Interactions Between Depression, Alcohol Intake, and Smoking on the Risk of Acute Coronary Syndrome
Article information
Abstract
Objective
Our study hypothesizes that the interaction between depression, alcohol intake, and smoking status can significantly influence the risk of acute coronary syndrome (ACS). We aim to investigate the magnitude of the association between depression and ACS risk and explore how alcohol intake and smoking status affect this association.
Methods
We used data from the Korean Genome and Epidemiology Study. The primary exposure of interest was the presence of depression, as measured using the Beck Depression Inventory score at baseline. The primary outcome was the occurrence of ACS observed in the biennial follow-up surveys. We used Cox proportional regression analysis to estimate the effect of depression on ACS incidence. We conducted interaction and joint effect analyses to explore the interactions between depression and health-related habits including alcohol intake and smoking with regard to ACS incidence.
Results
During 16 years of follow-up among 3,254 individuals, we documented 88 cases of new-onset ACS (2.2 cases per 1,000 personyears). We found no association between depression and ACS risk; furthermore, the effect of depression on ACS risk by alcohol intake and smoking status did not differ significantly. In the analysis to observe the joint effect of smoking and depression, the multivariate hazard ratios of ACS were 1.26 (95% confidence interval [CI], 0.67–2.36) for non-smoking and depression, 1.52 (95% CI, 0.83–2.82) for smoking and non-depression, and 2.79 (95% CI, 1.21–6.41) for smoking and depression compared with non-smoking and non-depression.
Conclusion
Our study reveals the combined effect of depression and smoking on ACS risk, highlighting the potential benefits of concurrent interventions for both depression and smoking for cardiovascular health.
INTRODUCTION
Acute coronary syndrome (ACS) is the most common manifestation of cardiovascular disease and represents a significant global health burden, contributing to approximately 17.8 million deaths worldwide annually [1,2]. ACS has been widely studied in clinical and epidemiologic research studies. Both non-modifiable cardiovascular risk factors, including age, sex, genetic predisposition, and ethnicity and modifiable risk factors, such as high blood pressure, obesity, smoking, alcohol use, physical inactivity, dyslipidaemia, inflammation, diabetes, metabolic syndrome, and undetected ACS, contribute to increased cardiovascular risk [3-5]. Identifying modifiable risk factors of ACS is critical to developing effective preventive strategies and reducing its worldwide health burden [6,7].
Depression, a prevalent and debilitating mental health disorder, affects more than 264 million people worldwide [8,9]. The association between depression and ACS receives increasing attention, with numerous studies demonstrating a substantial link between the two conditions [10,11]. Moreover, depression is associated with poor prognosis and increased mortality in individuals with existing ACS [12].
Lifestyle factors, such as alcohol intake and smoking, are well-established risk factors of ACS [13,14]. Both alcohol consumption and smoking have complex associations with ACS risk, with the former exhibiting a J-shaped association [15] and the latter demonstrating a dose-dependent relationship [16]. Although the effect of these factors on ACS risk has been extensively studied, their interactions with depression with regard to ACS risk remain less explored.
Depression can also significantly affect an individual’s alcohol intake and smoking habits, often leading to unhealthy behaviors that exacerbate mental health challenges and overall health risks. Individuals with depression are more likely to consume alcohol as a self-medication to alleviate negative emotions and cope with the symptoms [17]. However, this can result in a vicious cycle, as excessive alcohol consumption can further disrupt the brain’s neurotransmitter balance and exacerbate depressive symptoms [18]. Similarly, individuals with depression may turn to smoking as a coping mechanism given the temporary mood-enhancing effects of nicotine [19]. By exploring the effect of depression on alcohol intake and smoking within the context of the risk of coronary artery disease, we aim to improve the understanding of these complex interactions, which would inform targeted interventions and preventive strategies. Our study hypothesizes that the interaction between depression, alcohol intake, and smoking status can significantly influence the risk of ACS. We aim to investigate the magnitude of the association between depression and ACS risk and explore how alcohol intake and smoking status affect this association.
METHODS
Study design and data sources
The Korea Genome and Epidemiology Study (KoGES) is a large-scale, population-based cohort study initiated to understand the genetic and environmental factors associated with common, complex diseases in the Korean population. The primary objectives of the KoGES are to identify the prevalence, incidence, and risk factors for chronic non-communicable diseases, including cardiovascular diseases, diabetes, and obesity. Detailed methodologies, recruitment strategies, and baseline characteristics of the study participants can be found in the references provided [20]. The KoGES initiated 2 independent prospective cohort studies in 2001 conducted in 2 cities: Ansung, a rural community with a population of 175,824 (based on the 2010 census) and Ansan, an urban community with a population of 714,891 (based on the 2010 census). Each cohort comprised a population sample of Korean men and women aged 40–69 years with the same ethnicity. Detailed information on the sampling plan and selection criteria for these ongoing prospective studies has been published previously [20,21]. Between 2001 and 2002, we identified 7,129 eligible participants in Ansung and 10,957 participants in Ansan. In total, 5,018 (2,239 men and 2,779 women) participants from Ansung and 5,020 (2,523 men and 2,497 women) participants from Ansan completed a baseline examination in their respective cities. Cohort participants underwent follow-up examinations until the end of the cohort study (9th follow-up examination from 2019 to 2020).
All interviewers are trained every 2 years using a standardised protocol. Cohort members are followed up biennially with a scheduled site visit. Trained interviewers conducted face-to-face interviews every two years to collect participant data. During these interviews, participants provided direct responses about various health factors. Specifically, the statuses of smoking and alcohol consumption were based on participants’ self-reported responses during these interviews.
Study population and definition of coronary artery disease
KoGES data included biennial follow-up assessments of patient information, beginning with the baseline survey in 2001–2002. However, the use of the Beck Depression Inventory (BDI), a measure of depression, started in 2005–2006 during the second follow-up period. Therefore, our study designated the second follow-up period (2005–2006) as the baseline for this investigation and considered the third follow-up of KoGES as the first follow-up study in our analysis.
For the analysis, we excluded participants who did not complete the BDI questionnaire or whose alcohol intake and smoking status were not reported by 2005–2006 (the baseline period for our study). We also excluded participants with physician-diagnosed ACS including myocardial infarction or angina pectoris at the baseline.
In this study, ACS was defined as myocardial infarction or angina pectoris diagnosed during the biennial follow-up assessments conducted from 2007 to 2020.
Depression and other potential risk factors
Participants completed an interviewer-administered questionnaire. The questionnaires administered during 2005–2006 collected information on BDI, which is a widely-used self-report questionnaire designed to assess the presence and severity of depressive symptoms [22]; demographic characteristics, including age, sex, marital status, and education level; and health-related factors including smoking status, alcohol intake, and physical activity.
Depression was categorized based on the BDI scores. Participants were classified into 4 categories: no or slight depression (0–13), mild depression (14–19), moderate depression (20–28), and severe depression (29–63) [23,24]. At the time of the survey, alcohol intake was assessed by determining whether participants were drinkers or non-drinkers. Smoking status was categorized into non-smokers, former smokers, and regular smokers based on participants’ self-reported smoking habits during the survey period.
Statistical analysis
We calculated the descriptive statistics for the baseline characteristics of study participants by the categories of depression. Baseline characteristics of KoGES participants were compared using the Wilcoxon rank sum test for continuous variables and the chi-square test for categorical variables. The crude 15-year (2005–2020) incidence rates of ACS were calculated as the number of at-risk cases per 1,000 person-years based on the presence of depression and health-related habits including alcohol intake and smoking. Thereafter, hazard ratios (HRs) and 95% confidence intervals (CIs) from Cox proportional hazards regression models with fixed covariates (with the nondepression group as the reference group) were used to estimate relative risks for 15-year cumulative ACS incidence based on baseline depression and health-related habits including alcohol intake and smoking. For our primary analysis using the Cox proportional hazards regression model, we assessed the proportional hazards assumption using Schoenfeld residuals. Diagnostic plots and tests confirmed that the assumption was met for the variables in the model. A multivariate logistic regression analysis was performed to estimate the effect of depression on the incidence of ACS after adjusting for potential confounders. Furthermore, we used the interaction term for depression and health-related habits including alcohol intake and smoking into the multivariate logistic regression model to estimate the effect of changes in depression by alcohol intake and smoking status on the study outcomes. To reduce the number of subgroups created for the analysis of the joint effects, we combined 3 depression groups such as mild depression, moderate depression, and severe depression, and compared the depression and non-depression groups. We tested the multi-collinearity among the covariates in the model. All statistical analyses were performed using SAS software (version 9.4; SAS Institute Inc., Cary, NC, USA).
Ethics approval and consent to participate
The study protocol was reviewed and approved by the Institutional Review Board of Chonnam National University Hospital (CNUH-2018-297). The requirement for informed consent from patients was waived because the study was a retrospective analysis of existing data.
RESULTS
Demographic findings
During the 16 years of follow-up among 3,254 individuals, we documented 88 cases of new-onset ACS including myocardial infarction and angina pectoris (2.2 cases per 1,000 person-years). The study population was stratified based on the BDI scores into 4 groups: no or slight depression (BDI score: 0–13) (n=2,631, 80.9%), mild depression (BDI score: 14–19) (n=334, 10.3%), moderate depression (BDI score: 20–28) (n=168, 5.2%), and severe depression (BDI score: 29–63) (n=121, 3.7%). The characteristics of the study participants across these categories are summarised in Table 1. The mean age across the groups did not differ significantly. However, the proportion of women was higher in the moderate and severe depression groups (45.7%, 55.1%, 63.1%, and 57.9% in none or slight, mild, moderate, and severe depression group). Comorbidities including hypertension and diabetes mellitus did not differ across groups. Regarding health-related behaviours, the proportion of never smokers increased as depression severity increased (58.1%, 61.7%, 65.5%, and 66.1% in none or slight, mild, moderate, and severe depression group). As the severity of depression increased, the likelihood of having an education period of 9 years or longer decreased (p<0.01). Additionally, the average sleep duration tended to increase with the increasing severity of depression (p<0.01).
Main outcomes
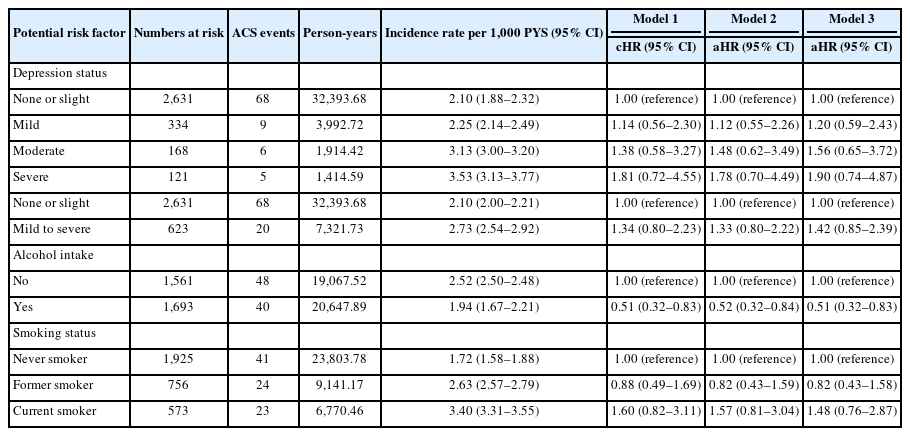
Table 2 summarises the association between depression and ACS. Depression severity had no association with ACS risk when no or slight depression was used as the reference (mild: 1.20 [0.59–2.43], moderate: 1.56 [0.65–3.72], and severe: 1.90 [0.74–4.87]). Analyses stratified by alcohol intake and smoking were conducted for the association between depression and ACS, and no significant difference in the effect of depression on the risk of ACS based on alcohol intake and smoking status was observed (Table 3).

Multivariate analysis stratified by alcohol intake and smoking for the association between depression and ACS
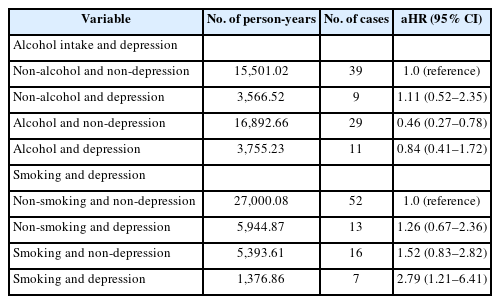
Table 4 summarises the combined effects of depression and other risk factors including alcohol intake and smoking. In the analysis for smoking and depression, the multivariate HRs of ACS were 1.26 (95% CI, 0.67–2.36) for non-smoking and depression, 1.52 (95% CI, 0.83–2.82) for smoking and non-depression, and 2.79 (95% CI, 1.21–6.41) for smoking and depression compared with non-smoking and non-depression. However, no significant association was observed in the analysis for the joint effect of alcohol intake and depression.
DISCUSSION
Using the prospective cohort study, we studied the effect of depression on the risk of ACS onset and how this effect varies with alcohol intake and smoking status. The Cox proportional hazards regression analysis did not identify depression, alcohol intake, and smoking as independent risk factors for ACS. However, when considering the combined effects, the presence of depression and a smoker status significantly increased the risk for ACS compared to the absence of these 2 factors. These findings suggest that although depression and smoking may not independently influence the risk of ACS, their simultaneous presence could increase ACS risk.
Smoking is a well-known risk factor for ACS as it accelerates atherosclerosis, induces vascular constriction, and increases platelet aggregation [25,26]. In contrast to previous findings, we did not find a significant increase in the risk of ACS associated with smoking. Previous studies have illustrated a complex association between alcohol intake and ACS, with moderate drinking often associated with reduced risk, a phenomenon known as the “French Paradox,” whereas excessive intake was associated with increased risk [27,28]. Our study aligns with these findings, showing a reduced ACS risk associated with alcohol intake. However, we did not consider the quantity of alcohol consumed, which makes direct comparison of our results with those of previous studies that considered moderate consumption challenging.
Previous studies have consistently identified depression as a significant risk factor for the development of ACS [29-31]. This is hypothesized to be because of a combination of direct biological effects of depression on heart function, such as increased inflammation and hormonal imbalance, and behavioral effects such as poor diet, lack of exercise, and poor adherence to medical treatment [32]. However, the exact mechanism linking depression and ACS remains to be understood. Contrary to the findings of previous studies, our study demonstrated that the presence and severity of depression did not increase the risk of ACS. These results suggest that the effect of depression on ACS risk may be more nuanced and multifactorial than previously understood. Although several studies have assessed the individual effects of depression, alcohol intake, and smoking on the risk of ACS, those studying the associations between depression and alcohol intake or smoking on ACS risk are few.
We found that the combination of depression and smoking significantly increased the risk of ACS. This outcome can be theoretically supported by the biological stress theory and the health behavior theory. The biological stress theory posits that both depression and smoking elevate stress response, subsequently increasing the risk of cardiovascular disease. This increased stress places an increased burden on the heart, potentially increasing the risk of ACS. The health behavior theory suggests that depression and smoking can impede the formation and maintenance of healthy lifestyle habits. In particular, individuals with depression who engage in smoking are less likely to develop behaviors that reduce the risk of ACS, such as smoking cessation, regular exercise, and a healthy diet. These factors can increase ACS risk. In addition to these theories, physiological interactions between depression and smoking can also play a role. Smoking is known to activate the nervous system, constrict blood vessels, and increase blood pressure. Furthermore, depression has been associated with reduced blood flow to the heart and increased inflammation within blood vessels. The concurrent presence of these conditions can mutually exacerbate their negative effects, increasing the risk of ACS.
Our findings highlight the complex interactions among depression, smoking, alcohol intake, and the risk of ACS. Although these factors may not independently contribute to the risk of ACS, their coexistence could significantly increase the risk of ACS. This evidence underlines the need for a comprehensive health management approach that concurrently addresses both depression and smoking status, indicating the need for focused attention for individuals with depression and a smoking habit. Further research should aim to elucidate the mechanisms underlying these interactions and suggest tailored interventions to mitigate the risk of ACS in this at-risk population.
Our study has several limitations. First, although this study is a prospective cohort study and had the strength of observing the natural progression of events, it lacked the robustness of a randomized controlled trial in establishing a causal association. Second, the status of depression, alcohol intake, and smoking were based on self-reporting, which may have introduced biases. Social desirability bias could have resulted in underreporting of smoking and alcohol intake. Third, we did not account for the quantity and duration of alcohol intake and smoking, which could significantly affect the observed associations. This may have caused a misclassification or under-or over-estimation of the effects of these variables on ACS risk. Fourth, the main outcome of this study, ACS, did not distinctly differentiate between stable angina, unstable angina, and myocardial infarction in terms of severity. The absence of such differentiation may limit specific insights into how each ACS subtype relates to depression, alcohol intake, and smoking. Fifth, though depression was segmented into 4 categories for the purpose of our analysis, it is important to recognize the limitations posed by the joint test that simplifies it into just 2 broad categories. This dichotomous categorization might not capture the nuances and intricacies of the varying levels of depression. Sixth, although we made statistical adjustments, the risk of biases due to unobserved or unmeasured confounding variables does exist. Finally, as the KoGES dataset is confined to a specific population group, the generalizability of our results may be limited. The association observed in our study may manifest differently in other population groups.
In conclusion, our study shows that depression and smoking have a combined effect on the ACS risk. This finding underscores the importance of simultaneous treatment of depression and smoking to improve heart health and the need for further research in this field.
Notes
Availability of Data and Material
Data in this study were from the Korean Genome and Epidemiology Study (KoGES; 6635-302), National Institute of Health, Korea Disease Control and Prevention Agency, Republic of Korea.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Eujene Jung, Hyun Ho Ryu. Data curation: Eujene Jung, Hyun Ho Ryu, Young Ju Cho. Formal analysis: Eujene Jung, Hyun Ho Ryu, Byeong Jo Chun. Funding acquisition: Eujene Jung, Hyun Ho Ryu. Investigation: Eujene Jung. Methodology: Hyun Ho Ryu. Project administration: Eujene Jung, Hyun Ho Ryu. Resources: Eujene Jung, Hyun Ho Ryu. Software: Eujene Jung, Hyun Ho Ryu. Supervision: Hyun Ho Ryu. Validation: Eujene Jung. Visualization: Eujene Jung. Writing—original draft: Eujene Jung. Writing—review & editing: Hyun Ho Ryu.
Funding Statement
This work was supported by research programmes funded by the Korea Centers for Disease Control and Prevention (contract numbers: 2001-347-6111-221, 2002-347-6111-221, 2003-347-6111-221, 2004-E71001-00, 2005-E71001-00, 2006-E71005-00, 2006-E71006-00, 2007-E71001-00, 2007-E71003-00, 2008-E71001-00, 2008-E71005-00, 2009-E71002-00, 2009-E71007-00, 2010-E71001-00, 2010-E71004-00, 2011-E71004-00, 2011-E71008-00, 2012-E71008-00, 2012-E71005-00, 2013-E71007-00, 2013-E71005-00, 2014-E71005-00, and 2014-E71003-00).