 |
 |
- Search
| Psychiatry Investig > Volume 19(10); 2022 > Article |
|
Abstract
Objective
Despite the well-documented relationship between emotion dysregulation and both post-traumatic stress disorder (PTSD) and alcohol use disorder symptoms, no studies investigated this issue in the context of the outbreak. Moreover, additional research investigating the role of mediators intervening in these pathways is required. Dissociation and emotional beliefs are two factors that may explain such relationships. However, a poor number of studies empirically tested their role.
Methods
A cross-sectional study on a sample of 719 community participants (32.5% males; Mage=34.36, standard deviation=14.38 years) was conducted. Participants fulfilled a battery of self-report questionnaires measuring levels of PTSD outbreak-related symptoms, alcohol use disorder, emotion dysregulation, emotional beliefs, and dissociation.
Results
Partial r-Pearson correlations showed that PTSD symptoms’ level was positively and significantly related to all variables investigated in the study whereas alcohol use disorder level was positively and significantly associated with emotion dysregulation and only some dimension of emotional beliefs and dissociation. Results drawn from a structural equation model highlight the mediating role of both emotional belief and dissociation in the relationship linking emotion dysregulation and alcohol use disorder whereas only dissociation, but not emotional beliefs, mediated the link between emotion dysregulation and PTSD symptoms.
In the 2019, population worldwide began to struggle from a new threat to physical health that is the outbreak of the coronavirus disease (COVID-19). In addition to the medical, economic, and social costs induced by the outbreak, experts from the field of mental health early stressed the potential wide range of psychological negative impacts caused by the set of events related to this situation [1-3]. Within the complexity and the heterogeneity of environmental changes that individuals experienced in response to the outbreak, some specific factors have been pointed out as potentially stressful and deleterious for the psychological functioning. For instance, “stayat-home” measures adopted by several countries have been likely to increase loneliness levels [4,5]. or exposure to family stressors [6] that are well-known risk factors for the onset and maintenance of mental disorders [7]. Also, fear for the COVID-19 [8], increase of grief rates [9], separation from significant others because of quarantine measures [10,11], loss of jobs [12], and uncertainty towards the future are only some of the potential stressful factors that may have negatively impacted mental health from the beginning of the outbreak.
Empirical research promptly investigated the nature of the psychological impacts related to the COVID-19 outbreak, stressing for instance the heightened onset of mood disorders or the reduction of psychological well-being [13,14]. Within the wide array of these psychological consequences, two specific psychological outcomes deserved the interest of researchers that are post-traumatic stress disorder (PTSD) and addictions.
Regarding PTSD, the identification of outbreak-related conditions as risk factors is not new. Studies documented elevated prevalence rates of PTSD among individuals having experienced quarantine, among “frontline workers” and among general population during the outbreak [15-17]. PTSD has been described as a condition characterized by the presence of some specific symptoms as such as vivid flashback, intrusive thoughts as well as emotional and somatic manifestations related to the traumatic events [18]. Despite the impact of the outbreak on the onset of PTSD symptoms has been quite well documented, less studies investigated the nature of the predictive psychological variables accounting for a higher propensity to develop this symptomatology. Anyway, the existing studies brought inspiring results evidencing that low income, education, pandemic related job loss [19,20], loneliness, COVID-19 worry, poor distress tolerance [21], media engagement [22], lack of social and organizational support, being female, having a lower age [23,24], economic stability and fear of contagion [20,25], and previous psychopathology [8,26] may play a role in the vulnerability to PTSD onset in the context of the outbreak.
Another central concern of the scientific and clinical communities regarding the impact of the COVID-19 outbreak on mental health is related to the field of addictions. For instance, substance use, nicotine consumption, and technological addictions have been investigated in individuals experiencing “stay-at-home” measures [27-31]. Some evidences report an increased selling of alcohol during the lockdown period, highlighting the potential increase in substance consumption as well as the worsening of pre-existing substance use disorder or even the risk of relapse of treatment seeking individuals [19,32-34]. Several theoretical, clinical, and empirical contributions pointed out the role of potential explaining variables of the proneness to suffer from problematic alcohol consumption as such as anxiety, depression and stress levels [35], gender [36,37], lower age, civil status, high income, fear of COVID-19, finance concerns [37], using social media as a source of information, experiencing child care challenges, and not being associated with a religious community [38].
As a whole, current literature provided convincing pieces of evidence documenting the impact of the COVID-19 on the propensity to experience both PTSD symptoms and alcohol use disorder. However, a still limited number of these studies investigated the role of psychological variables accounting for the interindividual differences in the vulnerability to experience these negative psychological consequences.
A potential explaining variable of both PTSD and alcohol use disorder is emotion dysregulation. Emotion dysregulation can be considered an umbrella construct that refers to the set of psychological processes and characteristics that describe a poor capacity to modulate the valence, duration, and intensity of own emotional states in order to behave successfully in coherence to own’s goals [39,40]. This construct is complex and multidimensional and is often considered as a transdiagnostic psychopathological factor [41,42]. The association between emotion dysregulation and both PTSD and addictions has been well established from a theoretical and empirical point of view [43-48]. Noteworthy, contributions published in the last decades stressed the importance to consider the way emotion dysregulation dimensions interact with contextual factors [49,50]. For instance, it has been argued that the adaptive versus maladaptive role of some emotion regulation strategies should be considered in light of the environmental demands [51,52]. Therefore, there is a need to investigate the role of emotion dysregulation in different contexts to extend the knowledge regarding the relationship between emotion dysregulation and psychopathology. Of note, few studies investigated the link between emotion dysregulation and both PTSD and alcohol use disorder in the context of the outbreak. Some authors found that heart rate reactivity to acute psychological stress predicts higher levels of PTSD symptoms during the COVID-19 pandemic [53] and others that emotion dysregulation predicted PTSD symptoms [8]. Also, among a sample of frontline healthcare workers, Zhou et al. [24] found that coping strategies mediated the relationship between perceived organizational support and PTSD symptoms. Regarding addictions, Cho et al. [54] observed that distress intolerance, anxiety sensitivity, and negative urgency predicted substance use among adolescents during the pandemic and that these pathways were mediated by the need to cope with outbreak related concerns.
Beyond the issues related to the topic of the COVID-19 outbreak, our knowledge regarding the mechanisms that may explain the association between emotion dysregulation and both PTSD and alcohol use disorder is far from being complete. For instance, the few studies that explored the topic of mediators linking emotion dysregulation to alcohol consumption highlight the role of metacognitions towards alcohol use [55], drinking motives [56,57], and depressive symptoms [58]. Other potential but currently overlooked variables accounting for the relationship between emotion dysregulation and both PTSD symptoms and alcohol use disorder are dissociation and emotion beliefs.
Dissociation refers to a set of distinct processes related to the disaggregation psychological functions deputed to the maintenance of the integrity of consciousness. The definition of dissociation and dissociative experiences is still a matter of debate and includes the question of its conceptualization as laying on a continuum ranging from normality to pathology [17]. The acceptation of the construct as a pathological process helped to recognize different dissociative experiences that characterize several mental disorders as such as borderline personality disorder, dissociative disorders, and PTSD [18]. The construct of dissociation refers to several features as such as altered experiences of consciousness called derealization and depersonalization (i.e., feeling to be outside of own body or feeling far away from the reality), amnesia (i.e., not remembering actions or events), and absorption (i.e., an intense experience of immersion in an activity together with a loss of psychological contact with the external world).
The explanations of why an individual may be more prone to dissociate compared to others include the role of emotional experiences [59]. Indeed, it has been argued that individuals dissociate more likely when they experience strong and negative emotional states [60]. From this perspective, it has been stated that a poor capacity to regulate own emotions may act as a predictor of the proneness to dissociate [61]. Importantly, dissociation is also thought to be strongly associated with PTSD [18]. Specifically, an individual experiencing high levels of fear, for instance when exposed to a traumatic event, may respond activating dissociative processes in order to transitory protect own psychological functioning. Therefore, a proneness to dissociate has been shown to act as a risk factor for the onset of PTSD [62]. High levels of dissociation have been showed to increase the risk for developing an addiction too [31]. Indeed, dissociation is likely to undermine self-regulation in consumption behavior, fostering the development of mechanisms accounting for addictions. As a whole, several preliminary evidences suggest that dissociation may be a central variable that mediates the relationships between emotion dysregulation and both PTSD and alcohol use disorder.
Another potential mediator of these relationships is metacognitions towards emotions. These correspond to the beliefs an individual has towards the utility and controllability of emotional states (either positive or negative). Past research demonstrated that emotion regulation self-efficacy is strongly related to emotion regulation capacities [63]. Therefore, believing that emotional states are not malleable and are out of control is likely to be associated with emotion dysregulation [64]. Similarly, negative beliefs towards emotions consisting in viewing emotional states as usefulness are likely to be associated with emotion dysregulation and especially with the lack of emotional awareness and emotional clarity. Despite the construct of emotional belief deserved a growing attention from researchers in the last decades, the opportunity to investigate the role of this topic has been only recently offered to the scientific community with the creation of the Emotional Belief Questionnaire (EBQ [65]). Therefore, direct empirical evidences regarding the link between this set of variables and some psychopathological conditions have been not extensively produced. However, a wide number of studies reported the relationship between the tendency to judge negatively own emotion states and PTSD or addictions [8,66]. Despite the current lack of evidence surrounding this issue, the gap regarding the exploration of the relationships between metacognitive beliefs and psychopathological outcomes (as such as PTSD and alcohol use disorder) and the potential mediating role of this variable in the pathways linking emotion dysregulation and psychopathological conditions is still to bridge.
As a whole, the existing literature suffers from several limitations. First, few studies investigated the relationship between emotion dysregulation and both PTSD and alcohol use disorder in the context of the outbreak. Then, the knowledge concerning the potential mediators accounting for these relationships is still limited. Specifically, dissociation and emotional beliefs are likely to explain these pathways, but few empirical evidences documented these topics. Therefore, a cross-sectional study on a sample of community participants was conducted to test the following hypotheses: H1. Emotion dysregulation will be associated with both PTSD and alcohol use disorder in the context of the COVID-19 outbreak. H2. Emotion dysregulation will be associated with both dissociation and emotional beliefs. H3. Dissociation and emotional beliefs will mediate the relationships between emotion dysregulation and both PTSD symptoms and alcohol use disorder.
In this study, a sample of 719 Italian adults has been recruited throughout a convenience sampling technique method (32.5% males; Mage=34.36, standard deviation [SD]=14.38 years). The only inclusion criteria were to being 18 years or older, to live in Italy and to have a sufficient understanding of the written Italian language. Specifically, an URL redirecting on a survey created on the EUsurvey platform was send to all potential participants. Starting the survey implied first to confirm being older than 18 years and read a cover letter illustrating the aims and the procedure of the study as well as information regarding anonymity and privacy. The main goal of the study, investigating the psychological impacts of the COVID-19 pandemic was illustrated in this cover letter. The email contact of the responsible for treatment data was also provided in order to allow the request of additional information regarding these issues. Finally, in case participants accepted to participate to the study, they were asked to fulfill an informed consent. Afterward, participants were asked to complete a battery of self-report questionnaires.
An initial questionnaire, created for the purposes of the study, collected demographic data as such as age and sex.
To measure emotion dysregulation levels, the Italian version of the Difficulties in Emotion Regulation Scale Short Form [39,67] was administrated. This questionnaire consists of 18 items asking the individual to answer on a 5-points Likert type scale (1=never; to 5=always) and provides a total score as well as a score for each subscales measuring distinct emotion dysregulation dimensions corresponding to 1) impulse-control difficulties, 2) difficulties pursuing goal-directed behavior when experiencing an negative emotions, 3) poor emotional awareness, 4) poor emotional clarity, 5) poor capacity to access to effective emotion-regulation strategies, 6) difficulty to accept in a nonjudgmental way own negative emotions. Overall, the instrument confirmed its good reliability as showed by the Cronbach’s values being 0.89 for the total score and higher than 0.74 for all subscales expect for the awareness subscale that obtained a reliability coefficient of 0.65.
Metacognitive beliefs regarding emotional responses were measured thanks to the administration of the EBQ [65]. This is a 16 items self-report questionnaire asking the participant to answer on a 7-points Likert type scale ranging from 1 (strongly disagree) to 7 (strongly agree). Different scoring methods have been provided by the authors that lead to the identification of specific subscales. For the purpose of this study, the subscales Positive Usefulness, Negative Usefulness (i.e., corresponding to beliefs regarding the lack of utility of positive and negative emotions respectively) and Controllability (i.e., beliefs about how emotions are uncontrollable) have been used. Preliminary analyses supported the good internal consistency of the EBQ subscales with Cronbach’s alpha resulting ≥0.81.
To measure dissociation levels, the Italian translation of the second version of the Dissociative Experiences Scale (DES [68,69]) has been administrated to all participants. This self-report questionnaire, consisting of 28 items with an answer response scale ranging from 0 (0% of the time) to 10 (100% of the time), evaluates the frequency by which the individual experience dissociative experiences in daily life. Because the factorial structures of the instrument are still a matter of debate [70], a conservative approach has been selected, using the original three factorial structure of the instrument. Therefore, three subscales have been used corresponding to three subtypes of dissociative experiences being depersonalization/derealization (DD, i.e., altered perceptions of the self or the surroundings), absorption (i.e., immersion in activities and unawareness of the external environment), and amnesia (i.e., not remembering past actions or events). Each subscale of the instrument showed, in this study, an excellent internal reliability with Cronbach’s alpha not being lower than 0.86.
Alcohol use disorder was measured with the Alcohol Use Disorders Identification Test (AUDIT [71]) that is a self-report questionnaire encompassing 10 items investigating the frequency of alcohol-related behaviors. The Cronbach alpha index obtained in this study (0.74) supported the good internal consistency of the instrument.
Finally, to measure the levels of PTSD symptoms, a modified version of the National Stressful Events Survey PTSD Short Scale [72] has been administered. This instrument asks the participant to answer to each of its 9 items on a 5-points Likert-type scale ranging from 0 (not at all) to 4 (extremely). In the version used in the study, we specified in the instruction that participant should have answered referring only to stressful events related to the COVID-19 outbreak. In this study, the instrument showed a good internal consistency with a Cronbach’s alpha index being 0.89.
The researcher procedure received the approval of the Ethical Committee of the University of Rome Sapienza Ethical Board (N° 808/2020) and were developed in compliance with the guidelines of the American Psychological Association for ethic in research. The study was conducted according to the ethical approval protocol and the 1975 Helsinki Declaration. Informed consent was signed by all the participant.
Analyses were performed by several steps. In a preliminary step, the internal consistencies of the measures used in the study have been verified calculating alpha Cronbach’s indexes. Afterward, using age and sex as covariates, the r-Pearson correlation matrix estimating the association between the main variables included in the study was calculated. These preliminary analyses were performed using the SPSS software v.23 for Windows (IBM Co., Armonk, NY, USA). The last step of the analytical plan was instead carried out using the lavaan package of the Rstudio software for Mac (R Foundation for Statistical Computing, Vienna, Austria). This consisted in the creation and the test of a structural equation model. Specifically, the model has been tested using the maximum likelihood estimation method and the goodness of fit was evaluated using several fit indexes namely the comparative fit index (CFI) and the root mean square error of approximation (RMSEA) [73,74]. Acceptable fit was considered when the indexes were equal or superior to 0.90 and inferior or equal to 0.08 for CFI and RMSEA respectively. In addition, in case of poor fit, modification indexes of the software were used in order to better specify the model adding the estimation of the correlation of some residuals [75,76].
Regarding the demographic characteristics of the sample, 98.3% of participants reported to be Italian and 24.2% stated to have at least one child. 17.4% of participants lived with the partner and/or with own child(ren) whereas most (47.4%) lived alone or with parents (13.1%). Fourteen participants were currently under quarantine measure while fulfilling the survey. Most participants lived in the Latium (56.9%), a central area of Italy and the others were quite well distributed across the Italian territory with a high percentage of participants also living in Lombardy (7.5%) the Italian area facing the highest rate of COVID-19 contaminations. Analyses of frequency were performed regarding potential traumatic variables related to the COVID-19 pandemic. In the total sample, four participants stated having been contaminated by the COVID-19 pandemic and one of them having been hospitalized. Also, 63 stated that they know at least one significant other (i.e., family member, friend or colleague) being contaminated by the COVID-19 and 25 participants reported having lost at least one significant other because of the COVID-19. Lastly, 58 participants stated that they changed or lost their job because of the COVID-19 pandemic. In addition, means and SDs of each variable involved in the study were calculated (see Table 1).
Computations of partial r-Pearson correlations matrix, controlling by age and sex, evidenced some statistically significant associations between the main variables investigated in the study. A full overview of results is available in Table 2. It was found that PTSD levels correlated positively and significantly with all other variables and that AUDIT total scores correlated positively and significantly with PTSD scores, emotion dysregulation levels, the uncontrollability, and positive usefulness subscales of the EBQ and the DD subscales of the DES-II. Also, the DERS-SF total score, the EBQ and DES-II subscales correlated significantly and positively with each other except for the Absorption subscale of the DES-II that was not correlated significantly with the EBQ subscales measuring usefulness beliefs towards positive and negative emotions.
The measurement model was drawn using items or subscales of each measure to create five latent variables (LVs). When instruments provided subscales, these were preferred to single items in order to avoid an overparameterization of the model. Specifically, the nine items of the National Stressful Events Survey PTSD Short Scale, the 10 items of the AUDIT, the six subscales of the DERS, the three subscales of the DES-II, and the three subscales of the EBQ were used as manifest variables to create the PTSD, alcohol use disorder, the emotion dysregulation, the dissociation and the emotion beliefs LVs, respectively.
Regarding the path model, this was created coherently with the hypotheses of the study. Specifically, emotion dysregulation was inserted as a predictor of all other LVs whereas dissociation and emotional beliefs were inserted as predictors of both PTSD and alcohol use disorder LVs. In addition, the indirect pathways leading emotion dysregulation to both PTSD and alcohol use disorder throughout the parallel mediating role of both emotional beliefs and dissociation levels were estimated. Finally, age and sex were inserted as covariates predicting the two outcomes (i.e., PTSD and alcohol use disorder).
The first test of the model obtained a good fit considering the RSMEA index (0.06; confidence interval [CI] 90%, 0.055 to 0.062). However, the CFI felt below the acceptable cut-off (0.88). Therefore, following the modification indexes, additional parameters were added to the model until a satisfactory fit was obtained according to both indexes. Four parameters, concerning the correlations between residuals of manifest variables converging on the same LVs, were added. The final model, fully displayed in Figure 1, showed a good fit with an RMSEA index being 0.05 (CI 90%, 0.050 to 0.057) and a CFI reaching 0.90. Regarding the measurement model, manifest variables significantly and positively loaded on the expected LVs. Results related to the path model evidenced that both emotional beliefs and dissociation were positively and significantly predicted by emotion dysregulation levels. Multiple regressions investigating the factors predicting PTSD levels identified emotion dysregulation, dissociation, and sex as positive and significant predictor whereas emotional beliefs and age did not explain an additional portion of observed variance. In addition, all variables, except emotion dysregulation, were showed to significantly predict alcohol use disorder levels either positively (dissociation, emotional beliefs) or negatively (age, sex). Regarding the indirect pathways, results indicated that dissociation significantly mediated the relationship between emotion dysregulation and PTSD levels (b=0.14, p<0.001) whereas emotional belief did not (b=0.01, p=0.651). Finally, data evidenced that the relationship between emotion dysregulation and alcohol use disorder was mediated by both dissociation (b=0.11, p=0.002) and emotional beliefs (b=0.05, p=0.036).
The aim of this study was to partially bridge several gaps of the current empirical literature. These were related to the lack of investigation of the relationship between emotion dysregulation and both PTSD and alcohol use disorder symptoms in the context of the outbreak as well as to the poor investigation of the potential mediating role of both dissociation and emotional beliefs in these pathways.
First, we found that emotion dysregulation was actually associated, also when controlling for age and sex, with both PTSD and alcohol use disorder symptoms during the outbreak. This is in line with previous literature advancing a theoretical and empirical link between these variables [43-48]. Therefore, in the context of the outbreak, the pattern of associations between these constructs did not appear to vary. Albeit this may apparently be considered a foregone conclusion, this is a relevant piece of research arguing for the stability of the maladaptive valence of the construct of emotion regulation across the context of the outbreak. This scientific effort was in line with most recent contributions that pointed out the need to examine the role of environmental changes on the adaptive versus maladaptive potential of some emotion regulation features [51]. Of note, the study did not measure the changes in the intensity of the relationship between emotion dysregulation and the two psychopathological outcomes. It may be speculated that the outbreak context may have potentiated this relationship in line with the idea that the maladaptive facet of emotion dysregulation is likely to act under stressful conditions. Future longitudinal studies would be able to disentangle this issue.
In addition, it has been found that higher levels of emotion dysregulation were associated with higher frequency of each type of dissociative experiences with the highest association being observed in relation to the derealization/depersonalization factor. This was in line with the hypotheses of the study. Indeed, it was expected that high levels of emotional dysregulation would have led to higher levels of dissociation because a poor capacity to regulate emotional states usually leads to high levels of emotional arousal that, in turn, is a well-known trigger for dissociative experiences. Moreover, the same pattern of association was found between PTSD levels and dissociation features. This is not surprising as dissociation has been described as a central aspect associated to this disorder [18]. Therefore, results of this study are in line with past literature. Regarding the associations between dissociation and alcohol use disorder symptoms, a more nuanced pattern of results emerged. Indeed, only the derealization and depersonalization components were found to be associated with alcohol use disorder during the outbreak. These results suggest the relevance to adopt a multidimensional perspective when approaching to the role of dissociation in psychopathology. In the case of alcohol use disorder, it may be speculated that alcohol may be used as a regulator of depersonalization and derealization states that are likely to induce anxious states in the individual. Moreover, experiencing this altered state of consciousness may undermine self-regulation capacities and specifically control over alcohol consumption. In line with this interpretation, several studies stressed the causal relationship of impulsivity on alcohol consumption [77]. Going beyond the bivariate associations between this set of variables, the mediational role of dissociation in the pathways linking emotion dysregulation to both PTSD and alcohol use disorder symptoms was tested successfully. These results mean that the role of emotion dysregulation is at least partially mediated by dissociative processes leading to psychopathological conditions. Regarding the nature of the emotional experiences involved in these pathways, even though we did not measure this aspect in our study, some interpretations can be formulated. Indeed, in the context of the outbreak, several authors observed that population experienced high levels of fear regarding the COVID-19 [8]. Of note, intense fear is thought to be the core emotion inducing dissociative experiences as well as the development of PTSD [54]. In addition, alcohol use is known to be often used to regulate anxious feelings. Therefore, it is plausible that the main emotional experience involved in the pathway linking emotional dysregulation to both alcohol use disorder and PTSD throughout dissociative processes referred to intense feelings of fear towards the COVID-19. From a clinical point of view, this underlines the utility to accurately assess and target dissociative processes in individuals with poor emotion regulation difficulties that suffer from PTSD and/or alcohol use disorder symptoms. This would allow, at least partially, the depotentiation of the deleterious impact of emotion dysregulation on these psychopathological outcomes.
The present study investigated a somewhat innovative topic that is emotional beliefs. The role of metacognitions towards the utility and the malleability of emotions (either positive or negative) has been theoretically stressed by several authors [64,78]. However, the investigation of this topic remained at the sidelines for several years partially because of the lack of a sound psychometric measures that operationalize the construct (since the creation of the EBQ). Explorative analyses evidenced that emotion dysregulation levels were positively and significantly associated with all the three components of emotional beliefs measured in this study, namely beliefs towards the usefulness and uncontrollability of positive and negative emotional states. This converges with data evidencing the relationship between poor emotion regulation performance and both poor emotion regulation self-efficacy and beliefs towards the non-malleability of emotional states [63]. In addition, results showed that PTSD symptoms were related to thoughts towards the uncontrollability of emotional states either positive or negative. This agrees with conclusions drawn from past studies that stressed the subjective nature of emotional arousal in individuals suffering from PTSD that reported their emotions to be overwhelming and uncontrollable [18]. Moreover, PTSD symptoms, in the present study, has been shown to be significantly associated with beliefs regarding the lack of utility of emotional states. Importantly, the proneness for emotional suppression of unpleasant internal states has been observed among individuals suffering from PTSD [79]. Also, a very recent study referred that a difficulty to accept positive emotion in a nonjudgmental way was a predictive factor of PTSD symptoms [80]. Therefore, the results of the present study may suggest that the relationship between this difficulty and PTSD symptoms may be at least partially linked to dysfunctional metacognitive beliefs towards the lack of utility of positive emotions. A slightly different pattern of association has been identified between emotional beliefs and alcohol use disorder. Indeed, only the uncontrollability of emotions and beliefs towards the lack of utility of positive emotions were associated with levels of alcohol use disorder. This converges towards the idea that individuals believing that emotions are static and not malleable may adopt strategies aimed to down-regulate disturbing internal states externally and passively as such as use of alcohol [64]. In addition, Weiss et al. [81] recently stressed the role of a difficulty to regulate positive emotional states in individuals prone to excessive drinking supporting the role of dysregulation of regulation of positive emotion as a central, but mainly overlooked, factor in addiction [82]. Finally, data evidenced that emotional beliefs mediate the pathways linking emotional dysregulation to alcohol use disorder but not the link between emotional dysregulation and PTSD symptoms. Regarding alcohol use disorder, this result suggests that intervention on individuals with high levels of emotional dysregulation and alcohol use disorder may benefit from a focus on emotional beliefs. In the context of the outbreak, individuals may have experienced high levels of loneliness due to interpersonal distancing and this may have led to negative emotions such as sadness and, potentially, depressive symptoms [4]. Negative metacognitive beliefs regarding low mood have been found to account for the maintenance of depression [83] so beliefs towards the impossibility to control sadness and the usefulness of positive emotions relieving from this may have acted as a risk factor for the use of alcohol as an automatic external regulator of negative internal states. This is especially important as dysfunctional metacognitive beliefs are likely to be targeted with effective and efficient treatment as such as psychoeducation or cognitive restructuring [32]. However, this may not be the case for the treatment of PTSD symptoms that may better benefit from a twice focus on both emotional dysregulation and emotional beliefs that appeared, in our study, to be two independent pathways increasing the proneness to experience PTSD symptoms. Indeed, our results may suggest that high levels of emotion dysregulation may lead to PTSD symptoms because of an actual difficulty to control a hyper emotional reactivity to triggers related to the traumatic events rather than to a low level of emotion regulation self-efficacy. Another explanation of this finding is that the mediating role of metacognitive beliefs in this pathway has been tested merging three dimensions of the construct that may be less pertinent to PTSD with respect to alcohol use disorder. For instance, whereas the role of dysregulation of positive emotions in addictions appears to be well established, its role in PTSD is still largely unexplored [84]. Therefore, merging dimensions related to both positive and negative emotions may have drowned the mediating role of metacognitive beliefs in the pathways linking emotion dysregulation to PTSD.
The conclusions drawn from the present study should be appreciated keeping in mind some key limitations. First, the design of research used is likely to limit the inferences that can be made towards the causal nature of the relationship observed. Therefore, an additional study may want to replicate the results obtained throughout the conduction of a longitudinal or experimental study. Also, participants were recruited among community and no clinical sample was included in the study. This may be especially problematic in light of the generalization of the conclusions to the clinical population. Again, a future study may want to replicate the study suing a sample of individuals suffering from PTSD and/or alcohol use disorder. Finally, the operationalization of the emotion dysregulation construct did not include the role of positive emotions. For instance, inspiring past studies used instrument as such as the Difficulties in Emotion Regulation Scale Positive or measuring the construct of Positive Urgency [85]. Considering the result documenting the link between emotional beliefs on positive emotions and both PTSD and alcohol use disorder, this topic would have deserved a greater attention during the study planification. Therefore, future studies may want to extend the knowledge regarding this issue using specific measures that operationalize the construct of dysregulation of positive emotions.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Damiano Rizzi receives a salary from association Soleterre Onlus. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Patrizia Velotti. Data curation: Sara Beomonte Zobel, Damiano Rizzi, Guyonne Rogier. Writing—original draft: Guyonne Rogier, Sara Beomonte Zobel, Writing—review & editing: all authors.
Funding Statement
This work was partially supported by the Soleterre Onlus [12.07.2019]. Partial financial support was received from Fondazione Soleterre Srl [Grant Number 588/19].
Figure 1.
Structural equation model testing the mediating role of emotional beliefs and dissociation in the relationships between emotion dysregulation and both PTSD symptoms and alcohol disorder. Dashed lines indicate non-significant paths; solid lines indicate significant paths at a 0.05 level; covariance alcohol disorder and PTSD=-0.002 (p=0.753). PTSD, post-traumatic stress disorder; DD, depersonalization/derealization.
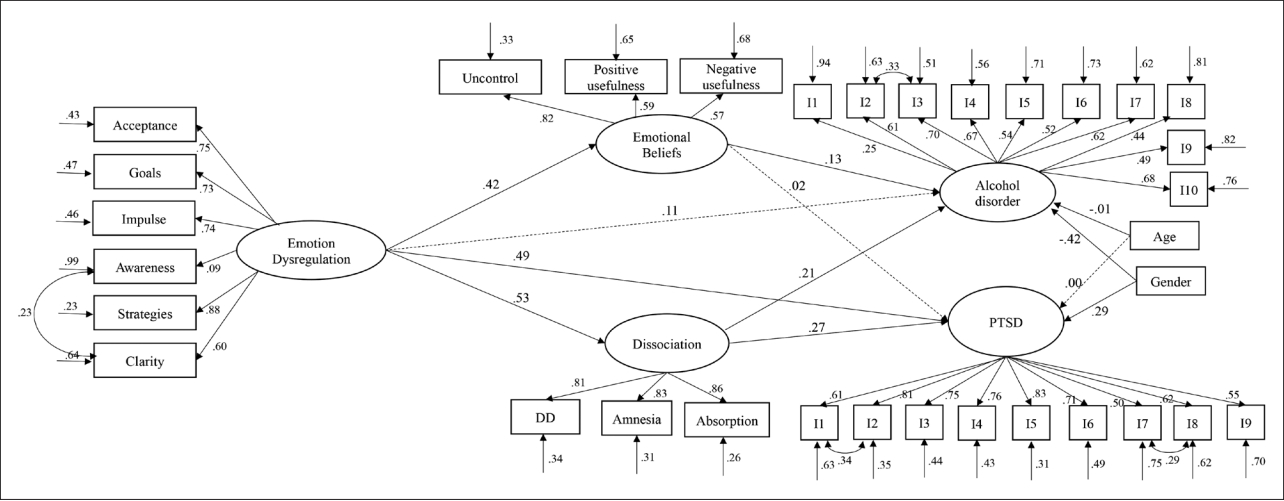
Table 1.
Ranges, means, and SDs of continuous variables involved in the study
Table 2.
Partial correlations, controlling for age and sex, between PTSD, alcohol disorder, emotion dysregulation, emotional beliefs, and dissociation
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
|---|---|---|---|---|---|---|---|---|
| 1. PTSD score | - | |||||||
| 2. AUDIT | 0.14** | - | ||||||
| 3. DERS-SF | 0.52** | 0.21** | - | |||||
| EBQ | 4. Uncontrollability | 0.26** | 0.13* | 0.36** | - | |||
| 5. Positive usefulness | 0.19** | 0.17** | 0.31** | 0.49** | - | |||
| 6. Negative usefulness | 0.18** | 0.06 | 0.24** | 0.50** | 0.34** | - | ||
| DES-II | 7. DD | 0.42** | 0.22** | 0.37** | 0.20** | 0.30** | 0.14** | - |
| 8. Amnesia | 0.26** | 0.07 | 0.19** | 0.19** | 0.20** | 0.15** | 0.39** | |
| 9. Absorption | 0.24** | 0.07 | 0.19** | 0.12* | 0.04 | 0.04 | 0.32** | |
REFERENCES
1. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - A systematic review and meta-analysis. Psychiatry Res 2020;291:113190



2. Sheraton M, Deo N, Dutt T, Surani S, Hall-Flavin D, Kashyap R. Psychological effects of the COVID 19 pandemic on healthcare workers globally: a systematic review. Psychiatry Res 2020;292:113360



3. Wang Y, Kala MP, Jafar TH. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: a systematic review and metaanalysis. PLoS One 2020;15:e0244630



4. Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry 2020;59:1218-1239.e3.



5. Sayin Kasar K, Karaman E. Life in lockdown: social isolation, loneliness and quality of life in the elderly during the COVID-19 pandemic: a scoping review. Geriatr Nurs 2021;42:1222-1229.



6. Pereda N, Díaz-Faes DA. Family violence against children in the wake of COVID-19 pandemic: a review of current perspectives and risk factors. Child Adolesc Psychiatry Ment Health 2020;14:40




7. Rodríguez-Fernández P, González-Santos J, Santamaría-Peláez M, Soto-Cámara R, Sánchez-González E, González-Bernal JJ. Psychological effects of home confinement and social distancing derived from COVID-19 in the general population—a systematic review. Int J Environ Res Public Health 2021;18:6528



8. Velotti P, Civilla C, Rogier G, Beomonte Zobel S. A fear of COVID-19 and PTSD symptoms in pathological personality: the mediating effect of dissociation and emotion dysregulation. Front Psychiatry 2021;12:590021



9. Stroebe M, Schut H. Bereavement in times of COVID-19: a review and theoretical framework. Omega (Westport) 2021;82:500-522.




10. Gracia DR, Rubetta ER. Literature review: quarantine and lockdown during covid19 outbreak impact on mental health problem. Jurnal Kesehatan Lingkungan 2020;12:29-37.


11. Velotti P, Rogier G, Beomonte Zobel S, Castellano R, Tambelli R. Loneliness, emotion dysregulation, and internalizing symptoms during coronavirus disease 2019: a structural equation modeling approach. Front Psychiatry 2021;11:581494



12. Mojtahedi D, Dagnall N, Denovan A, Clough P, Hull S, Canning D, et al. The relationship between mental toughness, job loss, and mental health issues during the COVID-19 pandemic. Front Psychiatry 2021;11:607246



13. Bareeqa SB, Ahmed SI, Samar SS, Yasin W, Zehra S, Monese GM, et al. Prevalence of depression, anxiety and stress in china during COVID-19 pandemic: a systematic review with meta-analysis. Int J Psychiatry Med 2021;56:210-227.



14. Mahmud S, Hossain S, Muyeed A, Islam MM, Mohsin M. The global prevalence of depression, anxiety, stress, and, insomnia and its changes among health professionals during COVID-19 pandemic: a rapid systematic review and meta-analysis. Heliyon 2021;7:e07393



15. Li Y, Scherer N, Felix L, Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: a systematic review and meta-analysis. PLoS One 2021;16:e0246454



16. Salehi M, Amanat M, Mohammadi M, Salmanian M, Rezaei N, Saghazadeh A, et al. The prevalence of post-traumatic stress disorder related symptoms in coronavirus outbreaks: a systematic-review and meta-analysis. J Affect Disord 2021;282:527-538.



17. Zhang L, Pan R, Cai Y, Pan J. The prevalence of post-traumatic stress disorder in the general population during the COVID-19 pandemic: a systematic review and single-arm meta-analysis. Psychiatry Investig 2021;18:426-433.




18. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed). Arlington: American Psychiatric Association; 2013.
19. Currie CL. Adult PTSD symptoms and substance use during Wave 1 of the COVID-19 pandemic. Addict Behav Rep 2021;13:100341



20. Di Crosta A, Palumbo R, Marchetti D, Ceccato I, La Malva P, Maiella R, et al. Individual differences, economic stability, and fear of contagion as risk factors for PTSD symptoms in the COVID-19 emergency. Front Psychol 2021;11:567367



21. Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res 2020;290:113172



22. Mukherjee M, Maity C. Influence of media engagement on the post traumatic stress disorder in context of the COVID-19 pandemic: an empirical reflection from India. J Hum Behav Soc Environ 2021;31:409-424.

23. Bonsaksen T, Heir T, Schou-Bredal I, Ekeberg Ø, Skogstad L, Grimholt TK. Post-traumatic stress disorder and associated factors during the early stage of the COVID-19 pandemic in Norway. Int J Environ Res Public Health 2020;17:9210



24. Zhou T, Guan R, Sun L. Perceived organizational support and PTSD symptoms of frontline healthcare workers in the outbreak of COVID-19 in Wuhan: the mediating effects of self-efficacy and coping strategies. Appl Psychol Health Well Being 2021;13:745-760.




25. Yin Q, Chen A, Song X, Deng G, Dong W. Risk perception and PTSD symptoms of medical staff combating against COVID-19: a PLS structural equation model. Front Psychiatry 2021;12:607612



26. Ravaldi C, Ricca V, Wilson A, Homer C, Vannacci A. Previous psychopathology predicted severe COVID-19 concern, anxiety, and PTSD symptoms in pregnant women during “lockdown” in Italy. Arch Womens Ment Health 2020;23:783-786.




27. Avena NM, Simkus J, Lewandowski A, Gold MS, Potenza MN. Substance use disorders and behavioral addictions during the COVID-19 pandemic and COVID-19-related restrictions. Front Psychiatry 2021;12:653674



28. Dumas TM, Ellis W, Litt DM. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health 2021;67:354-361.



29. Jager J, Keyes KM. Is substance use changing because of the COVID-19 pandemic? Conceptual and methodological considerations to delineating the impact of the COVID-19 pandemic on substance use and disorder. Addiction 2021;116:1301-1303.




30. Sun Y, Li Y, Bao Y, Meng S, Sun Y, Schumann G, et al. Brief report: increased addictive internet and substance use behavior during the COVID-19 pandemic in China. Am J Addict 2020;29:268-270.




31. Rogier G, Capone A, Velotti P. Emotion regulation strategies and dissociation in gambling disorder. Int Gambl Stud 2022;22:18-36.

32. Bakaloudi DR, Jeyakumar DT, Jayawardena R, Chourdakis M. The impact of COVID-19 lockdown on snacking habits, fast-food and alcohol consumption: a systematic review of the evidence. Clin Nutr 2022;Apr 16 [Epub]. Available at: https://doi.org/10.1016/j.clnu.2021.04.020.

33. DeJong CAJ, DeJong Verhagen JG, Pols R, Verbrugge CAG, Baldacchino A. Psychological impact of the acute COVID-19 period on patients with substance use disorders: we are all in this together. Basic Clin Neurosci 2020;11:207-216.


34. Xu S, Park M, Kang UG, Choi JS, Koo JW. Problematic use of alcohol and online gaming as coping strategies during the COVID-19 pandemic: a mini review. Front Psychiatry 2021;12:685964



35. DiClemente RJ, Capasso A, Ali SH, Jones AM, Foreman J, Tozan Y. Knowledge, beliefs, mental health, substance use, and behaviors related to the COVID-19 pandemic among US adults: a national online survey. J Public Health (Berl) 2022;30:2069-2079.




36. Ogueji IA, Agberotimi SF, Adesanya BJ, Gidado TN. Mental health and coping strategies during the COVID-19 pandemic: a qualitative study of unemployed and employed people in Nigeria. Anal Soc Issues Public Policy 2021;21:941-959.




37. Mougharbel F, Sampasa-Kanyinga H, Heidinger B, Corace K, Hamilton HA, Goldfield GS. Psychological and demographic determinants of substance use and mental health during the COVID-19 pandemic. Front Public Health 2021;9:680028



38. MacMillan T, Corrigan MJ, Coffey K, Tronnier CD, Wang D, Krase K. Exploring factors associated with alcohol and/or substance use during the COVID-19 pandemic. Int J Ment Health Addict 2022;20:1814-1823.



39. Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess 2004;26:41-54.


40. Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol 2003;85:348-362.


41. Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev 2010;30:217-237.


42. Garofalo C, Velotti P, Callea A, Popolo R, Salvatore G, Cavallo F, et al. Emotion dysregulation, impulsivity and personality disorder traits: a community sample study. Psychiatry Res 2018;266:186-192.


43. Espil FM, Viana AG, Dixon LJ. Post-traumatic stress disorder and depressive symptoms among inpatient adolescents: the underlying role of emotion regulation. Resid Treat Child Youth 2016;33:51-68.

44. Seligowski AV, Rogers AP, Orcutt HK. Relations among emotion regulation and DSM-5 symptom clusters of PTSD. Pers Individ Differ 2016;92:104-108.

45. Shepherd L, Wild J. Emotion regulation, physiological arousal and PTSD symptoms in trauma-exposed individuals. J Behav Ther Exp Psychiatry 2014;45:360-367.



46. Sheykhan R, Ghazanfari F, Jadidi F, Adineh M, Sadrmohamadi R. Attachment styles and cognitive emotion regulation strategies as predictor of post-traumatic stress disorder in veterans. J Mazandaran Univ Med Sci 2016;26:95-104.
47. Short NA, Boffa JW, Clancy K, Schmidt NB. Effects of emotion regulation strategy use in response to stressors on PTSD symptoms: an ecological momentary assessment study. J Affect Disord 2018;230:77-83.



48. Spies JP, Cwik JC, Willmund GD, Knaevelsrud C, Schumacher S, Niemeyer H, et al. Associations between difficulties in emotion regulation and post-traumatic stress disorder in deployed service members of the German Armed Forces. Front Psychiatry 2020;11:576553



49. Aldao A, Nolen-Hoeksema S. The influence of context on the implementation of adaptive emotion regulation strategies. Behav Res Ther 2012;50:493-501.


50. Tang Y, Huang Y. Contextual factors influence the selection of specific and broad types of emotion regulation strategies. Br J Soc Psychol 2019;58:1008-1033.



51. Bonanno GA, Papa A, Lalande K, Westphal M, Coifman K. The importance of being flexible: the ability to both enhance and suppress emotional expression predicts long-term adjustment. Psychol Sci 2004;15:482-487.



52. Rogier G, Garofalo C, Velotti P. Is emotional suppression always bad? A matter of flexibility and gender differences. Curr Psychol 2019;38:411-420.


53. Ginty AT, Young DA, Tyra AT, Hurley PE, Brindle RC, Williams SE. Heart rate reactivity to acute psychological stress predicts higher levels of posttraumatic stress disorder symptoms during the COVID-19 pandemic. Psychosom Med 2021;83:351-357.


54. Cho J, Bello MS, Christie NC, Monterosso JR, Leventhal AM. Adolescent emotional disorder symptoms and transdiagnostic vulnerabilities as predictors of young adult substance use during the COVID-19 pandemic: mediation by substance-related coping behaviors. Cogn Behav Ther 2021;50:276-294.



55. Dragan M. Difficulties in emotion regulation and problem drinking in young women: the mediating effect of metacognitions about alcohol use. Addict Behav 2015;48:30-35.


56. Aurora P, Klanecky AK. Drinking motives mediate emotion regulation difficulties and problem drinking in college students. Am J Drug Alcohol Abuse 2016;42:341-350.


57. Buckner JD, Lewis EM, Abarno CN, Morris PE, Glover NI, Zvolensky MJ. Difficulties with emotion regulation and drinking during the COVID-19 pandemic among undergraduates: the serial mediation of COVID-related distress and drinking to cope with the pandemic. Cogn Behav Ther 2021;50:261-275.


58. Holzhauer CG, Gamble SA. Depressive symptoms mediate the relationship between changes in emotion regulation during treatment and abstinence among women with alcohol use disorders. Psychol Addict Behav 2017;31:284-294.



60. Van der Hart O, Rydberg JA. Vehement emotions and trauma-generated dissociation: a Janetian perspective on integrative failure. J Trauma Dissociation 2019;3:191-201.

61. Zavattini GC, Garofalo C, Velotti P, Tommasi M, Romanelli R, Santo HE, et al. Dissociative experiences and psychopathology among inmates in Italian and Portuguese prisons. Int J Offender Ther Comp Criminol 2017;61:975-992.



62. Breh DC, Seidler GH. Is peritraumatic dissociation a risk factor for PTSD? J Trauma Dissociation 2007;8:53-69.

63. Tamir M, Bigman YE, Rhodes E, Salerno J, Schreier J. An expectancyvalue model of emotion regulation: implications for motivation, emotional experience, and decision making. Emotion 2015;15:90-103.


64. Ford BQ, Gross JJ. Why beliefs about emotion matter: an emotion-regulation perspective. Curr Dir Psychol Sci 2019;28:74-81.


65. Becerra R, Preece DA, Gross JJ. Assessing beliefs about emotions: development and validation of the emotion beliefs questionnaire. PLoS One 2020;15:e0231395



66. Powers A, Cross D, Fani N, Bradley B. PTSD, emotion dysregulation, and dissociative symptoms in a highly traumatized sample. J Psychiatr Res 2015;61:174-179.



67. Giromini L, Velotti P, de Campora G, Bonalume L, Cesare Zavattini G. Cultural adaptation of the difficulties in emotion regulation scale: reliability and validity of an Italian version. J Clin Psychol 2012;68:989-1007.


68. Carlson EB, Putnam FW. An update on the dissociative experiences scale. Dissociation: Progress in the Dissociative Disorders 1993;6:16-27.
69. Schimmenti A. Dissociative experiences and dissociative minds: exploring a nomological network of dissociative functioning. J Trauma Dissociation 2016;17:338-361.


70. Saggino A, Molinengo G, Rogier G, Garofalo C, Loera B, Tommasi M, et al. Improving the psychometric properties of the dissociative experiences scale (DES-II): a Rasch validation study. BMC Psychiatry 2020;20:8




71. Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption--II. Addiction 1993;88:791-804.


72. LeBeau R, Mischel E, Resnick H, Kilpatrick D, Friedman M, Craske M. Dimensional assessment of posttraumatic stress disorder in DSM-5. Psychiatry Res 2014;218:143-147.


73. Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociol Methods Res 1992;21:230-258.


74. Kline RB. Promise and pitfalls of structural equation modeling in gifted research. In: Thompson B, Subotnik RF, editor. Methodologies for conducting research on giftedness. Washington, DC: American Psychological Association, 2010, p. 147-169.
75. Saris WE, Satorra A, Van der Veld WM. Testing structural equation models or detection of misspecifications? Struct Equ Model 2009;16:561-582.

76. Coskunpinar A, Dir AL, Cyders MA. Multidimensionality in impulsivity and alcohol use: a meta-analysis using the UPPS model of impulsivity. Alcohol Clin Exp Res 2013;37:1441-1450.



77. Moore SA. The cognitive consequences of emotional suppression in PTSD [dissertation] Seattle, University of Washington. 2008.
78. Rogier G, Beomonte Zobel S, Morganti W, Ponzoni S, Velotti P. Metacognition in gambling disorder: a systematic review and meta-analysis. Addict Behav 2021;112:106600


79. Weiss NH, Nelson RJ, Contractor AA, Sullivan TP. Emotion dysregulation and posttraumatic stress disorder: a test of the incremental role of difficulties regulating positive emotions. Anxiety Stress Coping 2019;32:443-456.



80. Weiss NH, Forkus SR, Contractor AA, Schick MR. Difficulties regulating positive emotions and alcohol and drug misuse: a path analysis. Addict Behav 2018;84:45-52.



81. Weiss NH, Gratz KL, Lavender JM. Factor structure and initial validation of a multidimensional measure of difficulties in the regulation of positive emotions: the DERS-positive. Behav Modif 2015;39:431-453.




82. Velotti P, Rogier G. An exploratory study of the role played by hedonic dysregulation in gambling disorder. Int Gambl Stud 2021;21:1-16.

83. Cano-López JB, García-Sancho E, Fernández-Castilla B, Salguero JM. Empirical evidence of the metacognitive model of rumination and depression in clinical and nonclinical samples: a systematic review and meta-analysis. Cogn Ther Res 2022;46:367-392.


84. Gruber J. The Oxford handbook of positive emotion and psychopathology. New York: Oxford University Press; 2019.







