1. Roohafza H, Feizi A, Afshar H, Mazaheri M, Behnamfar O, Hassanzadeh-Keshteli A, et al. Path analysis of relationship among personality, perceived stress, coping, social support, and psychological outcomes. World J Psychiatry 2016;6:248-256.



2. Suldo SM, Shaunessy E, Hardesty R. Relationships among stress, coping, and mental health in high-achieving high school students. Psychol Sch 2008;45:273-290.

3. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385-396.


4. Hammen C. Stress and depression. Annu Rev Clin Psychol 2005;1:293-319.


5. Monroe SM, Hadjiyannakis K. The Social Environment and Depression: Focusing on Severe Life Stress. In: Gotlib IH, Hammen CL, editor. Handbook of Depression. New York, NY: The Guilford Press, 2002, p. 314-340.
6. Paykel ES. Life events and affective disorders. Acta Psychiatr Scand Suppl 2003;(418):61-66.


8. Beck AT, Haigh EAP. Advances in cognitive theory and therapy: the generic cognitive model. Annu Rev Clin Psychol 2014;10:1-24.


9. Disner SG, Beevers CG, Haigh EA, Beck AT. Neural mechanisms of the cognitive model of depression. Nat Rev Neurosci 2011;12:467-477.


10. Vollrath M, Torgersen S. Personality types and coping. Pers Individ Dif 2000;29:367-378.

11. Wang SM, Lai CY, Chang YY, Huang CY, Zauszniewski JA, Yu CY. The relationships among work stress, resourcefulness, and depression level in psychiatric nurses. Arch Psychiatr Nurs 2015;29:64-70.


13. Guo L, Zauszniewski JA, Liu Y, Yv S, Zhu Y. Is resourcefulness as a mediator between perceived stress and depression among old Chinese stroke patients? J Affect Disord 2019;253:44-50.


14. Huh HJ, Kim SY, Min JA, Chae JH. Development of the Clinical Short-Form Positive Resources Test. Korean J Str Res 2018;26:77-87.

15. Zauszniewski JA. Self-help and help-seeking behavior patterns in healthy elders. J Holist Nurs 1996;14:223-226.


16. Zauszniewski JA. Learned resourcefulness: a conceptual analysis. Issues Ment Health Nurs 1995;16:13-31.


17. Lai CY, Zauszniewski JA, Tang TC, Hou SY, Su SF, Lai PY. Personal beliefs, learned resourcefulness, and adaptive functioning in depressed adults. J Psychiatr Ment Health Nurs 2014;21:280-287.


18. Chen MC, Palmer MH, Lin SY. Creating a conceptual model for family caregivers of older adults intervention research: a narrative review of learned resourcefulness, resourcefulness, and the transtheoretical model. Geriatr Nurs 2018;39:521-527.


19. Bekhet AK, Zauszniewski JA. The effect of a resourcefulness training intervention on relocation adjustment and adaptive functioning among older adults in retirement communities. Issues Ment Health Nurs 2016;37:182-189.


20. Bekhet AK, Zauszniewski JA. Resourcefulness, positive cognitions, relocation controllability and relocation adjustment among older people: a cross-sectional study of cultural differences. Int J Older People Nurs 2013;8:244-252.


21. Huang CY, Guo SE. Stress, perceived support, resourcefulness and depressive symptoms in Taiwanese adolescents. J Clin Nurs 2009;18:3271-3279.


22. Huang CY, Sousa VD, Tu SY, Hwang MY. Depressive symptoms and learned resourcefulness among Taiwanese female adolescents. Arch Psychiatr Nurs 2005;19:133-140.


23. Boonpongmanee C, Zauszniewski JA, Morris DL. Resourcefulness and self-care in pregnant women with HIV. West J Nurs Res 2003;25:75-92.


24. Huang CY, Guo SE, Hung CM, Shih SL, Lee LC, Hung GC, et al. Learned resourcefulness, quality of life, and depressive symptoms for patients with breast cancer. Oncol Nurs Forum 2010;37:E280-287.


25. Huang CY, Perng SJ, Chen HF, Lai CY. The impact of learned resourcefulness on quality of life in type II diabetic patients: a cross-sectional correlational study. J Nurs Res 2008;16:264-274.


26. Min JA, Jung YE, Kim DJ, Yim HW, Kim JJ, Kim TS, et al. Characteristics associated with low resilience in patients with depression and/or anxiety disorders. Qual Life Res 2013;22:231-241.


27. Min JA, Lee CU, Hwang SI, Shin JI, Lee BS, Han SH, et al. The moderation of resilience on the negative effect of pain on depression and post-traumatic growth in individuals with spinal cord injury. Disabil Rehabil 2014;36:1196-1202.


29. Aiken LS, West SG, Reno RR. Multiple regression: Testing and interpreting interactions. sage; 1991.
30. Cohen J, Cohen P, West SG, Aiken LS. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. New York: Routledge; 2013.
31. SH L, YJ H, JH K, CS H. Finding optimal cut off points of the Korean Version of the Patient Health Questionnaire-9(PHQ-9) for screening depressive disorders. Mood Emot 2014;12:32-36.
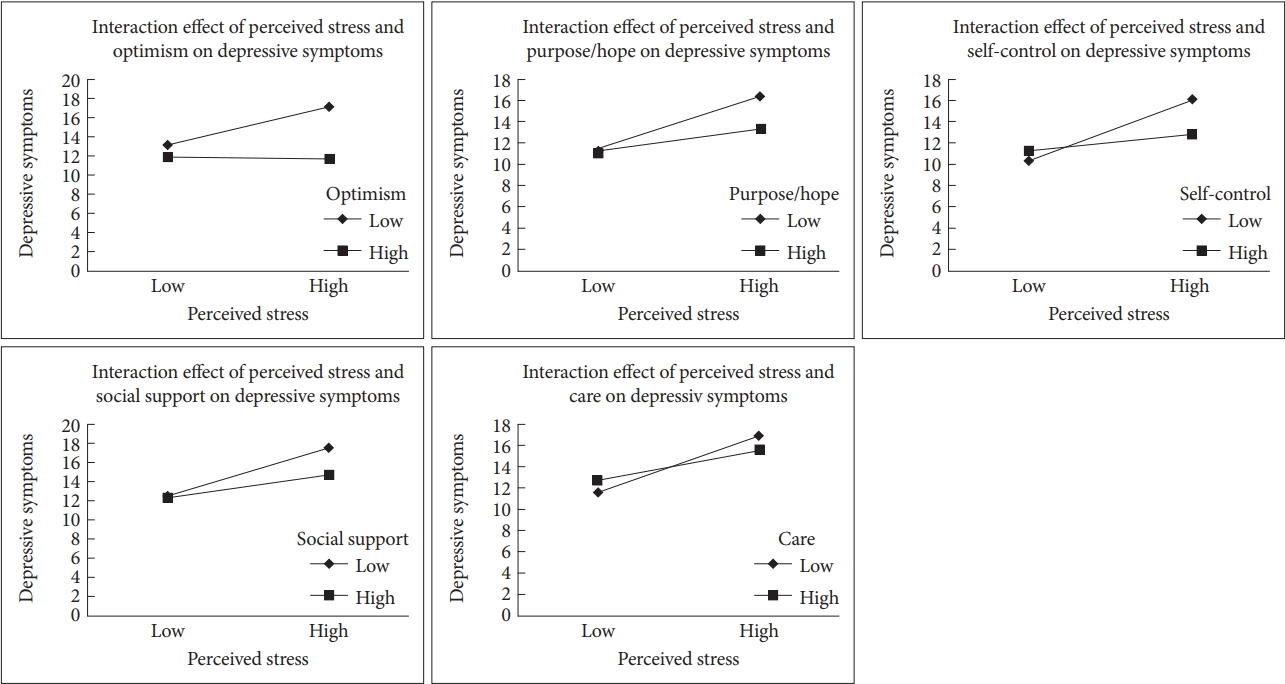
33. Thomas JL, Britt TW, Odle-Dusseau H, Bliese PD. Dispositional optimism buffers combat veterans from the negative effects of warzone stress on mental health symptoms and work impairment. J Clin Psychol 2011;67:866-880.


34. Vollmann M, Scharloo M, Langguth B, Kalkouskaya N, Salewski C. Illness representations as mediators of the relationship between dispositional optimism and depression in patients with chronic tinnitus: a cross-sectional study. Psychol Health 2013;29:81-93.


35. Tyser J, Scott WD, Readdy T, McCrea SM. The role of goal representations, cultural identity, and dispositional optimism in the depressive experiences of American Indian youth from a Northern Plains tribe. J Youth Adolesc 2014;43:329-342.


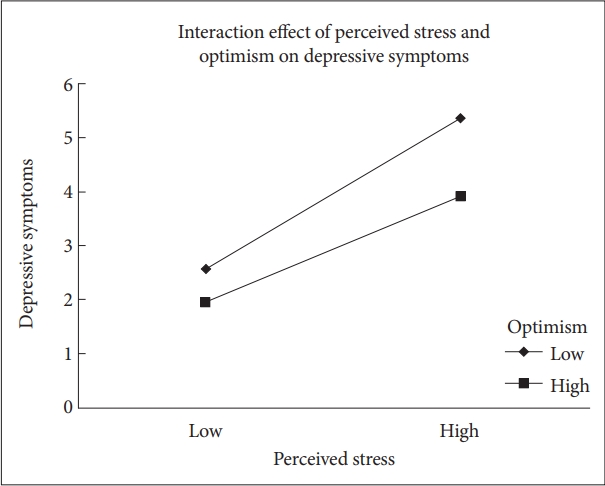
36. Liu B, Pu J, Hou H. Effect of perceived stress on depression of Chinese “Ant Tribe” and the moderating role of dispositional optimism. J Health Psychol 2016;21:2725-2731.


37. Breton JJ, Labelle R, Berthiaume C, Royer C, St-Georges M, Ricard D, et al. Protective factors against depression and suicidal behaviour in adolescence. Can J Psychiatry 2015;60:S5-S15.
39. Horwitz AG, Berona J, Czyz EK, Yeguez CE, King CA. Positive and negative expectations of hopelessness as longitudinal predictors of depression, suicidal ideation, and suicidal behavior in high-risk adolescents. Suicide Life Threat Behav 2017;47:168-176.


40. Martela F, Steger MF. The three meanings of meaning in life: distinguishing coherence, purpose, and significance. J Posit Psychol 2016;11:531-545.

41. Beck R, Perkins TS. Cognitive content-specificity for anxiety and depression: A meta-analysis. Cognit Ther Res 2001;25:651-663.
42. Steger MF. Meaning in Life. In: Lopez SJ, Snyder CR, editor. Oxford Handbook of Positive Psychology. 2nd Ed. New York, NY: Oxford University Press, 2009, p. 679-687.
43. Joormann J, Stanton CH. Examining emotion regulation in depression: a review and future directions. Behav Res Ther 2016;86:35-49.


45. Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev 2010;30:217-237.


46. Liu DY, Thompson RJ. Selection and implementation of emotion regulation strategies in major depressive disorder: an integrative review. Clin Psychol Rev 2017;57:183-194.


47. Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annu Rev Clin Psychol 2005;1:255-291.


48. Travis LA, Lyness JM, Shields CG, King DA, Cox C. Social support, depression, and functional disability in older adult primary-care patients. Am J Geriatr Psychiatry 2004;12:265-271.


49. Oxman TE, Hull JG. Social support and treatment response in older depressed primary care patients. J Gerontol B Psychol Sci Soc Sci 2001;56:P35-P45.


50. Bisschop MI, Kriegsman DM, Beekman AT, Deeg DJ. Chronic diseases and depression: the modifying role of psychosocial resources. Soc Sci Med 2004;59:721-733.


51. Kupferberg A, Bicks L, Hasler G. Social functioning in major depressive disorder. Neurosci Biobehav Rev 2016;69:313-332.


53. Schwartz C, Meisenhelder JB, Ma Y, Reed G. Altruistic social interest behaviors are associated with better mental health. Psychosom Med 2003;65:778-785.


54. Anderson NB. Emotional Longevity: What Really Determines How Long You Live. New York, NY: Penguin Press; 2003.
55. Kalamatianos A, Canellopoulos L. A diathesis-stress model conceptualization of depressive symptomatology. Psychiatriki 2019;30:49-57.


56. Blatt SJ. Experiences of Depression: Theoretical, Clinical, and Research Perspectives. Washington, DC: American Psychological Association; 2004.