1. Weiner RD, Reti IM. Key updates in the clinical application of electroconvulsive therapy. Int Rev Psychiatry 2017;29:54-62.


2. Lisanby SH. Electroconvulsive therapy for depression. N Engl J Med 2007;357:1939-1945.


3. Oudman E. Is electroconvulsive therapy (ECT) effective and safe for treatment of depression in dementia? A short review. J ECT 2012;28:34-38.

5. Wachtel LE, Shorter E, Fink M. Electroconvulsive therapy for self-injurious behaviour in autism spectrum disorders: recognizing catatonia is key. Curr Opin Psychiatry 2018;31:116-122.

6. Griesemer DA, Kellner CH, Beale MD, Smith GM. Electroconvulsive therapy for treatment of intractable seizures. Initial findings in two children. Neurology 1997;49:1389-1392.


7. Borisovskaya A, Bryson WC, Buchholz J, Samii A, Borson S. Electroconvulsive therapy for depression in Parkinsonâs disease: systematic review of evidence and recommendations. Neurodegener Dis Manag 2016;6:161-176.


8. Ueda S, Koyama K, Okubo Y. Marked improvement of psychotic symptoms after electroconvulsive therapy in Parkinson disease. J ECT 2010;26:111-115.


10. Narang P, Glowacki A, Lippmann S. Electroconvulsive therapy intervention for Parkinsonâs disease. Innov Clin Neurosci 2015;12:25-28.


11. Volkaerts L, Roels R, Bouckaert F. Motor function improvement after electroconvulsive therapy in a Parkinsonâs disease patient with deep brain stimulator. J ECT 2020;36:66-68.


12. Langston JW, Ballard P, Tetrud JW, Irwin I. Chronic parkinsonism in humans due to a product of meperidine-analog synthesis. Science 1983;219:979-980.


15. SundstrĂśm E, Fredriksson A, Archer T. Chronic neurochemical and behavioral changes in MPTP-lesioned C57BL/6 mice: a model for Parkinsonâs disease. Brain Res 1990;528:181-188.


16. Mori A, Ohashi S, Nakai M, Moriizumi T, Mitsumoto Y. Neural mechanisms underlying motor dysfunction as detected by the tail suspension test in MPTP-treated C57BL/6 mice. Neurosci Res 2005;51:265-274.


17. Moriguchi S, Yabuki Y, Fukunaga K. Reduced calcium/calmodulin-dependent protein kinase II activity in the hippocampus is associated with impaired cognitive function in MPTP-treated mice. J Neurochem 2012;120:541-551.


20. Poewe W. Non-motor symptoms in Parkinsonâs disease. Eur J Neurol 2008;15 Suppl 1:14-20.


21. Borroni B, Premi E, Formenti A, Turrone R, Alberici A, Cottini E, et al. Structural and functional imaging study in dementia with Lewy bodies and Parkinsonâs disease dementia. Parkinsonism Relat Disord 2015;21:1049-1055.


22. Tadaiesky MT, Dombrowski PA, Figueiredo CP, Cargnin-Ferreira E, Da Cunha C Takahashi RN. Emotional, cognitive and neurochemical alterations in a premotor stage model of Parkinsonâs disease. Neuroscience 2008;156:830-840.


23. Foltynie T, Goldberg TE, Lewis SG, Blackwell AD, Kolachana BS, Weinberger DR, et al. Planning ability in Parkinsonâs disease is influenced by the COMT val158met polymorphism. Mov Disord 2004;19:885-891.


24. Storvik M, Arguel MJ, Schmieder S, Delerue-Audegond A, Li Q, Qin C, et al. Genes regulated in MPTP-treated macaques and human Parkinsonâs disease suggest a common signature in prefrontal cortex. Neurobiol Dis 2010;38:386-394.


25. Segi-Nishida E. Exploration of new molecular mechanisms for antidepressant actions of electroconvulsive seizure. Biol Pharm Bull 2011;34:939-944.


30. Jackson-Lewis V, Jakowec M, Burke RE, Przedborski S. Time course and morphology of dopaminergic neuronal death caused by the neurotoxin 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine. Neurodegeneration 1995;4:257-269.


33. Kim SH, Yu HS, Park HG, Jeon WJ, Song JY, Kang UG, et al. Dose-dependent effect of intracerebroventricular injection of ouabain on the phosphorylation of the MEK1/2-ERK1/2-p90RSK pathway in the rat brain related to locomotor activity. Prog Neuropsychopharmacol Biol Psychiatry 2008;32:1637-1642.


34. Park HG, Yu HS, Park S, Ahn YM, Kim YS, Kim SH. Repeated treatment with electroconvulsive seizures induces HDAC2 expression and downregulation of NMDA receptor-related genes through histone deacetylation in the rat frontal cortex. Int J Neuropsychopharmacol 2014;17:1487-1500.


35. Eslamboli A, Romero-Ramos M, Burger C, Bjorklund T, Muzyczka N, Mandel RJ, et al. Long-term consequences of human alpha-synuclein overexpression in the primate ventral midbrain. Brain 2007;130:799-815.


36. Kuhn K, Wellen J, Link N, Maskri L, LĂźbbert H, Stichel CC. The mouse MPTP model: gene expression changes in dopaminergic neurons. Eur J Neurosci 2003;17:1-12.


37. Shimoji M, Zhang L, Mandir AS, Dawson VL, Dawson TM. Absence of inclusion body formation in the MPTP mouse model of Parkinsonâs disease. Brain Res Mol Brain Res 2005;134:103-108.


38. Saporito MS, Thomas BA, Scott RW. MPTP activates c-Jun NH(2)-terminal kinase (JNK) and its upstream regulatory kinase MKK4 in nigrostriatal neurons in vivo. J Neurochem 2000;75:1200-1208.


39. Robertson DC, Schmidt O, Ninkina N, Jones PA, Sharkey J, Buchman VL. Developmental loss and resistance to MPTP toxicity of dopaminergic neurones in substantia nigra pars compacta of gamma-synuclein, alpha-synuclein and double alpha/gamma-synuclein null mutant mice. J Neurochem 2004;89:1126-1136.


41. Carling D. The AMP-activated protein kinase cascade-a unifying system for energy control. Trends Biochem Sci 2004;29:18-24.


43. Kuroyanagi H, Yan J, Seki N, Yamanouchi Y, Suzuki Y, Takano T, et al. Human ULK1, a novel serine/threonine kinase related to UNC-51 kinase of Caenorhabditis elegans: cDNA cloning, expression, and chromosomal assignment. Genomics 1998;51:76-85.


47. Inoki K, Zhu T, Guan KL. TSC2 mediates cellular energy response to control cell growth and survival. Cell 2003;115:577-590.


49. Pullen N, Dennis PB, Andjelkovic M, Dufner A, Kozma SC, Hemmings BA, et al. Phosphorylation and activation of p70s6k by PDK1. Science 1998;279:707-710.


51. Faber R, Trimble MR. Electroconvulsive therapy in Parkinsonâs disease and other movement disorders. Mov Disord 1991;6:293-303.


54. Cousineau J, Plateau V, Baufreton J, Le Bon- JĂŠgo M. Dopaminergic modulation of primary motor cortex: from cellular and synaptic mechanisms underlying motor learning to cognitive symptoms in Parkinsonâs disease. Neurobiol Dis 2022;167:105674


57. Pupyshev AB, Tikhonova MA, Akopyan AA, Tenditnik MV, Dubrovina NI, Korolenko TA. Therapeutic activation of autophagy by combined treatment with rapamycin and trehalose in a mouse MPTP-induced model of Parkinsonâs disease. Pharmacol Biochem Behav 2019;177:1-11.


58. Zhu J, Gao W, Shan X, Wang C, Wang H, Shao Z, et al. Apelin-36 mediates neuroprotective effects by regulating oxidative stress, autophagy and apoptosis in MPTP-induced Parkinsonâs disease model mice. Brain Res 2020;1726:146493


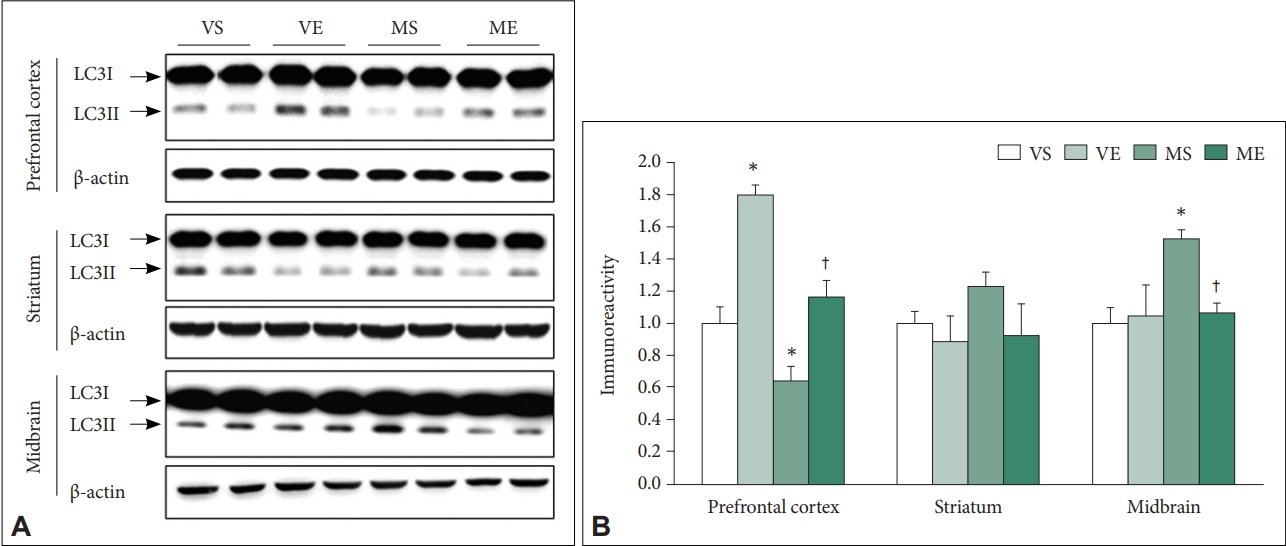
60. Mizushima N, Yoshimori T. How to interpret LC3 immunoblotting. Autophagy 2007;3:542-545.


61. Poels J, SpasiÄ MR, Callaerts P, Norga KK. Expanding roles for AMP-activated protein kinase in neuronal survival and autophagy. Bioessays 2009;31:944-952.


64. Madsen TM, Treschow A, Bengzon J, Bolwig TG, Lindvall O, TingstrĂśm A. Increased neurogenesis in a model of electroconvulsive therapy. Biol Psychiatry 2000;47:1043-1049.


65. Kim Y, Seo MS, Kang UG, Yoon SC, Ahn YM, Kim YS, et al. Activation of Cdk2-pRB-E2F1 cell cycle pathway by repeated electroconvulsive shock in the rat frontal cortex. Biol Psychiatry 2005;57:107-109.


66. Kang UG, Koo YJ, Jeon WJ, Park DB, Juhnn YS, Park JB, et al. Activation of extracellular signal-regulated kinase signaling by chronic electroconvulsive shock in the rat frontal cortex. Psychiatry Res 2006;145:75-78.