|
 |
- Search
| Psychiatry Investig > Volume 18(5); 2021 > Article |
|
Abstract
Objective
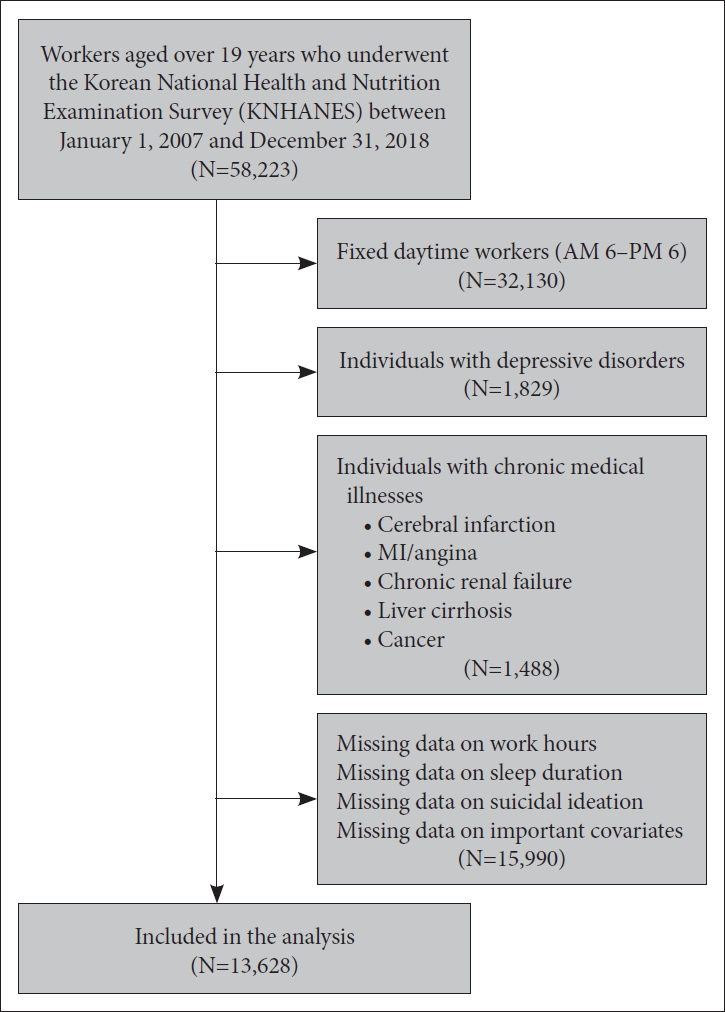
Methods
Results
The authors have no potential conflicts of interest to disclose.
AuthorsŌĆÖ contribution
Conceptualization: Sun-Young Kim. Data curation: Sun-Young Kim. Formal analysis: Sun-Young Kim. Funding acquisition: Weon-Jeong Lim. Investigation: Sun-Young Kim. Methodology: Sun-Young Kim. Project administration: Weon-Jeong Lim, Soo In Kim. Resources: Sun-Young Kim. Software: Sun-Young Kim. Supervision: Soo In Kim. Validation: Sun-Young Kim. Visualization: Sun-Young Kim. WritingŌĆöoriginal draft: Sun-Young Kim. WritingŌĆöreview & editing: Sun-Young Kim, Soo In Kim.
Table┬Ā1.
Table┬Ā2.
Table┬Ā3.
| Sleep duration (hours/day) |
Model 1* |
Model 2ŌĆĀ |
Model 3ŌĆĪ |
Model 4┬¦ |
Model 5Ūü |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Categorical sleep duration | ||||||||||
| ŌĆā<6 | 1.50 (1.29-1.75) | <0.001 | 1.43 (1.23-1.68) | <0.001 | 1.55 (1.32-1.82) | <0.001 | 1.52 (1.29-1.78) | <0.001 | 1.36 (1.15-1.60) | <0.001 |
| ŌĆā6 to <7 | 1.13 (0.99-1.29) | 0.067 | 1.17 (1.02-1.34) | 0.024 | 1.20 (1.05-1.37) | 0.009 | 1.18 (1.03-1.35) | 0.016 | 1.14 (0.99-1.32) | 0.060 |
| ŌĆā7 to <9 | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] | |||||
| ŌĆā9 to <10 | 1.07 (0.80-1.43) | 0.640 | 0.94 (0.70-1.26) | 0.692 | 1.03 (0.76-1.38) | 0.866 | 1.04 (0.77-1.40) | 0.809 | 1.01 (0.74-1.37) | 0.956 |
| ŌĆāŌēź10 | 1.74 (1.30-2.34) | <0.001 | 1.45 (1.07-1.95) | 0.015 | 1.54 (1.14-2.08) | 0.005 | 1.56 (1.16-2.12) | 0.004 | 1.42 (1.03-1.95) | 0.031 |
| Continuous sleep duration | 0.92 (0.88-0.95) | <0.001 | 0.91 (0.87-0.95) | <0.001 | 0.91 (0.87-0.95) | <0.001 | 0.92 (0.88-0.96) | <0.001 | 0.93 (0.89-0.97) | 0.001 |
ŌĆĀ Model 2 adjusted for age, sex, marital status, education, income, alcohol consumption frequency, smoking status, and BMI,
ŌĆĪ Model 3 adjusted for age, sex, marital status, education, income, alcohol consumption frequency, smoking status, BMI, shift work patterns, occupation, and employment status,
Table┬Ā4.
| Working hours (hours/week) |
Model 1* |
Model 2ŌĆĀ |
Model 3ŌĆĪ |
Model 4┬¦ |
Model 5Ūü |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Categorical working hours | ||||||||||
| ŌĆāŌēż40 | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] | |||||
| ŌĆā40.1 to 52 | 1.01 (0.87-1.17) | 0.888 | 1.02 (0.88-1.19) | 0.787 | 0.97 (0.83-1.13) | 0.674 | 0.95 (0.82-1.11) | 0.551 | 0.93 (0.8-1.09) | 0.402 |
| ŌĆā>52 | 1.47 (1.29-1.67) | <0.001 | 1.39 (1.22-1.58) | <0.001 | 1.34 (1.17-1.54) | <0.001 | 1.31 (1.14-1.50) | <0.001 | 1.30 (1.13-1.49) | <0.001 |
| Continuous working hours | 1.008 (1.005-1.011) | <0.001 | 1.008 (1.005-1.011) | <0.001 | 1.007 (1.004-1.010) | <0.001 | 1.006 (1.003-1.009) | <0.001 | 1.006 (1.003-1.009) | <0.001 |
ŌĆĀ Model 2 adjusted for age, sex, marital status, education, income, alcohol consumption frequency, smoking status, and BMI,
ŌĆĪ Model 3 adjusted for age, sex, marital status, education, income, alcohol consumption frequency, smoking status, BMI, shift work patterns, occupation, employment status,
REFERENCES