compared with a wait-list control (WLC), in 143 male patients with IGD. The manualized CBT program consisted of 15 weekly group sessions and up to 8 additional 2-week individual sessions. The primary outcome was assessed using the AICA-S. Results showed that STICA facilitated remission (69.4%) compared with the WLC group (23.9%; OR=10.10). Furthermore, STICA was significantly more effective than WLC, with a large effect size for AICA-S (Cohen’s d=1.19) and gaming time (d=0.88).
Li et al. [73] investigated the efficacy of an 8-week group-based mindfulness-oriented recovery enhancement (MORE) program, compared with a support group, in 30 adults with IGD. The results showed higher reductions in the number of DSM-5 IGD criteria in the MORE group than in the supportive therapy group, with a large between-group effect size (Hedges’ g=0.78). The MORE group showed significantly greater reductions in craving for gaming and maladaptive cognitive tendencies related to gaming. These therapeutic effects were maintained at the 3-month follow-up.
In a study by Li and Wang [74], 28 adolescents with IGD were randomly assigned to a CBT group (n=14) and a clinical control group (n=14) for a 6-week trial. IGD severity was assessed using the YIAS and online game cognitive addiction scale (OGCAS). The CBT group received a 12-session course of CBT, and the control group received basic counseling regarding their online game playing behavior twice a week. After 6 weeks, both the CBT and control groups showed significantly lower OGCAS scores than those at baseline. However, there was no difference between the two groups in the overall reduction in the YIAS and OGCAS scores.
Kim et al. [75] evaluated the efficacy of CBT combined with bupropion, compared with that of bupropion treatment alone, in adolescents with IGD and comorbid MDD. Sixty-five adolescents with IGD and MDD were randomly assigned to either a CBT combined with bupropion group (n=32) or a bupropion group (n=33) in an 8-week trial. Participants in both groups were prescribed bupropion at 150 mg/day for the first week, followed by 300 mg/day thereafter. As expected, the results demonstrated that CBT with bupropion was more effective in reducing IGD severity and gaming time when compared to bupropion alone. There were no significant differences in the severity of depressive symptoms between the two groups.
Park et al. [76] compared the effects of CBT with virtual reality therapy (VRT) in 24 individuals with IGD. Participants were randomly assigned to either the CBT or VRT group and provided with therapy twice a week for four weeks. After four weeks of treatment, significant reductions in YIAS scores were observed in both groups; however, there was no significant change in YIAS scores between the two groups. Additionally, RSFC analyses demonstrated that CBT increased RSFC from the posterior cingulate cortex (PCC) to the bilateral thalami and right cerebellum. With regard to the VRT, increased RSFC from the PCC to the left middle frontal and bilateral temporal lobes was found, suggesting that VRT may alleviate IGD symptoms by facilitating a limbic-regulated response to rewarding stimuli.
Eight additional studies [77-84] applied CBT-based interventions for the treatment of IGD. González-Bueso et al. [77] evaluated the efficacy of CBT combined with psychoeducation. Thirty adolescents with IGD were divided into two experimental groups. Both groups received 12 sessions of CBT; parents in one group received 6 sessions of psychoeducational intervention. IGD severity was evaluated with the Diagnostic questionnaires for video games, mobile phone, or Internet addiction (DQVMIA). Significant decreases in DQVMIA scores were identified, with an effect size of d=0.70, but no significant difference was found in the reduction of DQVMIA scores between the two experimental groups.
Torrez-Rodríguez et al. [78] assessed the efficacy of specialized CBT, compared with standard CBT, in 34 adolescents with IGD. The specialized CBT program comprised six modules: psychoeducation, standard CBT intervention, intrapersonal, interpersonal, family, and development of a new lifestyle. Both groups exhibited a significant reduction in IGD severity and gaming time, but the effect of specialized CBT was superior to that of standard CBT, suggesting that CBT with an integrative focus may be more effective in reducing IGD symptoms than CBT focusing on IGD only. This treatment effect was stable only in the specialized CBT group at the three month follow-up.
In a study by Zhang et al. [79], the effects of a six-session craving behavioral intervention (CBI) were compared with no intervention, in 40 subjects with IGD. IGD severity was assessed using the Chen Internet Addiction Scale (CIAS). The results revealed significantly lower CIAS scores, less gaming time, and decreased craving for gaming in the CBI group compared with that in the control group. Moreover, analyses of functional magnetic resonance imaging data showed increased activation of the insula in response to gaming cues and decreased insular connectivity with the lingual gyrus and precuneus, in the CBI group. These results indicated that the effect of CBI may result from enhancing cognitive control through a top-down mechanism as well as reducing the salience of the gaming-related cue.
In a study by Yao et al. [80], the efficacy of a six-session, group behavioral intervention (GBI) combining reality therapy and mindfulness meditation was assessed in 18 adults with IGD. The GBI was designed to treat six areas specific to IGD based on the practices and principles of reality therapy and mindfulness meditation, including body relaxation and mindfulness training. After the GBI, IGD severity and depressive and anxiety symptoms were significantly decreased, indicating the effectiveness of GBI in the treatment of IGD and related psychiatric symptoms.
Han et al. [81] compared the effectiveness of CBT with that of supportive therapy in patients with IGD. A total of 101 patients received 14 sessions of CBT, and 104 patients received supportive therapy. In both groups, medication use as monotherapy was allowed to treat comorbidities such as MDD, ADHD, and anxiety disorders. Improvement was defined as a CGI score of less than 4 and a YIAS score of less than 50. The number of patients who showed improvement after the intervention was significantly higher in the CBT group than in the supportive therapy group. Also, the CBT group showed greater reduction of IGD severity, anxiety, impulsivity, and social avoidance.
In a study by Han et al. [82], the efficacy and related neural effects of 12 sessions of CBT were assessed in 20 subjects with IGD. IGD severity was measured using the CIAS. RSFC between the OFC and putamen was significantly lower in the IGD group than in the control group before CBT. CIAS scores and weekly gaming time were significantly reduced in the IGD group after CBT. Increased RSFC between the OFC and putamen was found compared with baseline, suggesting a possible therapeutic mechanism of CBT that could enhance impaired prefrontal-striatal circuits.
Zhang et al. [83] examined the efficacy and related RSFC changes after a six-session CBI versus no intervention in 36 patients with IGD. After 6 weeks of intervention, the CBI group demonstrated significantly lower CIAS scores and weekly gaming time. Moreover, compared with the non-CBI group, the CBI group showed decreased RSFC of the OFC with the hippocampus and parahippocampal gyrus, and a decreased RSFC of the PCC with the supplementary motor area, precentral gyrus, and postcentral gyrus. These findings suggest that CBI may exert therapeutic effects by reducing RSFC between regions within a reward-related network and across the DMN and executive control network.
Liu et al. [84] examined the efficacy of CBI and its association with RSFC in patients with IGD. Twenty patients received six sessions of CBI over a 6-week period, while 16 received no intervention. The results showed greater reductions in CIAS scores and gaming time in the CBI group than in the non-CBI group. CBI was associated with enhanced RSFC within regions in the DMN and decreased RSFC between the DMN and SN, suggesting CBI-related functional network reorganization.
Other treatment modalities
Other treatment modalities besides pharmacotherapy and CBT-based psychotherapy have been applied in the treatment of patients with IGD. In a study by Han et al. [85], five sessions of a brief 3-week family therapy program focusing on increasing family cohesion was associated with significant reductions in IGD severity and gaming time in 15 adolescents with IGD. These results indicate that family cohesion may play an important role in the treatment of IGD. Improvement of family cohesion was associated with increased activity of the caudate nucleus in response to affection stimuli. Sakuma et al. [86] examined the efficacy of a 9-day self-discovery camp (SDC) in 10 patients with IGD. The SDC included 14 sessions of CBT, 8 sessions of personal counseling, 3 medical lectures, outdoor cooking, and trekking. At 3 months after the SDC, gaming time significantly decreased, with a large effect size for hours of gaming/day (d=1.15) and hours of gaming/week (d=1.26). However, the number of days of gaming/week remained consistent. In the RCT by Park et al. [76], eight sessions of VRT were associated with significant decreases in IGD severity. VRT was carried out in three steps: relaxation, simulation of highrisk situations, and sound-assisted cognitive reconstruction. Pallesen et al. [87] evaluated the effect of 13 sessions of an eclectic treatment encompassing CBT, strategic family therapy, solution-focused therapy, and motivational interviewing in 12 adolescents with IGD. After treatment, significant improvements in IGD severity were found in the mother-reported scale but not in patient-reported scales.
The RCT by Kim et al. [88] compared game-based education with general education in a sample of 59 adolescents who were addicted to Massive Multiplayer Online Role-Playing Games (MMORPGs). The game-based group received education consisting of speaking and writing about various aspects of the MMORPG. The control group received the same education, except the content was not related to gaming. After the educational course, which was carried out in 21 sessions over 2 months, the rate of reduction of gaming time was significantly greater in the game-based group than in the control group, with medium treatment effect size (d=-0.49), suggesting that game-based education may be effective in treating patients with IGD. Lee et al. [89] investigated the efficacy of transcranial direct current stimulation (tDCS) over the DLPFC in adults with two or more IGD symptoms. After 12 sessions of tDCS over a period of 4 weeks, IGD severity and gaming time were decreased significantly. 18F-fluoro-deoxyglucose scans revealed that the aberrant asymmetry of regional cerebral glucose metabolism in the DLPFC was partially alleviated, suggesting that the effect of tDCS may result from improving the interhemispheric balance of regional cerebral glucose metabolism. King et al. [90], reported on the efficacy of brief voluntary abstinence in 9 gamers with IGD and 15 gamers without IGD. Significant improvement in IGD symptoms and gaming time occurred in 75% and 38%, respectively, at the 28-day follow-up. Furthermore, a greater rate of reduction in both IGD symptoms and gaming time was found in the IGD group than in the non-IGD group. Pornnoppadol et al. [91] compared the efficacy of four psychosocial interventions in 104 adolescents with IGD and their parents. The interventions included the following: a 7-day residential camp (RC), an 8-session parent management training (PMT), RC combined with PMT, and basic psychoeducation. The reduction in IGD severity was significantly greater in the three active groups than in the basic psychoeducation group at 1, 3, and 6 months post-intervention.
DISCUSSION
This review summarizes the most recent findings of clinical trials using pharmacological and psychosocial treatments for IGD. None of the treatment modalities identified in our review have been studied extensively to confirm their efficacy. Nevertheless, current evidence suggests that specific pharmacological and psychosocial treatments may be effective for IGD.
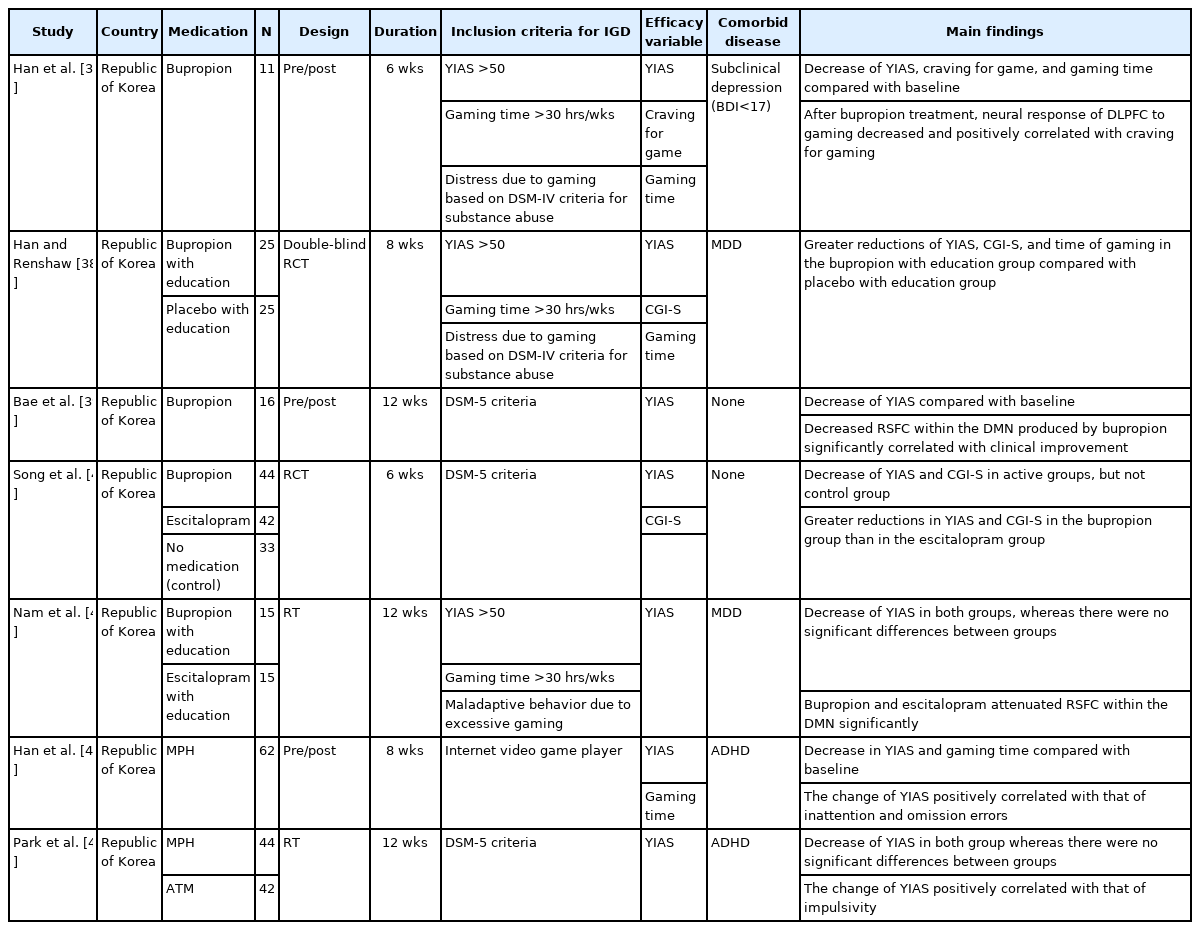
In terms of pharmacotherapy, only two studies employed a randomized design with a control group, which hindered the drawing of conclusions about pharmacological efficacy (Table 1). Bupropion was the most studied drug for IGD. Although there were concerns such as small sample size and short duration, two RCTs [38,40] and three additional studies [37,39,41] reported the efficacy of bupropion consistently. The efficacy of MPH and ATM treatment was also identified in two studies [47,48]; however, their effects have not been compared to those of a placebo. At the neural level, pharmacological studies [37,41] combining functional neuroimaging showed that bupropion attenuated RSFC within the DMN and the SN and the neural response of the DLPFC to gaming cues. The DLPFC and DMN have been implicated in impulse control of substance addiction [92-94]. These neural effects may result from the action of bupropion, which increases dopamine and norepinephrine. Nuclear and genetic studies on IGD have shown the functional impairment of the dopaminergic system, which provides the neurobiological underpinning for the efficacy of dopamine-enhancing drugs such as bupropion and MPH. Collectively, although the number of studies is limited, evidence suggests that bupropion may play a meaningful role in the treatment of IGD. More doubleblind RCTs with larger sample sizes are needed to confirm their efficacy on IGD.
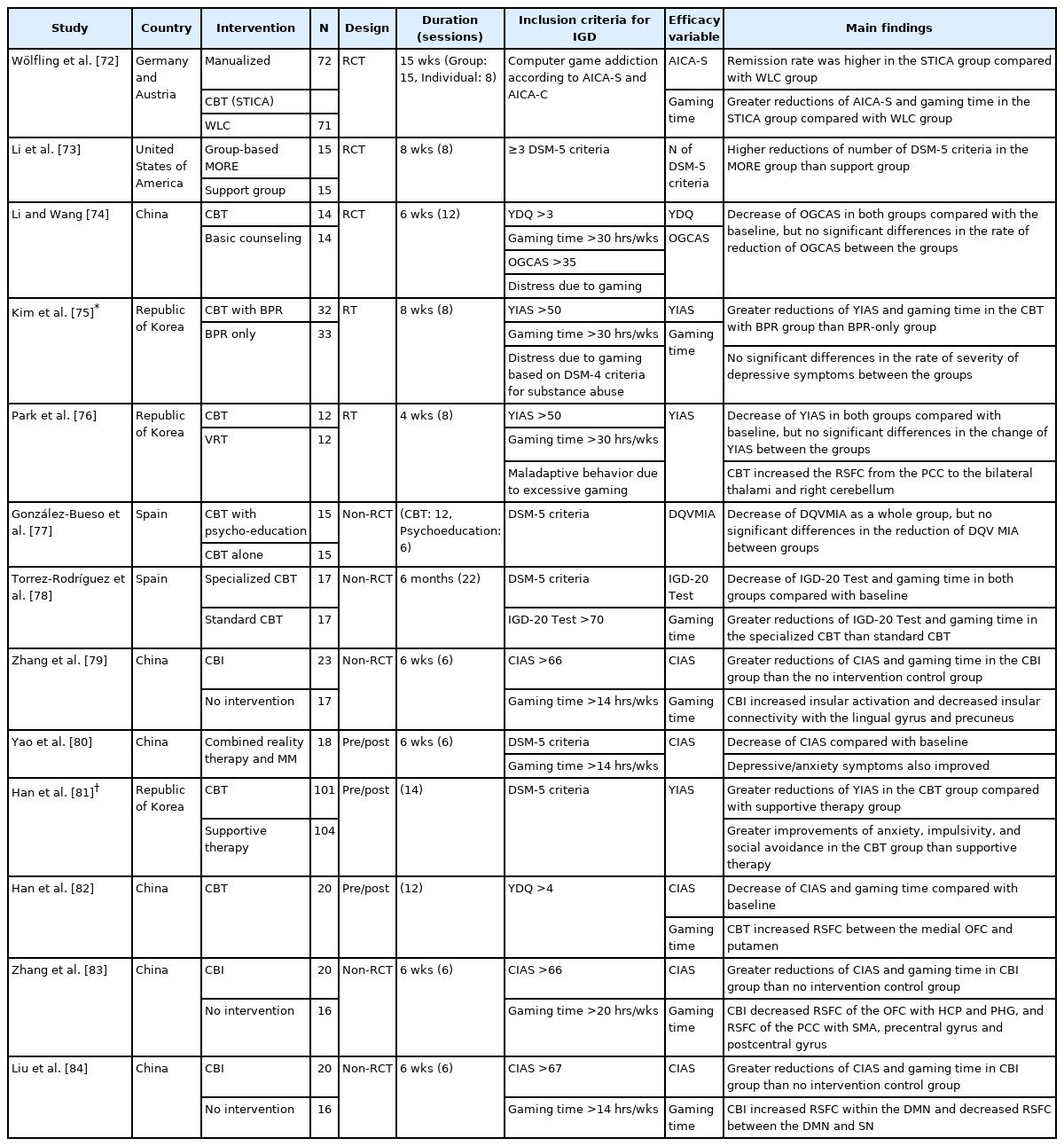
Of the various psychosocial IGD treatments, CBT-based psychotherapy has been studied extensively. Three RCTs and 10 non-RCTs demonstrated that CBT-based intervention significantly reduced IGD symptoms consistently, suggesting that this may be an effective approach for IGD (Table 2). Specifically, three [72,73,75] of the five randomized trials (RTs) for IGD found CBT-based treatment to be superior to the control group. One RCT [72] with a relatively large sample size reported that manualized CBT was more efficacious than WLC, but all subjects were male. The superiority of mindfulness-oriented group therapy over more traditional support groups, and CBT with bupropion over bupropion alone, was found [73,75], but the sample sizes were small. However, the other two RTs [74,76] failed to reveal the superiority of CBT over basic counseling and VRT. This could be due to the fact that both basic counseling and VRT were active therapeutic strategies. At the neural level, CBT enhanced cortical-subcortical circuits [76,82], which may be associated with cognitive control of craving for gaming. Consistent with this, recent models for addiction highlight cortico-subcortical pathology [95]. Furthermore, a meta-analysis of CBT has demonstrated high efficacy in reducing IGD symptoms with a large effect size (g=0.92), but the effect in reducing gaming time is unclear [96]. Additionally, the long-term benefits of CBT have not been evaluated and, according to the currently available data, tend to be maintained only in the short term. More rigorous longitudinal studies are needed to develop evidence-based treatment guidelines for IGD.
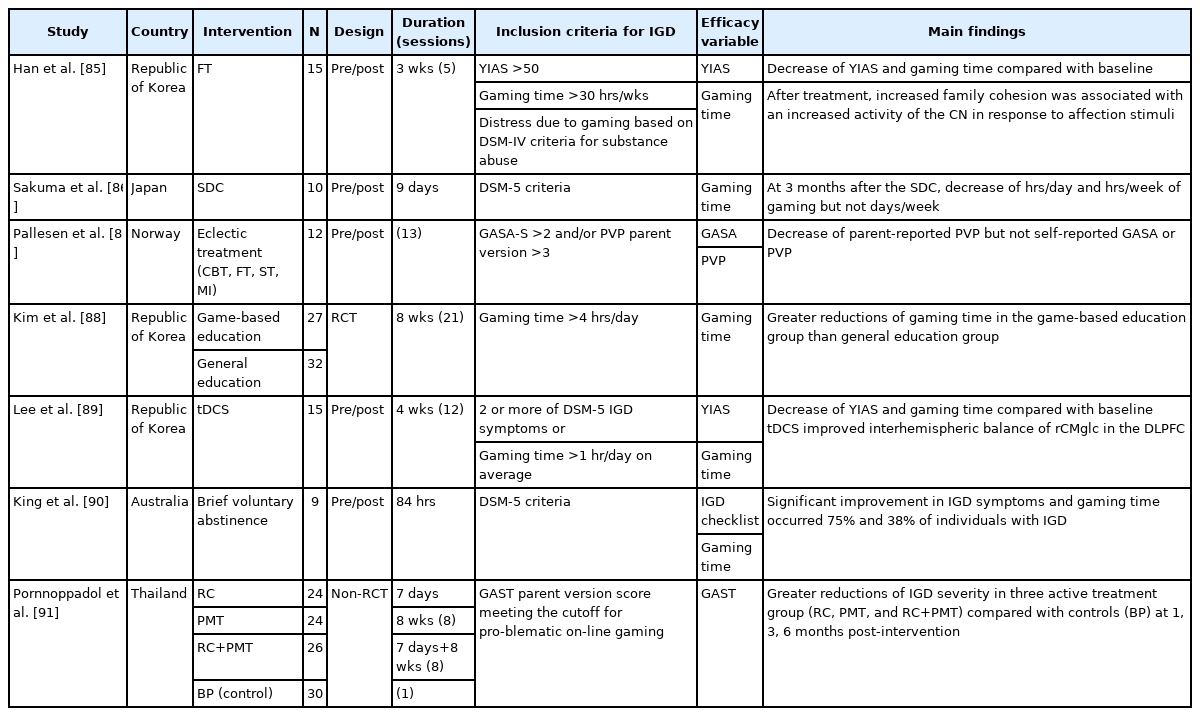
The efficacy of other psychosocial interventions, including family therapy and therapeutic RC, was reported (Table 3) [85,86]. However, the benefits were observed only in small samples and did not include controls. One study [91] demonstrated the superior efficacy of RC, PMT, and RC with PMT over basic psychoeducation, but its design was not randomized. One RCT [88] demonstrated that game-based educational intervention significantly decreased gaming time compared with general education, but the severity of IGD was not evaluated. Although studies using innovative approaches for IGD, ranging from eclectic treatment to VRT, voluntary abstinence, and tDCS, reported somewhat hopeful results [76,87,89,90], these studies had limitations such as the absence of control groups and small sample sizes. Additional RCTs with larger sample sizes are required to confirm these as an evidence-based treatments for IGD.
One of the major concerns regarding IGD treatment studies is that the inclusion criteria for IGD are not consistent across studies. Only 9 of the 27 studies reviewed here used DSM-5 criteria to diagnose IGD [39,40,48,77,78,80,81,86,90]. In some studies [37,38,41,75,76,85], inclusion criteria for IGD were based on YIAS scores and gaming time. Since the YIAS was designed to measure Internet overuse, items of the YIAS are not specific to IGD symptoms [6]. Nonetheless, only one study had disclosed that the word “Internet” was modified to “on-line games” to assess IGD symptoms [89]; most of studies did not mention this, which means that individuals with IA might have been incorrectly determined as having IGD. In terms of efficacy, all studies used selfreport scales; however, self-report scales have the problem of subjectivity and may not accurately evaluate gaming behavior. The development of a validated diagnostic interview and objective rating scale based on DSM-5 criteria is needed for precise and reliable diagnosis and evaluation of the treatment response. Future studies using standard assessment tools may enable us to meaningfully compare the results across studies. About three-fourths of the studies reviewed were conducted in Northeast Asia, limiting their generalizability to other cultures. Because cultural gaps may influence the acceptability of specific treatment approaches, a larger number of studies across countries would be required to examine cross-cultural differences. Since craving may play an important role in the development and maintenance of IGD, therapeutic interventions that help individuals with IGD to cope with and to reduce craving may contribute to positive therapeutic outcomes and prevent relapse. Among various CBT-based interventions, CBI has shown a significant reduction in craving for gaming and IGD severity [83,84]. Meanwhile, interventions designed to reduce withdrawal have not been applied in the treatment of IGD. In a study by Kaptsis et al. [97], patients with IGD experienced the largest reduction in withdrawal symptoms within the first 24 h, suggesting that it is unlikely that withdrawal intensifies during the initial period of abstinence. Future research on the long-term course of gaming withdrawal could broaden our knowledge regarding the role of withdrawal in the treatment and relapse of IGD. Furthermore, controversy remains about whether IGD is an independent mental disorder. In most pharmacological trials for IGD, the participants had one comorbidity, such as depression or ADHD. Given the high level of comorbidity, there is a possibility that the treatment effect may result from the improvement of comorbid conditions. If IGD is better explained by comorbid disorders, treatment strategies focusing on these conditions need to be considered. Finally, there have been few studies on the natural progression of IGD and the factors associated with recovery or relapse, which have important implications in IGD treatment. In a review of 13 longitudinal studies, the course of IGD was variable but tended to be more stable in adolescents than adults, implying that age may partially affect the clinical progression of IGD [98]. A recent longitudinal cohort study reported that older age and fewer symptoms of depression and ADHD were associated with long-term recovery from IGD. Younger IGD patients and those with higher levels of family and social support showed improved initial engagement and response to treatment, suggesting that age, family, and social factors should be considered in IGD treatments. Previous studies have reported that the prognosis of IGD is associated with family cohesion as well as gaming-related cognitions [85,99,100]. These studies have several limitations, including small sample sizes, inconsistent criteria of IGD, and relatively short follow-up periods. Ongoing basic research and clinical trials overcoming the above-mentioned limitations could broaden our understanding of IGD and contribute to the development of evidence-based treatments.
Notes
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
Conflicts of Interest
Seon-Cheol Park, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Hyung-Jun Yoon. Investigation: all authors. Writing—original draft: Eun Hyun Seo, Hae-Jung Yang, Hyung-Jun Yoon. Writing—review & editing: all authors.
Funding Statement
None