Mental Health Problems During COVID-19 and Attitudes Toward Digital Therapeutics
Article information
Abstract
Objective
We aimed to elucidate public mental health problems and associated factors during the coronavirus disease-2019 (COVID-19). Furthermore, we evaluated people’s attitudes toward digital therapeutics during the pandemic.
Methods
Data was collected online from participants, aged between 20–50 without any history of mental illness, from June 1st to June 30th 2021. The survey consisted of questions regarding demographics, changes during pandemic and attitude towards digital therapeutics, and mental health measures.
Results
Among the total of 445 participants, 49.2% reported significant level of stress and 13.5% and 7.0% met the screening criteria for major depressive disorder and generalized anxiety disorder, respectively. Significant predictive factors for mental health problems were-younger age group, female sex, currently being treated for medical or surgical disease, change in the amount of time spent on mobile device or computer after pandemic, change in household income, and change in work environment due to pandemic. Furthermore, 35.1% of participants, considered psychiatric consultation, at least slightly, but were hesitant to receive it due to the fear of contacting COVID-19 at the clinics. Instead, 54.4% of them preferred using digital therapeutics as an alternative to visiting offline clinics.
Conclusion
We demonstrated that COVID-19 increased mental health problems along with access problems and identified their predictive factors. Digital therapeutics emerged as a viable solution to mental health problems and it was well-received by those in need of psychiatric consultation. Therefore, development and implementation of digital therapeutics should be considered to improve the mental health of people.
INTRODUCTION
The coronavirus disease-2019 (COVID-19) disease began to spread globally from December 2019, and the World Health Organization declared it as a worldwide public health emergency. In South Korea, since the first diagnosis of it on 20th January 2020, a sum of 132,818 people have been diagnosed with COVID-19 by 18 May 2021 [1]. While the majority of countries have shown decreasing number of COVID-19 cases from early 2021 to June 2021, confirmed cases started to increase again due to the delta variant of the virus by June [2]. In June 2021, strict social distancing measures were applied in South Korea: private gatherings of five or more people were prohibited and restaurants and cafés had to close at 10PM [3].
The COVID-19 pandemic triggered fear and anxiety among people, while preventive social measures led to social isolation, along with financial difficulties, which increased people’s perceived level of stress [4-8]. Researchers and mental health professionals became increasingly concerned about the pandemic’s impact on mental health [9-11]. Indeed, many research have demonstrated evidence for increase in mental health problems associated with COVID-19. In a recent meta-analysis, on the prevalence of mental health problems associated with the COVID-19 pandemic worldwide, involving 221,970 participants, evidenced pooled prevalence of depression, anxiety, distress, and insomnia to be 31.4%, 31.9%, 41.1%, and 37.9%, respectively [12]. Previous studies have identified candidate risk factors for increased mental health problems during the pandemic. Among Chinese individuals, the following two factors-time spent focusing on the COVID-19 and age less than 35 years-were associated with increased risk for Generalized Anxiety Disorder (GAD) [13]. In Canadian and American people, factors such as female sex, younger age (below 35), and past mental health treatment were demonstrated to be significant predictors of mental health problems [14].
Having experienced the peak of the COVID-19 pandemic, some people choose to avoid crowds or places with a possibility of meeting other patients, such as hospitals [15]. Indeed, studies on medical service behaviors have shown that number of emergency and non-emergency visits to hospitals have decreased worldwide [15-17]. Patients’ avoidance of face-to-face clinic visits has led healthcare providers’ search for digital solutions for health problems [18]. Digital therapeutics is a software-driven evidence-based intervention that is designed to prevent, manage, or treat a particular disorder [19]. Digital therapeutics has been developed in multiple clinical areas such as diabetes [20,21], cardiovascular diseases [18], neurological disorders [22], or mental illnesses [23,24]. As digital therapeutics does not require hospital visit or face-to-face interaction, it is well-suited to fill the access gap in healthcare during or after the pandemic [18].
In this study, we intended to find the predictors of mental health problems following the COVID-19 outbreak and evaluate public’s attitudes toward digital healthcare. Unlike most of the previous studies, our study only included participants without previous history of being treated or diagnosed for mental illness. Results from logistic regression studies that include participants with previous history of mental illness can reflect predictive factors for the mental illness [25], regardless of whether it appeared during or before the pandemic. Therefore, we focused on incident cases of mental illness and on finding predictive factors for mental health problems that appeared during the pandemic. In addition, our study focused on people aged between 20–50 years, who were the most active participants in economic and social activities. Furthermore, we studied public’s attitudes toward digital therapeutics as a solution for increased need of diagnosis and treatment of mental health problems during the pandemic.
METHODS
Participants
We collected the study data by sending out online survey to volunteer participants recruited on social media websites from June 1st to June 30th, 2021. Informed consent was obtained from all participants before the survey was sent to the participants. Data were collected anonymously using Google Sheets. Eligibility criteria required participants to be aged between 20 to 50 years and without any history of being diagnosed or treated for mental illness. Completed questionnaires were obtained from 508 participants. Twenty-nine participants were excluded for having previous history of being treated or having psychiatric disorders and 32 were excluded for not meeting the age range of 20 to 50. Total of 445 participants met our criteria. This study was approved by the Institutional Review Board of National Health Insurance Service Ilsan Hospital (NHIMC 2021-03-022).
Survey content and outcome measures
We developed our survey for this project and provided that to the participants as an online link that could be accessed both via computer or mobile phone. The survey was designed to gather information regarding the COVID-19 pandemic experience and psychiatric symptoms during the pandemic, and possible predictive factors for such psychiatric symptoms in participants without previous history of mental illness. For this purpose, we asked participants to answer questions regarding the demographics, COVID-19 related experiences, and self-reported questionnaire regarding psychiatric symptoms. Participants were initially asked for their history of being diagnosed or treated for psychiatric disorder for screening purpose. They provided us with demographic information, including age, gender, geographic location, marital status, education, and occupation. They also answered questions regarding their COVID-19 pandemic experience, such as admission to hospital, self-quarantine, or active surveillance, and the change in their occupation status, work environment, household income, daily hours spent self-isolating, frequency of leaving home other than for work and school, stress level due to social distancing, hopefulness for the pandemic to end, and time spent online before and after the COVID-19 pandemic. We also assessed their need for psychiatric consultation and attitudes toward using digital therapeutics.
Instruments used to evaluate participants’ psychiatric symptoms were the GAD-7 [26], Patient Health Questionnaire-9 (PHQ-9) [27], and Perceived Stress Scale-10 (PSS-10) [28]. In addition, Pittsburgh Sleep Quality Index (PSQI) and Rosenberg’s Selfesteem Scale (RSES) [29,30] were used to assess quality of sleep and subjective self-esteem in participants, respectively. GAD-7 is a screening scale for GAD, which measures anxiety symptoms in the past two weeks [26]. This scale contains seven items, each of which is rated from 0 to 3, with a total score ranging up to 21. In our study, GAD-7 score ≥10 was used to indicate significant anxiety symptoms [26]. PHQ-9 is a brief screening scale for depression and assesses depressive symptoms in the past two weeks. This scale contains nine items, each of which is scored from 0 to 3. Total score ranges from 0 to 27, with higher scores indicating more severe symptoms. In this study, PHQ-9 score ≥10 was used to indicate significant depressive symptoms [27]. PSS-10 is a screening scale to evaluate an individual’s feeling of uncontrollable stress. The scale contains 10 items, each rated from 1 to 5. Higher score indicates higher level of stress. In our study, PSS-10 score ≥14 was used to indicate significant level of stress [31]. PSQI is a self-rating questionnaire that evaluates sleep quality and disturbances during the past month. The index is comprised of 19 items with an overall score from 0 to 21. Participants who scored more than 5 were considered poor sleepers [32]. The index also includes seven other components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction [32]. RSES is a self-reported questionnaire that consists of a 10-item survey that measures global self-worth. Items are scored using a 4-point Likert scale with responses from ‘strongly agree’ to ‘strongly disagree.’ Scores below 15 suggest low self-esteem [29,33].
Statistical analyses
We used SPSS version 26.0 (IBM Corp., Armonk, NY, USA) statistical package for statistical analyses. Logistic regression was performed to determine factors for mental health disorders. We selected sociodemographic variables that appeared to be related to mental health problems during the pandemic: age, female sex, residing in a capital region, currently being treated for medical or surgical disease, average daily hours spent self-isolating. As excessive use of mobile device or computer has been shown to negatively affect mental and physical health [34], therefore, we selected change in the amount of time spent on mobile device or computer after COVID-19. Since previous studies demonstrated financial distress was associated with mental health problems, we selected change in the household income and change in the work environment due to COVID-19 as factors that might attribute to having mental health problems.
RESULTS
Sample demographics
A total of 445 participants were included for analysis (Table 1). Participants were categorized into age groups of 20–29 (50.3%), 30–39 (36.2%), 40–50 (13.5%). Their residence were categorized into two types: capital region and non-capital region. Capital region included Seoul, Gyeonggi, Incheon province, and non-capital region included all other areas in Korea. There were 311 participants (69.9%) from the capital region, and 134 (30.1%) from non-capital region in Korea; 306 (68.8%) were single, 132 (29.7%) were married, 4 (0.9%) were divorced, and 2 (0.4%) maintained domestic partnership. There was one participant who completed middle school or less, 33 (7.4%) completed high school or less, 19 (4.3%) graduated community college, 321 (72.1%) graduated university, and 70 (15.7%) completed graduate school (Table 1).
Impact of COVID-19 on daily life
As shown in Figure 1, at the time of the survey, 55 (12.4%) participants experienced self-quarantine while being asymptomatic, 8 (1.8%) went through self-quarantine due to COVID-19 symptoms (Figure 1A), and 2 (0.4%) had been admitted to hospitals due to the COVID-19 infection; 339 (76.2%) participants left home for other than work and school 0–2 days a week (Figure 1B), 67 (15.2%) left home 3–4 days a week, and 39 (8.8%) left home 5–7 days a week; 95 (21.9%) participants reported changes in their occupation due to COVID-19 (Figure 1C), 46 (10.3%) reported decreased number of days or hours of working (Figure 1D), 63 (14.2%) started working from home partially, while 41 (9.2%) reported working from home full time and 12 (2.7%) reported being on paid leave; 142 (31.9%) reported decrease in the household income post-COVID-19 (Figure 1E), 91 (20.4%) reported that they were not hopeful at all that the pandemic will end, while 18 (4.0%) reported they were extremely hopeful that it will end (Figure 1F). Regarding stress level due to social distancing, 9 (2.0%) reported extreme stress, 97 (21.8%) reported severe level of stress, 162 (36.4%) reported moderate level of stress, 119 (26.7%) reported mild level of stress while only 55 (12.4%) reported having no stress due to social distancing (Figure 1G). Meanwhile, the average amount of time spent online increased from 5.18 hours a day pre-COVID-19 to 7.65 hours post-COVID-19 (Figure 1H).
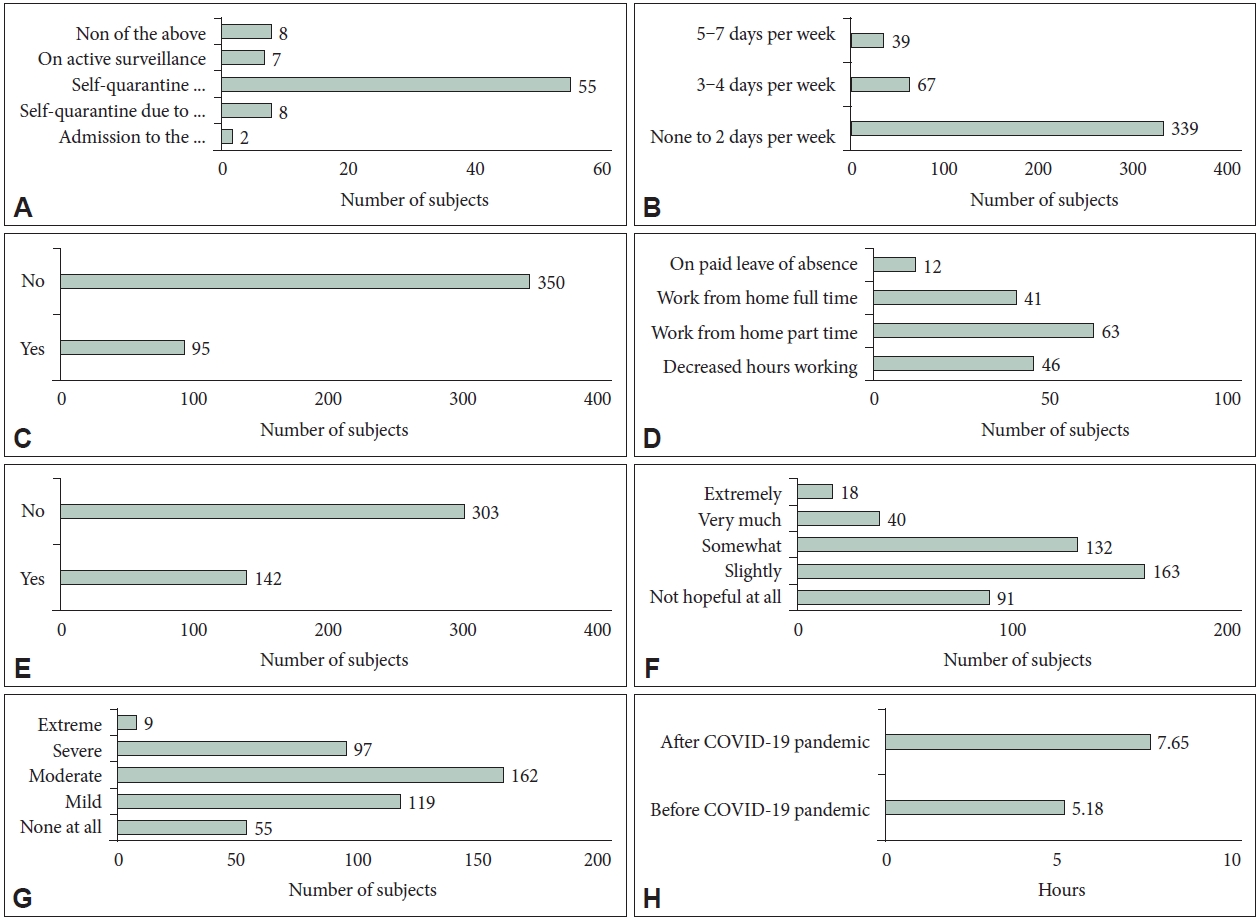
Impact of the COVID-19 pandemic in daily life. A: COVID-19 related experience. B: Frequency of leaving home other than work and school (per week). C: Change in the occupation due to COVID-19. D: Change in the work environment due to COVID-19. E: Decrease in household income due to COVID-19. F: How hopeful do you feel that the pandemic will end? G: Stress level due to social distancing. H: Time spent online. COVID-19, coronavirus disease-2019.
Public mental health during COVID-19
Mean symptom severity score for depression in PHQ-9 was 4.57, which was in the higher end of normal range for depressive symptoms (Table 1) [27]. Among the participants, 125 (28.1%) had mild depressive symptoms (PHQ-9: 5–9), 35 (7.9%) had moderate depressive symptoms (PHQ-9: 10-14), 14 (3.1%) had moderately severe depressive symptoms (PHQ-9: 15–19), and 6 (1.3%) had severe depressive symptoms (PHQ-9: 20–27) (Figure 2A). Mean symptom severity score for anxiety in GAD-7 was 2.88, which was also in the higher normal range (Table 1) [26]. Among the participants, 80 (18.0%) had mild anxiety symptoms (GAD-7: 5–9), 22 (4.9%) had moderate anxiety symptoms (GAD-7: 10–14), and 6 (1.3%) had severe anxiety symptoms (GAD-7: 15–21) (Figure 2B). Regarding GAD, 7.0% met the screening criteria [26], while 13.5% met the criteria for major depressive disorder (Table 1) [27]. Moreover, 70.3% of the participants had poor sleep quality measured by a total PSQI score over 5 [32]. About half of the participants (49.2%) reported significant level of stress with PSS-10 score over 14 [35], 6 (1.3%) had high stress level (PSS-10: 27–40), 201 (45.2%) had moderate stress level (PSS-10:14–26), and 215 (48.3%) had low stress level (PSS-10: 0–13) (Figure 2C).
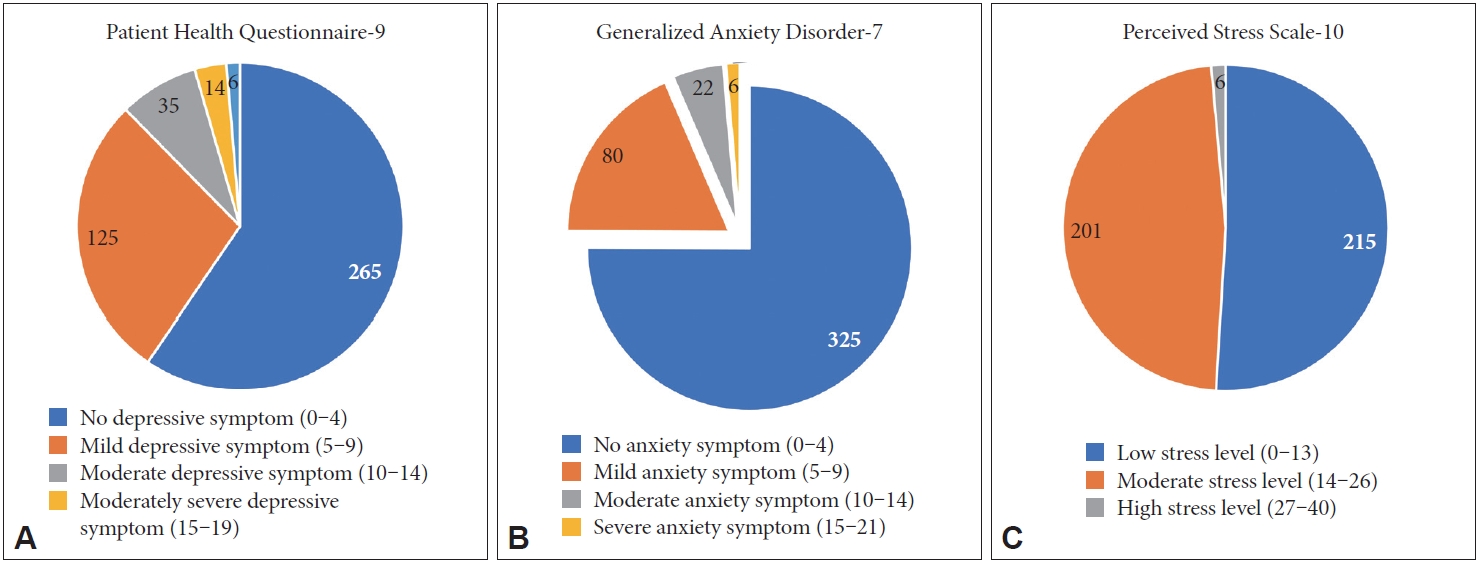
Severity of the current level of psychiatric symptoms of participants in the survey during COVID-19: depression (Patient Health Questionnaire-9) (A), anxiety (Generalized Anxiety Disorder-7) (B), and stress (Perceived Stress Scale-10) (C).
We evaluated predictors of significant level of major depressive disorder, GAD, stress or insomnia using logistic regression models (Table 2). Participants aged 20–29 years had odds ratios for major depressive disorder and GAD of 3.05 and 6.11, respectively. Female participants had odds ratios of 2.61, 3.12, and 2.18 for major depressive disorder, GAD, and higher perceived stress, respectively. Those who were currently being treated for medical or surgical disease had odds ratios of 2.32 and 4.22 for major depressive disorder and GAD, respectively. Change in the amount of time spent on mobile device or computer after COVID-19 pandemic was found to be a significant predictive factor for major depressive disorder and insomnia with odds ratios of 1.14 and 1.13, respectively. Decrease in household income due to COVID-19 had odds ratio for major depressive disorder of 2.18. Being on paid leave had an odds ratio of 5.24 for major depressive disorder.
Fifty-nine (13.3%) participants mentioned they considered receiving psychiatric consultation after the COVID-19 pandemic (Figure 3A). When participants were asked if they considered receiving psychiatric consultation after COVID-19 pandemic but hesitated due to the risk of contacting COVID-19 while visiting clinics, 13 (2.9%) replied very much, 30 (6.7%) replied somewhat, and 89 (20.0%) replied slightly, and 289 (64.9%) mentioned not at all (Figure 3B). For psychiatric diagnosis, 130 (29.2%) participants were willing to use remote treatment, 149 (33.5%) were willing to use self-diagnostic application or online program, while only 96 (21.6%) were willing to see a psychiatrist for psychiatric diagnosis (Figure 3C). For psychiatric treatment, only 93 (20.9%) were willing to visit a clinic to see a psychiatrist, while 151 (33.9%) preferred materials provided online and 127 (28.5%) preferred remote medical treatment (Figure 3D). Participants favored using digital therapeutics or self-diagnostic application, with 296 (66.5%) replying that they would be willing to use them once they were available (Figure 3E) and 242 (54.4%) mentioning that they would even prefer it to visiting offline clinics for diagnosis and treatment (Figure 3F).
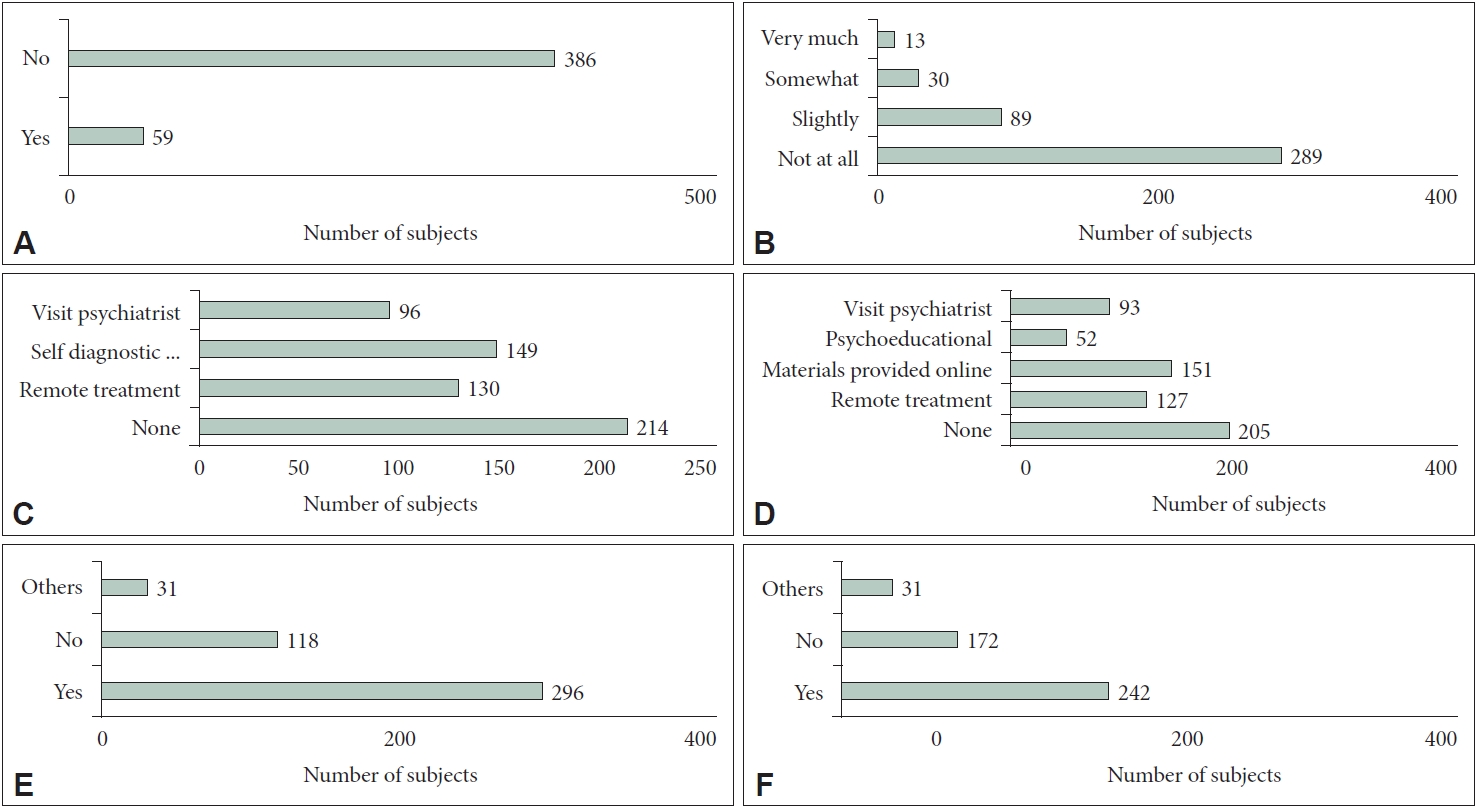
Attitude towards mental health services and digital therapeutics during the COVID-19 pandemic. A: Have you considered receiving psychiatric consultation after COVID-19 pandemic? B: Have you considered receiving psychiatric consultation after COVID-19 pandemic, but hesitated due to the risk of contacting COVID-19 while visiting hospital? C: Types of service you are willing to use for psychiatric diagnosis. D: Types of services you are willing to use for psychiatric treatment. E: Are you willing to use self-diagnostic application or digital therapeutics? F: If digital therapeutics allows self-diagnosis and treatment, would you prefer it to visiting offline clinic? COVID-19, coronavirus disease-2019.
DISCUSSION
In our study, 7.0% of the participants met the screening criteria of GAD with GAD-7 score above 10. Compared to the usual lifetime prevalence of GAD of 2.4% reported in the Korean national survey [36], prevalence was higher in our study. This was in line with high prevalence of GAD in the Chinese population from 19.6% [37] to 35.1% [13] and 30.7% in the US and Canadian population [14]. In our study 13.5% of participants met the screening criteria for major depressive disorder, with a PHQ-9 score of 10 or higher, which was higher than 6.1% [38] to 6.7% [39] reported in previous studies on Korean population. This was also in line with the reported range of 9.8% [37] to 48.3% [40] in China during the outbreak of COVID-19. As our study only included participants who did not have a history of being treated or diagnosed for mental illness, our result might reflect the increase in psychiatric symptoms such as depression and anxiety post-pandemic.
In this study, with logistic regression, we explored the relationship between different factors and mental health during the COVID-19 outbreak. For GAD, the following factors - female sex, younger age (20–29 years), currently being treated for medical or surgical disease - were demonstrated to be significantly predictive. For major depressive disorder, factors such as younger age (20–29), female sex, currently being treated for medical or surgical disease, change in the amount of time spent on mobile device or computer after the COVID-19 pandemic, change in the household income due to COVID-19, change in the work environment due to COVID-19 (being on paid leave) - appeared as predictive factors. For significant level of stress, female sex was shown as a predictive factor.
In our study, female sex was demonstrated as a predictive factor across different mental health problems. Female participants were 2.61, 3.12, and 2.61 times more likely to have major depressive disorder, GAD, and significant perceived stress, respectively. This is in line with previous studies of mental health problems in the pandemic, which showed female sex as a risk factor [14,41-43]. As women are known to use “emotional support” as a coping strategy more frequently than men [44], it is possible that social distancing measures implemented during the pandemic had a higher impact on women, interfering with the coping strategy. Other possible reasons could be related to working while taking care of children spending longer time at home due to social distancing measures [45]. While this result could suggest that women were more vulnerable to mental health problems during the pandemic, it might also reflect the epidemiological difference in depression and anxiety between men and women. In fact, it is known that prevalence of anxiety and depressive disorders were higher for women even before the pandemic [46].
Younger age (20–29) was shown as a predictor of GAD and major depressive disorder. Participants from age 20 to 29 were 3.05 and 6.11 times more likely to have major depressive disorder and GAD, respectively. This finding is in line with previous findings [47]. As older people, through experience, gain resilience and learn how to manage emotions, it is understandable that younger age will be a predictive factor for depression [48]. Previous studies reported that this vulnerability may, in part, be mediated by increase in the use of video-chatting, gaming and dating apps [14]. This trend was also shown in our sample, in which younger adults from age 20 to 29 reported increase of 3.04 hours per day on average time spent using cell phone or computer after the pandemic, which was higher than 2.05 hours and 1.47 hours reported by age groups 30–39 and 40–50, respectively. Previous studies also suggested that younger adults were more likely to engage in maladaptive behaviors in response to confinement and might show over-eating or increase in substance use [49].
Currently being treated for medical or surgical diseases has been shown to be a predictive factor for GAD and major depressive disorder. This is in line with previous studies that has demonstrated increased risk of mental health problems in patients with pre-existing conditions [50], and those with chronic diseases, such as autoimmune disease [51,52], chronic kidney disease [53], or cystic fibrosis [54]. This is especially worrying as patients with pre-existing medical condition have been reported to cancel medical appointments which led to delayed care [55]. Delayed care along with added mental health problems may lead to worst-case clinical outcomes [55].
Change in the amount of time spent on mobile device or computer after the COVID-19 pandemic has been shown to be a predictive factor for major depressive disorder and insomnia. For every increased hour of mobile phone usage after the COVID-19 pandemic, participants were 1.14 times more likely to have major depressive disorder. Lockdown due to COVID-19 has inevitably decreased the amount of time spent physically with loved ones while it increased the amount of time spent online [56]. Our result was in line with previous studies that reported increased time spent online was associated with depression, anxiety, and insomnia [57-59].
Furthermore, change in the household income has also been shown as a predictive factor for major depressive disorder. In our study, 31.9% reported change of income due to COVID-19, and they were 2.18 times more likely to have major depressive disorder. Previous studies demonstrated that financial distress might lead to mental health problems [60-62].
In this context, it is important to note that while 13.3% of the participants considered psychiatric consultation after the COVID-19 outbreak, 35.1% responded that they considered receiving psychiatric consultation but hesitated due to the fear of contacting COVID-19 while visiting the clinics. This problem of access is concerning as the pandemic, which has caused mental health problems, is also acting as a barrier to access proper psychiatric care to those who are most vulnerable.
Digital therapeutics has been gaining attention in the field of psychiatry, and has begun to be applied in clinical settings for attention-deficit/hyperactivity disorder, insomnia, and substance addiction [63]. As digital therapeutics do not require face-to-face interaction or frequent visit to the clinic, it may be an effective tool to help patients who are hesitant to visit the clinic during the pandemic. Increased need for psychiatric care, coupled with even higher barrier to access to the psychiatric clinic has led to a surge in demand for digital therapeutics as a more favorable option for receiving psychiatric care, with 54.4% of the participants in our study responding that they would prefer using psychiatric digital therapeutics than visiting an offline psychiatric clinic.
There are several potential limitations to our study. We collected the data through online survey. Using an online modality has a risk of selection bias. Furthermore, we used self-reported questionnaires to assess psychiatric symptoms without clinical diagnosis, which might lead to response bias. High number of variables, compared to a relatively smaller number of participants that meet the screening criteria for GAD in logistic regression analysis, may also lead to biased results [64]. Studies with larger samples that include more participants meeting the criteria for GAD would be required to address this problem. Lastly, as this study was cross-sectional, it was difficult to make causal inference regarding the predictive factors of mental health problems during the COVID-19 outbreak. Future studies may include a longitudinal design to account for this potential limitation.
In conclusion, the findings of our study demonstrated that the COVID 19 pandemic had a negative impact on the mental health of the participants. Predictive factors, such as younger age (20–29), female sex, currently being treated for medical or surgical disease, change in the amount of time spent on mobile device or computer after the COVID-19 pandemic, change in the household income were identified to be associated with mental health problems. It is important therefore to develop support strategies that target the most vulnerable population based on these factors. While the participants were willing to seek psychiatric treatment, fear of contacting COVID-19 while visiting the clinic deterred them. The participants were willing to utilize digital therapeutics if available, and even preferred this type of support compared to actually visiting a clinic. As such, it would only be rational to allocate more resource toward developing and implementing digital therapeutics, which may help improve mental health conditions during a pandemic.
Notes
Availability of Data and Material
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Jaeun Ahn. Data Curation: Manjae Kwon, Deokjong Lee, Jaeun Ahn. Formal analysis: Manjae Kwon. Investigation: all authors. Methodology: Young-Chul Jung, Jaeun Ahn. Project administration: Jaeun Ahn. Resources: Young-Chul Jung. Software: Young-Chul Jung. Supervision: Young-Chul Jung, Deokjong Lee. Validation: Young-Chul Jung, Deokjong Lee, Jaeun Ahn. Visualization: Manjae Kwon. Writing—original draft: Manjae Kwon. Writing—review & editing: Young-Chul Jung, Deokjong Lee, Jaeun Ahn.
Funding Statement
None


